Written By Avery F.
Before having my children, I read everything I could get my hands on about being a mom. I wanted to be prepared and to be the best mom I could! But nobody warned me about what could happen to my mental health. Nobody talked to me about postpartum depression.
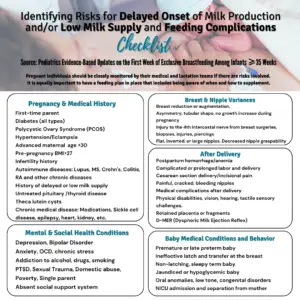
Did you know postpartum depression/mood disorders are the most common complication after childbirth for at least the first year? Suicide is one of the leading causes of death in the first year postpartum. We need to start taking maternal mental health seriously. The idea that breastfeeding prevents PPD is a myth. It can happen to any mom, no matter how she feeds her baby, and each mom can experience it very differently. We can SAVE lives if we DO talk about it!
When I first wrote this blog post, I was blown away by how many mothers related to my breastfeeding story. So many women reached out to let me know I wasn’t alone and shared nearly identical stories. This made me both relieved and very sad that this mental health side of breastfeeding isn’t talked about enough. I don’t understand why so many people act like it doesn’t happen and don’t talk about it.
I was just as equally shocked to see how many mothers thought that I should have kept breastfeeding anyway, even if it meant resenting my son and being nothing more than a food source and a shell of a person. Many lactivists picked my story apart, from accusing me of being selfish to thinking I didn’t have enough breastfeeding support or encouragement. But their accusations were false. I had more than enough breastfeeding support but very little support for switching to formula when I knew it was best for my own mental health and for my son. I can’t fathom telling a mom she’d better breastfeed or might as well be dead.

I’m not against breastfeeding. I successfully breastfed my second baby for almost a year! But I don’t believe in breastfeeding at all costs, especially at the expense of the mother’s health, and that includes her mental health. A mother’s mental and emotional health is just as important as her baby’s health. Not every mom gets that oxytocin-induced happy breastfeeding experience. Sometimes, it’s the opposite; those moms also need different support and respect.
I was four months postpartum, and I was suffering from postpartum depression(PPD). I began suffering from PPD almost immediately after birth. I brushed it off as “baby blues,” but it never went away. I slowly got worse as the weeks went by, and I finally admitted to myself that I had PPD. I was so ashamed and embarrassed. I didn’t want anyone to know. The tipping point was a combination of things. I was desperately trying to avoid medication or therapy due to the stigma surrounding them, but all the ‘natural options’ I tried were not working at all. (And I tried everything I could get my hands on. Supplements, oils, exercise, and religion.)
Breastfeeding/pumping was such a struggle for me that I found myself consumed by thoughts of disappearing every time I fed him. The people I admitted this to basically said that all that mattered was that he was getting my milk and not formula, which increased my guilt for wanting to stop. I hated myself for it. I didn’t have that magical bond everyone discussed, and I was sure it meant I was a terrible mother. I felt like a food source and nothing more, but it felt like it was the only thing I could do right since I seemed to be failing at everything else. I was not myself, and I knew that burdened my poor husband. It hurt my heart, but I didn’t know how to stop it. Everything just seemed to get worse. I felt stuck in a dark pit in the back of my mind, but the walls kept getting higher and harder to climb. I vividly remember being at work and writing down my thoughts of wanting to disappear/die on a scrap piece of paper. A co-worker found it while I was away from my desk, and all she said was, “I’m really disappointed in you.” At that point, I became thoroughly convinced that my husband and son would be better off without me. I’d be out of their lives, and they could move on happily without me. It makes me sick to say it now, but I thought they’d be much happier if I were gone.
I remember being in the basement bathroom, looking up at the tiny window, and thinking that would be the last thing I saw before I died. I was ready to go. My husband came home and found me at the right moment, saving my life. That moment marked my rock bottom, but it was also the turning point that led me to seek the psychological support I was so desperate for.
My fantastic doctor mentioned to me that formula feeding for my mental health did not equal failure. I didn’t have to keep putting myself through that, and that my sweet boy would be just fine on formula, and It would give me a chance to recover. I started the medication. It took a few weeks to work fully, but my husband noticed a change in me before I did. One day, he smiled at me and said, “It’s nice to have you back!”
But it took me longer to switch to the formula. The guilt I felt over it was crippling. Even though I really wanted to stop, I falsely worried I’d be dooming him for life and ruining his future. And I feared the judgment of my “breast is best” friends. Every day, I’d think, “Today is the day we try formula!” But guilt ate at me every time.
One day, I decided to do it. I felt so guilty preparing that bottle. I cried. But during that feeding, it was the first time I looked at my baby boy while feeding him. I made eye contact, stroked his red hair, and sang to him! I wanted to snuggle him afterward. I had no bitter feelings toward him or the feeding, no wishing it was over, no dreading the next feeding. He smiled at me, and my heart melted. It was a real bonding moment, and that one bottle took a huge weight off my shoulders. For me, that was the first day I started to feel relief and feel hopeful. I knew he’d be ok and happy on formula, and I’d be able to be the happy and healthy mommy that he deserved. My mental health slowly improved over three months, and I finally reached a point where I felt back to myself. I had a few hard days here and there, but soon, there were more good than bad days.
If you are a mom who is struggling, do whatever you need to do to be okay! There is help, support, and resources available to you. Please join our Facebook private support group,where you will find the best shame-free support available! If you feel that breastfeeding helps your postpartum depression, then keep doing it, but get extra help with PPD/A while doing so. If you feel like breastfeeding is making your postpartum depression worse, it’s okay to switch to formula if that is what you want. I say that because I desperately wish someone had said that to me when I was struggling instead of trying to push and guilt me into something that I hated. If you want to combo feed to give yourself a break from exclusive breastfeeding, you can do that, too!
You’re not alone:The National Maternal Mental Health Hotline (1-833-TLC-MAMA | 1-833-852-6262) is free, confidential, and available 24/7 to help new parents and loved ones.

About Avery: I am a 25-year-old mom of two boys and a little girl on the way. My amazing husband is a firefighter/EMT, and we have been happily married for seven years. I’m a hobby photographer and have a deep love of books. Before having my children, I read everything I could get my hands on about being a mom. I wanted to be prepared and to be the best mom I could! But nobody warned me about what could happen to my mental health. Nobody talked to me about postpartum depression. I wish it were talked about more. After recovering from my suicide attempt and PPD, I learned as much as I could about perinatal mood and anxiety disorders. Since then, I’ve tried to be an advocate for maternal mental health awareness so hopefully, other women won’t have to experience what I did. I volunteered as a Warrior Mom Ambassador with Postpartum Progress and co-led two Climb Out of the Darkness events in my community. I am honored to join the Fed Is Best Foundation to raise maternal mental health awareness about infant feeding choices -Avery F.
Please remember this:

Support and outcomes for mental health cannot be overstated, and they are not currently incorporated into breastfeeding policies. Each family decides with their healthcare professional which type of milk and feeding method will nourish their baby in the best way possible, given their individualized needs.
Our Newly Published transformative Book Teaches Parents How to Prioritize their Mental well-being.

Our transformative bookpromises to navigate the intricate landscape of infant feeding choices, empowering parents with knowledge and judgment-free support. Our highly anticipated book will reshape the conversation around infant nutrition, offering a comprehensive, science-backed, and inclusive perspective on the myriad ways families can safely and optimally nourish their babies. Click here to purchase our newly published, groundbreaking book!
We recognize the pressure to breastfeed from healthcare providers is associated with the onset of mental health conditions. According to research findings, the pressure to breastfeed exclusively is leading to depression, anxiety, disordered eating, and other mental health conditions. We advocate for fundamental change in educating and supporting breastfeeding without exerting pressure. We do this every day at work and in our support group.
Click hereformental health outcomesand infant feeding goals.
Educational blog resources and stories
It’s World Breastfeeding Week: What Sets Apart The ‘Fed Is Best’ Message From The ‘Breast Is Best’ Message? – Fed Is Best Foundation
The Fed Is Best Book: Protecting Infants and Empowering Choices

 My husband and I cried a lot during the first 24 hours at home. We fought to wake our sleepy newborn up, but we were rarely successful, and when we were, we couldn’t get him to eat. I kept on refusing to allow my husband to give our son any formula because I didn’t want it to ruin our breastfeeding relationship. We went to his newborn appointment when he was four days old. I knew at that point things weren’t going well but wasn’t prepared for the realities we were about to face. Our son had lost 13% of his body weight, he was hypothermic with a body temperature of 94.9, he was hypoglycemic, and had lost his reflexes. Our pediatrician looked at us with very sad eyes and kindly but firmly, explained our son was very sick and needed to eat now.
My husband and I cried a lot during the first 24 hours at home. We fought to wake our sleepy newborn up, but we were rarely successful, and when we were, we couldn’t get him to eat. I kept on refusing to allow my husband to give our son any formula because I didn’t want it to ruin our breastfeeding relationship. We went to his newborn appointment when he was four days old. I knew at that point things weren’t going well but wasn’t prepared for the realities we were about to face. Our son had lost 13% of his body weight, he was hypothermic with a body temperature of 94.9, he was hypoglycemic, and had lost his reflexes. Our pediatrician looked at us with very sad eyes and kindly but firmly, explained our son was very sick and needed to eat now.