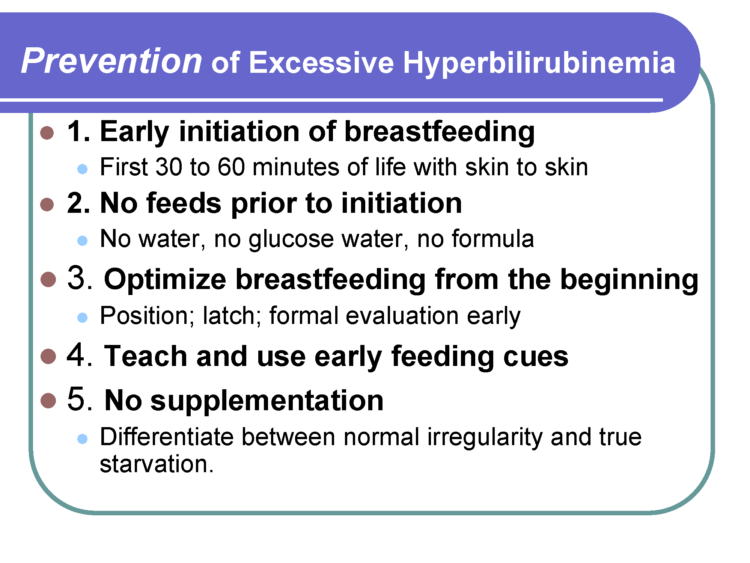
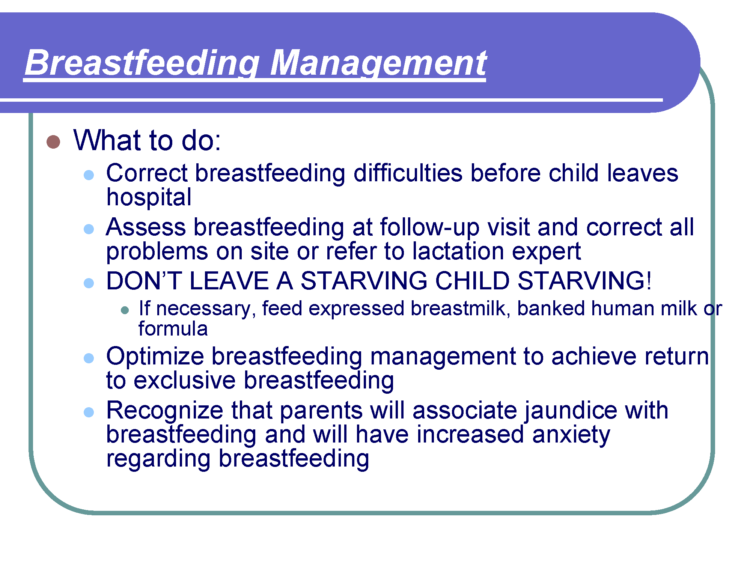
As a first-time mom, I braced myself for the worst but when my water broke that morning, I was super calm. At the hospital, I had some IV pain medications, but labor went really smoothly and quick. A little after my baby was born I decided to try and feed him, not really knowing what I was doing or supposed to do. The LC came and tried to help him to latch. He didn’t really want to latch, so she had me hand express some colostrum and spoon feed it to him. She warned me not to use a pump (Why I don’t know) and that the small drops I was expressing were enough for him. So, he had drops of colostrum all day.
The second night he was crying all night long. I kept telling the nurses that I didn’t think he was getting anything from me, because he wanted to nurse non-stop and would cry as soon as he was off my breast. But, I was told his crying was normal. Looking at my feeding log I got maybe 2 hours of sleep. I was exhausted and very concerned.