By Tiffany, Fed is Best Mom and Advocate
When I was pregnant I had already decided to formula feed my baby. My family (even some cousins) thought it was strange and tried to talk me out of it, and I had family delete me on social media because we disagreed on this topic. My midwife was amazing and encouraged me to consider breastfeeding, but if I didn’t want to, that was perfectly okay. By the time I was 30 weeks pregnant, I changed my mind and wanted to try to see if breastfeeding would work for us.
I delivered after 2 days of labor, 2 hours of pushing followed by 5 hours of waiting then some more pushes, a vacuum, and then some panicked doctors who rushed me to an emergency C-section at 41 weeks plus 2 days. My daughter was immediately sent to the NICU from the stressful delivery. I saw my baby following the surgery about 6 hours later and she was being tube fed. The next evening, they let me begin to try to feed her which went wonderfully! She latched, it didn’t hurt, but she was still hungry. My colostrum came in quickly, followed by my milk within 3 days in full.
But something was off. I ended up getting ill every time I breastfed her. I would get a fever, chills, and extremely tired every time I nursed her. I would have to sleep about 6 hours to feel normal again. The NICU asked if during the times I was sleeping they could supplement with formula. I said of course! If she needs fed, we feed her! Putting essential vitamins and nutrients in her tummy is what needed to happen. Over the course of her five day NICU stay, she breastfed, got breast milk from a bottle, and was supplemented when there wasn’t enough breast milk. I believe that supplementing her was what made her healthy and strong enough to recover and come home with us.
I was “encouraged” to keep pumping, so she could have “liquid gold” and that led to having no time to do anything. I was eating once a day and drinking very little. I became so ill, my husband spent multiple nights feeding her because I was shaking and couldn’t move due to weakness. I was not healthy at all. I couldn’t be a mother to her; I hated being a mother to her at that time; I regretted her. It was awful. Finally, at 3 weeks I decided I had enough and my health and sanity was crucial for my daughter to have the mother she deserves. I stopped pumping and switched her to formula completely and never touched that pump again.
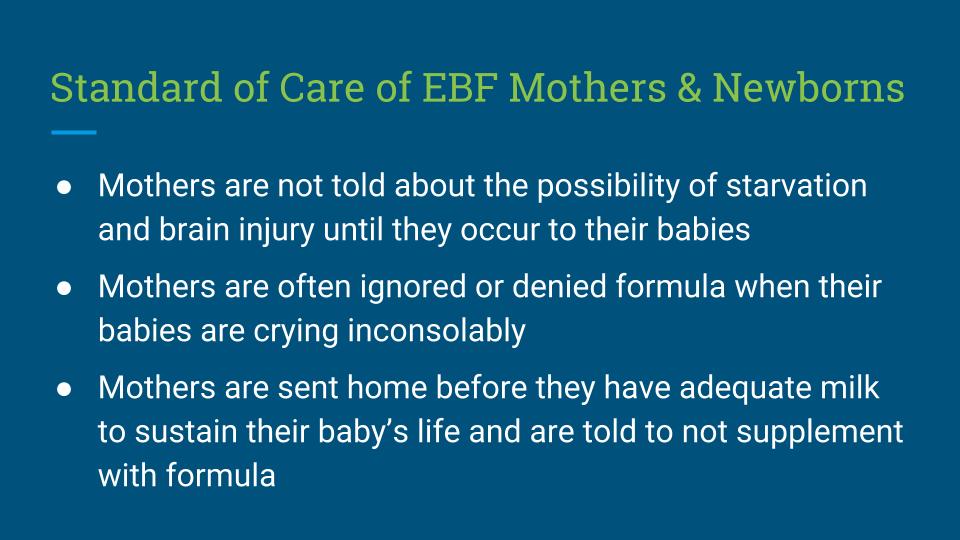
This was the Best. Decision. Ever. She continued to thrive, continued to eat just the same, and my body and mind healed. I loved feeding time with her and that magical bonding of looking at her, each time, was so very special to me. But people were mad! People argued that I wasn’t doing what was best for her, only for me. People continued to judge and spew hate about making a deeply personal choice that worked best for me. This is when I found the Fed Is Best Foundation. In their support group, which is private to keep it safe, I found the Foundation encouraged breastfeeding, pumping, supplementing, tube feeding, and formula feeding! They encouraged putting baby’s and mother’s health above an obsession to breastfeed. I fell in love with the information and the people surrounding this movement. I would come to find mothers in similar predicaments were being “encouraged,” but really, they needed a solution – not encouragement to continue something that wasn’t working for them. I brought many struggling mothers to our private support group. I continue to advocate for #fedisbest because until every mother can achieve the goal of a thriving, healthy baby in the health care system by whatever form of feeding suits their own family and babies the best, we have to work to make changes!

 Meet Tiffany, a new mama to her sweet baby girl and both are thriving and celebrating her first birthday!
Meet Tiffany, a new mama to her sweet baby girl and both are thriving and celebrating her first birthday!
Do you need genuine help and support for yourself and your baby? Please send us a message on our Facebook page.
HOW YOU CAN SUPPORT FED IS BEST
There are many ways you can support the mission of the Fed is Best Foundation. Please consider contributing in the following ways:
- Join the Fed is Best Volunteer group to help us reach Obstetric Health Providers to advocate for counseling of new mothers on the importance of safe infant feeding.
- Share the stories and the message of the Fed is Best Foundation through word-of-mouth, by posting on your social media page and by sending our resources to expectant moms that you know. Share the Fed is Best campaign letter with everyone you know.
- Print out our letter to obstetric providers and mail them to your local obstetricians, midwives, family practitioners who provide obstetric care and hospitals
- Write your local elected officials about what is happening to newborn babies in hospitals and ask for legal protection of newborn babies from underfeeding and of mother’s rights to honest informed consent on the risks of insufficient feeding of breastfed babies.
- Make a donation to the Fed is Best Foundation. We are using funds from donations to cover the cost of our website, our social media ads, our printing and mailing costs to reach health providers and hospitals. We do not accept donations from breast- or formula-feeding companies and 100% of your donations go toward these operational costs. All the work of the Foundation is achieved via the pro bono and volunteer work of its supporters.



 Meet Tiffany, a new mama to her sweet baby girl and both are thriving and celebrating her first birthday!
Meet Tiffany, a new mama to her sweet baby girl and both are thriving and celebrating her first birthday!