by Jillian Johnson with commentary from Dr. Christie del Castillo-Hegyi
Landon would be five today if he were still alive. It’s a very hard birthday–five. It’s a milestone birthday. Most kiddos would be starting kindergarten at this age. But not my little guy. I wanted to share for a long time about what happened to Landon, but I always feared what others would say and how I’d be judged. But I want people to know how much deeper the pain gets.
I share his story in hopes that no other family ever experiences the loss that we have.
Jarrod and I wanted what was best for Landon, as every parent does for their child. We took all of the classes. Bought and read all of the books. We were ready! Or so we thought….every class and book was geared toward breastfeeding and how it’s so important if you want a healthy child. Landon was born in a “Baby-Friendly” hospital. (What this means is everything is geared toward breastfeeding. Unless you’d had a breast augmentation or cancer or some serious medical reason as to why you couldn’t breastfeed, your baby would not be given formula unless the pediatrician wrote a prescription.)


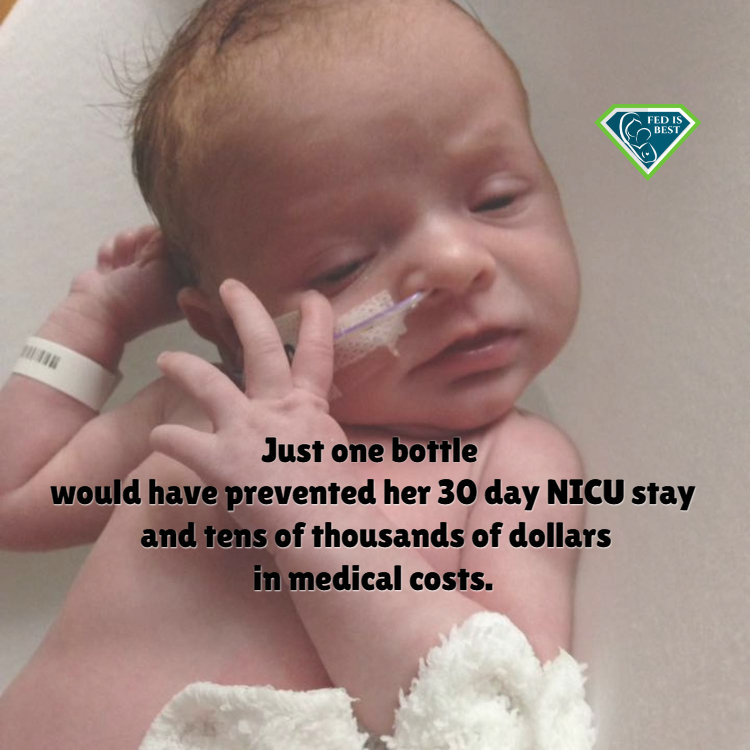 On day two a nurse comes in and tells me my baby is hungry and I’m not making milk…but by then it was too late. She lost almost a pound over night and she was too weak to take formula orally. We were rushed by ambulance to a NICU unit one hour away from where I delivered her.
On day two a nurse comes in and tells me my baby is hungry and I’m not making milk…but by then it was too late. She lost almost a pound over night and she was too weak to take formula orally. We were rushed by ambulance to a NICU unit one hour away from where I delivered her. Today, she is 3 months old and thriving. #FedIsBest
Today, she is 3 months old and thriving. #FedIsBest
 My beautiful boy was born on July 13, 2016 at 8:33 p.m. in a Baby Friendly Hospital Initiative (BFHI) certified hospital in Florida. I had every intention of breastfeeding my child, heck, I even wanted to continue beyond age one. I took classes for breastfeeding, read everything I could get my hands on, and I felt completely ready and excited to start this journey with my little one.
My beautiful boy was born on July 13, 2016 at 8:33 p.m. in a Baby Friendly Hospital Initiative (BFHI) certified hospital in Florida. I had every intention of breastfeeding my child, heck, I even wanted to continue beyond age one. I took classes for breastfeeding, read everything I could get my hands on, and I felt completely ready and excited to start this journey with my little one.
