By Christie del Castillo-Hegyi, M.D., Co-Founder of the Fed is Best Foundation
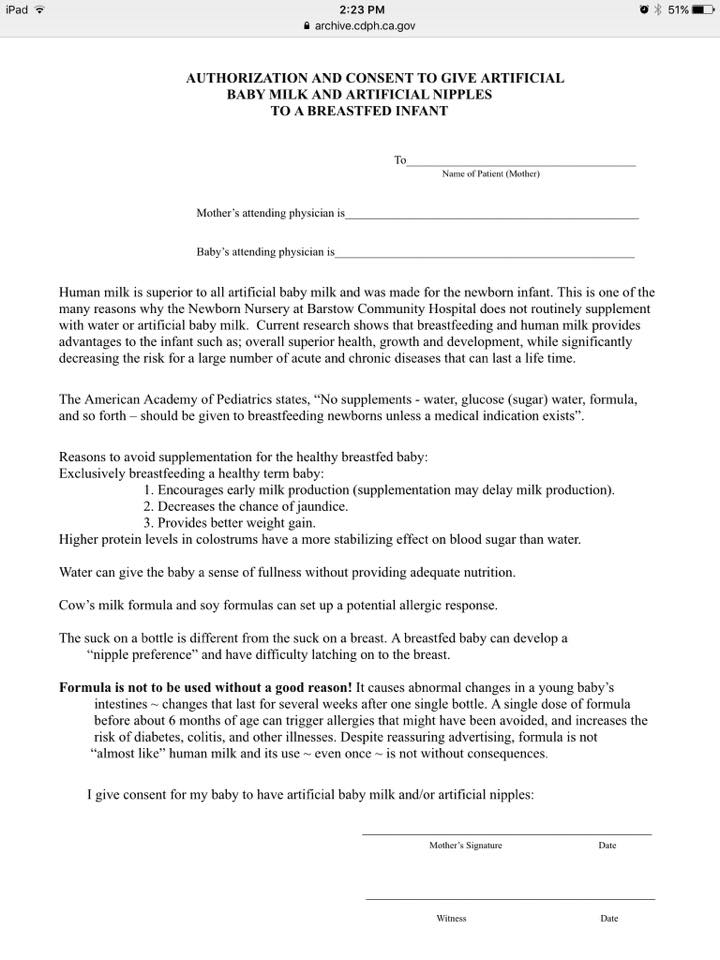
The primary reason why newborns experience starvation-related complications every single day as a result of the Baby-Friendly protocol is because the complications associated with the protocol are hidden from mothers who seek to breastfeed. The primary objective of the Baby-Friendly Hospital Initiative is high exclusive breastfeeding at discharge. Unfortunately, because the rates of insufficient breast milk and delayed lactogenesis II are high among mothers, the necessary consequences of hospital policies that seek high EBF at discharge rates are higher starvation-related complications like hyperbilirubinemia, hypernatremia, dehydration and hypoglycemia, all of which can cause newborn brain injury and permanent disability. Below is an example of the way mothers are made to fear formula supplementation while the risks of NOT supplementing are hidden. This is a waiver form published on the California Department of Public Health Website to provide an example of a model formula waiver form for hospitals.