A Review of the Literature by Dr. Christie del Castillo-Hegyi
We have received some questions here at the Fed is Best Foundation regarding the science of infant feeding and preventing accidental newborn starvation from insufficient breast milk intake. Some have said there is no evidence that insufficient milk intake in newborns causes brain injury, developmental delays and disabilities. We’d like to take the opportunity to open up a discussion on this very important topic.
The general body of medical and scientific literature largely supports that babies who are not fed enough calories and fluid through breastfeeding can develop excessive jaundice, severe dehydration and hypoglycemia – all complications that can cause brain injury if not corrected. This isn’t exclusive to humans. In fact, the basic rule of nature is that no creature, particularly mammals, can live without food.
We believe it is critically important to educate and support mothers in safe feeding practices. As we are pro-feeding, that means we’re not attached to one form of feeding versus another – as long as it is clinically safe and keeps a baby safe from underfeeding and what can be tragic outcomes. We talk a lot in this society about all the benefits and wonderful things associated with various forms of feeding, but we don’t often shed light on the importance of putting basic infant nutritional needs and hunger at the forefront of that discussion.
Specifically, it’s undeniable that babies can suffer greatly when they’re underfed, just like any human would, and it can be much more difficult to identify this suffering for these tiny patients outside of a clinical setting. As clinicians with practical experience in this arena, we understand the challenges that families face . It is why it is so important to us to educate others about the most severe consequences of starvation, such as permanent brain injury. We believe it is dangerous for health providers to guide breastfeeding without awareness of the irreversible consequences of a child not being fed enough, plain and simple.
Mothers are often reassured that this will not happen to their baby, oftentimes by non-clinical or medically trained staff, or alternatively, they are not informed of the risks at all so they are not able to make a fully informed feeding decision. However, hospitalization for excessive jaundice, dehydration and hypoglycemia from insufficient early exclusive breastfeeding are among the most common reasons for newborn hospitalization and re-hospitalization in the world. Our bottom line is that we believe in SAFE breastfeeding for EVERY newborn, SAFE milk bank or SAFE formula feeding for every newborn where it’s more appropriate – and NOT breastfeeding at all costs. Here at The Fed Is Best Foundation, we use the scientific literature available to learn where those safe limits and thresholds are. Given that, we would like to provide you this supporting evidence (studies linked in red):
ARTICLE 1: SYMPTOMATIC HYPOGLYCEMIA CAUSING BRAIN INJURY IN A TERM BREASTFED NEWBORN FOLLOWING EARLY DISCHARGE
A term (38 week 2 day) appropriate-for-gestational-age baby (2.5 kg or 5 lbs 8 oz) was born by normal vaginal delivery to a first-time mother. The labor, delivery and post-delivery course were normal. The baby had Apgar scores of 8 and 9 at 1 and 5 minutes respectively. The baby was discharged at 24 hours of life exclusively breastfeeding. The baby was brought to the pediatric emergency room at day 3 (60 hrs) of life with complaints of poor feeding since discharge, excessive crying and staring look for 3 hours. In the hospital, generalized seizures were observed. The blood glucose was 20 mg/dL. Weight on readmission was 2.275 kg (weight loss of 9% at 60 hrs). Baby was resuscitated with a bolus of 2 mL/kg of 10% dextrose, which aborted the seizure, followed by a glucose infusion. This was continued for 24 hours to 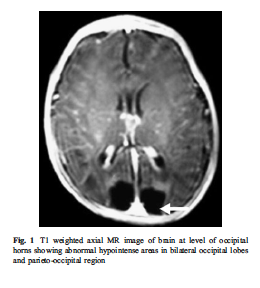 maintain a normal glucose of 60-90 mg/dL. The blood electrolytes were normal and the baby’s bilirubin was 8.2 mg/dL. Ultrasound of the head at that time was normal (brain injury usually takes a week to appear on ultrasound). The sepsis evaluation including blood cultures and cerebrospinal fluid were within normal limits. Glucose infusion was tapered as oral supplementation was started the next day and baby was discharged on day 10 of life on established breast feeds. An MRI brain was obtained at 1 month and showed loss of brain tissue in the occipital lobes and parieto-occipital regions.
maintain a normal glucose of 60-90 mg/dL. The blood electrolytes were normal and the baby’s bilirubin was 8.2 mg/dL. Ultrasound of the head at that time was normal (brain injury usually takes a week to appear on ultrasound). The sepsis evaluation including blood cultures and cerebrospinal fluid were within normal limits. Glucose infusion was tapered as oral supplementation was started the next day and baby was discharged on day 10 of life on established breast feeds. An MRI brain was obtained at 1 month and showed loss of brain tissue in the occipital lobes and parieto-occipital regions.
ARTICLE 2: LATE-ONSET HYPOGLYCEMIA IN TERM NEWBORNS WITH POOR BREASTFEEDING
A 39 1/7-week age boy was born via vaginal delivery at 2905 g (6 lbs 6 oz) to a first-time mother who was primarily breastfeeding but had reported supplementing with formula intermittently. The amount of formula used, mother’s change in breasts during pregnancy and after delivery, and infant’s ability to feed were not clearly documented and/or reported in the medical record. He presented to his primary medical doctor on day of life 3 for a normal newborn well-child check. On day of life 4, he was seen by a home health nurse and reportedly could not feed with a syringe due to lethargy and was referred to CCHMC emergency department, where his weight was 2600 g (5 lbs 8 oz), decreased 10.5% from birth. Glucose was measured to be 20 mg/dL. He was given an intravenous 2-mL/kg bolus of dextrose 10% in water. He had a seizure, which was treated with 1 dose of lorazepam. During his hospital course, he received phenobarbital for seizure prophylaxis. Magnetic resonance imaging (MRI) of the brain showed extensive areas of brain injury involving the bilateral parietal and occipital lobes with subtle restricted diffusion in the right frontal and temporal lobes. He was discharged from the hospital on maintenance phenobarbital (seizure medication).
Other babies described on Table 1 of the article.
1. 38 week 3 day male, vaginally-delivered, 2637 grams, lost 7.3% of birth weight, first-born, exclusive breast milk feeding at 4 days of life was lethargic, poorly feeding and had a seizure. His glucose was 20 mg/dL. MRI showed severe injury to the posterior one-third of the brain.
2.A 38 week vaginally-delivered baby weighing 2634 grams at birth, first-born child, lost 6.6% of their weight, was breastfed exclusively found at day 3 of life lethargic, poorly feeding with no urine output for 12 hours. The glucose was 36. No MRI was done.
3. A 39 week vaginally-delivered baby weighing 3989 grams at birth, lost 9.1%, first-born child, breastfed exclusively was found on day 2 of life twitching in the upper extremities with a glucose of 28 mg/dL. EEG was normal. No MRI was done.
4. A 40 week and 1 day old vaginally-delivered baby born 3288 grams and lost 4.2%, breastfed exclusively found at day 3 of life poorly feeding, shallow breathing and with tremors. The baby developed a seizure was found to have a glucose of 13 mg/dL. Brain MRI showed brain injury to the parietal and both sides of the occipital lobes
5. 37 weeks an 3 day vaginally delivered baby weighing 3525 with 16% weight loss, exclusively breastfed found at day 3 of life lethargic, unresponsive and not breathing with a glucose of less than 20. The baby had a seizure and on MRI was found to have diffuse brain injury involving the frontal, parietal and occipital lobes.
6. A 38 week 5 day old vaginally delivered baby weighing 2525 with 0% weight loss, first-born, exclusively breastfed found at day 3 blue, lethargic and poorly feeding. Was found to have a glucose of 20 mg/dL and had a seizure. Brain MRI showed brain injury to both parietal, temporal and occipital lobes.
7. 40 week vaginally delivered baby 3550 g, lost 7%, breastfed with some formula supplementation found at 4 days of life lethargic, poorly feeding with a glucose of 23. No MRI done.
8. 39 week 4 day cesarean-delivered baby 3015 g, lost 7.1%, exclusively breastfed, found at 2 days of life not breathing and weak, found to have a glucose of 8 mg/dL. MRI was normal.
9. 40 week vaginally-delivered baby born 3100 g, lost 5.5%, exclusively breastfed found at day 2 of life not breathing at home. He had a glucose of 13 mg/dL. No MRI done.
10. 37 week and 5 day cesarean-delivered baby weighing 2807 g, lost 4.5%, exclusively breastfed found at 5 days of life with low body temperature at pediatrician’s office. Had a glucose of 35 mg/dL. No MRI was done.
Nine of the 11 were first-time mothers. 9 of 11 lost less than 10% of their birth weight. 5 of the 11 were exclusively breastfeeding without any expressed milk provided. An additional 4 of the 11 were directly breastfeeding and also receiving expressed breast milk via syringe or a bottle, and 2 more were receiving formula in addition to direct breastfeeding. The volume of the supplementation of formula and/or expressed breast milk was not reported in the medical records. Six patients had an MRI obtained and only 1 was read as normal. Seven patients had follow-up available in their medical charts. Four of those 7 patients continue to have neurologic sequelae as a result of their hypoglycemic event. As of their most recent appointments, two of the patients are still on antiepileptic medication, one completed a phenobarbital wean after discharge but continues to have generalized hypotonia (weakness), and one continues to have visual impairment. Of the 2 who remain on medication, 1 continues to have feeding difficulties and is followed by speech therapy. (read the rest of the article here).
ARTICLE 3: PERMANENT BRAIN DAMAGE FROM HYPERNATREMIC DEHYDRATION IN BREASTFED INFANTS: PATIENT REPORTS
Patient 1: A 4073 g term first-born infant was delivered by vacuum-assisted vaginal delivery. The baby had a weak cry and was floppy but responded readily to blow-by oxygen. Glucose checks measured the first 10 hours were 33-57 then above stayed 40 mg/dL. The mother was seen by a lactation consultant on day 2 of life and the baby was having trouble staying latched on. On day 4, the baby was noted to have a normal feeding pattern and lost 10% of the birth weight. By day 7 of life, when seen by nurse practitioner, he had lost 14%. On day 8, the mother became concerned when he did not feed at all. She called the advice line and a physician advised her that she did not need to bring the baby to the emergency room. The next day, the baby was found severely dehydrated and lethargic. The baby was thin, emaciated, lethargic with dry lips and mouth, sunken eyes and absent tears. The baby was hypernatremic (higher concentration of blood sodium due to severe dehydration) with a sodium of 164 mEq/L (normal 135-145). 12 hours after admission, the baby had a seizure. A brain MRI was done and showed clotting in the veins of the brain. The follow-up brain MRI at 13 months old showed abnormalities in the white matter and loss of brain tissue matter around the ventricles. At age 4, the child had a seizure disorder, delayed language development, was unable to walk or stand and had right hand weakness.
Patient 2: A term baby was born by emergency cesarean section for fetal distress and acidosis weighing 2914 g. He appeared normal at birth and had a 5 minute Apgar score of 9. He did not nurse well. On day 2, he had tremors of his arms. He was discharged on day 3. Late that evening, the mother called 911 because the baby appeared blue, which luckily resolved on its own and the vitals signs were found to be normal. On day 4, the mother called the nurse advice hotline because she found her baby lethargic, not feeding and sleeping all the time; she was given advice on nursing techniques and reassured. She called multiple times on day 5 and was not seen until early afternoon on day 6. The baby was severely hypoglycemic (1 mg/dL) and severely dehydrated and hypernatremic (158 mEq/L). A CT scan showed encephalomalacia (brain injury). At 4 months of age, he developed infantile spasms (10-15 times daily) and his EEG showed seizure activity. CT scan showed loss of brain tissue and brain injury in the left occipital lobe. MRI brain at 1 year of age showed injury to the occipital cortex, parasagittal cortex, and the white matter consistent with ischemic injury. At 7 years of age, he had a few seizures daily even with seizure medication, was able to walk with a wide-based gait but could not feed himself or communicate. He had minimal vision and remained in diapers.
ARTICLE 4: LIFE-THREATENING HYPERNATREMIC DEHYDRATION IN BREASTFED BABIES
Five babies developed life-threatening hypernatremic dehydration due to inadequate breast milk intake. All were born healthy from normal pregnancies and deliveries and were all exclusively breastfed. They were regularly assessed by their midwives and general practitioners and all were assured their babies were feeding adequately and did not need to be weighed. The babies returned to the hospital profoundly dehydrated with cold extremities. Two newborns produced no urine but the others continued to pass urine despite severe dehydration. All the babies had severe hypernatremic dehydration and acute renal failure. Three newborns had extensive blood clots in their blood vessels requiring heparin treatment. The babies were followed up at 11-30 months and appeared to have met their developmental milestones but had no follow-up MRI or formal developmental testing.
ARTICLE 5: HYPERNATREMIC DEHYDRATION DUE TO LACTATION FAILURE IN AN EXCLUSIVELY BREASTFED NEONATE
A 13-day-old exclusively breastfed newborn, admitted with fever, poor feeding, lethargy and decreased urine output. She was born 3100 g, discharged at day 3 exclusively breastfeeding. The mother had a history of lactation failure. The baby was ill-appearing, irritable, lethargic and moderate dehydration. Her weight was 2200 g with a weight loss of 29%. The heart rate 110/min and pulses were weak. Fluid resuscitation was started. The baby had two episodes of convulsions an hour after admission and was started on seizure medications. The laboratory data was consistent with severe hypernatremia with kidney failure (sodium 220 mEq/dL). The white blood cell count was elevated (36,500) but the blood culture, urine culture and fungal culture showed no growth of organisms. The baby had to be placed on mechanical ventilation for shallow respirations and decreased consciousness. Dialysis was started for renal failure. The baby’s electrolyte abnormalities were eventually corrected with fluids and breast milk from the milk bank. No MRI was obtained and there was no long-term follow-up.
ARTICLE 6: STUDY OF ASYMPTOMATIC HYPOGLYCEMIA IN FULL TERM EXCLUSIVELY BREASTFED NEONATES (NEWBORNS) IN THE FIRST 48 HOURS OF LIFE
This was a study of 100 newborns that were healthy, term, all exclusively breastfed per the Baby-Friendly Hospital Initiative protocol. All roomed in with their mothers and had good sucking reflex and latching and had a normal newborn course. They defined hypoglycemia as < 40 mg/dL and checked their blood glucose at 1, 6, 24 and 48 hours of life. Overall, 10% of the newborns were hypoglycemic and all of the episodes were recorded at 1 hour and 6 hours of life. Amongst the first-born babies, 23% were hypoglycemic. There was no difference in rates of hypoglycemia between the vaginally-delivered and cesarean-delivered babies. Breastfeeding was initiated as soon as possible. There were 6 babies out of 76 babies (7.89%) fed < 1 hour of life who developed hypoglycemia and 4 out of 24 (16.67%) babies fed > 1 hours but the difference between these groups were not statistically significant (p = 0.212).
ARTICLE 7: ASSOCIATION BETWEEN TRANSIENT NEWBORN HYPOGLYCEMIA AND FOURTH-GRADE ACHIEVEMENT TEST PROFICIENCY: A POPULATION-BASED STUDY
This was a study of 1395 newborns universally-screened for hypoglycemia at 3 hours of life found that newborns with hypoglycemia, even if corrected, had lower ability to gain proficiency in literacy and math at 10 years of age.
Glucose levels less than 45 were associated with a 38% reduction in gaining proficiency in literacy.
Glucose levels less than 35 or 40 were associated with roughly 50% reductions in proficiency in literacy and math.
ARTICLE 8: HYPERNATREMIC DEHYDRATION IN THE NEWBORN PERIOD AND LONG-TERM FOLLOW-UP
28 newborns admitted to NICU with hypernatremic dehydration due to insufficient breast milk intake and 178 newborns found from a literature review were studied. Information was obtained on a total of 150 patients. The babies had an average percent weight loss of 11.5% (admitted newborns) and 25.7% (literature review). Long-term follow-up was performed in 15 patients from the study group using the Bayley Scales of Infant Development and 2 patient were severely neurologically delayed and 5 patients were moderately delayed.
IN SUMMARY
The scientific literature has shown that hypoglycemia and hypernatremic dehydration cause irreversible brain injury that results in long-term disability. Hypernatremic dehydration has been found to occur as early as 7% weight loss from birth weight. Many babies who developed hypoglycemic brain injury lost less than the 10% generally considered acceptable for babies to lose. That is because the original accepted weight loss threshold of 10% came from a study of 7 exclusively breastfed babies, 2 of which developed 10% weight loss without any investigation of negative consequences like hypoglycemia, hypernatremia, brain injury or negative long-term developmental problems. This subsequently became the standard accepted weight loss without any further investigation into whether or not that weight loss was safe. Babies have been found lethargic and hypoglycemic by day 3 of life from hypoglycemia and dehydration and have been found to have extensive brain injury on MRI by the time they developed symptoms. For those who do not receive an MRI, parents may not see the effects of the hypoglycemia until years later when they are expected to talk, walk and learn. However, we now have evidence that glucose levels of less than 45 mg/dL are associated with measurable declines in long-term academic achievement. Furthermore, recent evidence shows that 10% of exclusively breastfed babies can develop brain-threatening levels of hypoglycemia (40 mg/dL) by 6 hours of life, for which they are currently not monitored.
Ultimately, babies who are fed enough milk, both breast milk or formula, are protected from these dangerous complications. They will often tell a mother when they are not receiving enough by crying inconsolably and nursing constantly in the first days of life. But mothers who are taught to strive for exclusive breastfeeding may be convinced to withhold supplementation beyond a child’s tolerance for fasting. Our most important job as parents and health professionals is to feed a newborn enough milk to prevent these tragedies.
Because, Fed is Best.
To see a video presentation on this subject, watch the Effects of Underfeeding on the Newborn Brain.

I have practiced for over 25 years as a family doctor delivering babies and finally have the data to support what I have observed and not been supported because of political ( b.s.) correctness.
Dr. Heather McLeod
I am so GLAD Dr. McLeod that we are able to provide you SCIENCE to support your intuition as a physician! Thank you for supporting mothers in feeding their babies! Christie
I have IGT. I was told to just keep feeding. My breasts never became full, I noticed how different they looked than the other breastfeeding moms. My son was 7 days old, had lost just over 2 pounds and was jaundiced when it was finally taken seriously. The more I read and find the more guilty I feel. He’s almost 2 smart and on track, but I always feel like I’m waiting for that first week to to be over, to stop feeling guilty.
Same situation. Please email me?
Katie, can you contact me? Have questions. Went through similar situation.
Hi Frances, I need her permission to give you her email. I’ll email her and see if she wants to connect.
How can I get a hold of Katie???
I emailed her your info. Thanks for supporting us!
Hi Katie, can I send Frances your email address? She is trying to reach you.
These are just case studies. There is no indication that the children wouldn’t have had feeding difficulties with formula as well nor is there any evidence that the developmental delays were connected to the lack of nutrition. Surely you know that a few anecdotal instances don’t indicate causation. Don’t you?
The scientific evidence on brain injury caused by starvation-related complications can be found in the resource page under preventing complications. The videos discuss the scientific and non-anecdotal evidence.
Thank you for quoting us! Wonderful article. Feed your babies every where and any where mothers. Their needs come first.
I’m so glad and heart broken to have found this. My son, now nine has extreme disability and delay. We fit this model to a tee. Nicholas was naturally born, a healthy 8lb4oz, our first child. We attempted breast feeding for the first 3 days of Nicks life. These days were spent in the hospital in an attempt to have the help and expertise we felt we needed as first time parents. Over the following days Nick dropped 12% of his body weight, we even enquired about the need for formula on day one as my wife was clearly not producing milk. We were informed that if we wanted to use formula her milk would not come in and breastfeeding is best, etc, etc. To be provided formula in the hospital we would have to sign a waver, the scare tactics were to much and we failed to move forward with formula due to medical professionals recommendations. Honestly I had made some peace with who Nick is, I had come to the conclusion that some children are just born damaged. Our child was unlucky and happened to be part of that percentile. I am now struggling to not believe that the medical community and pro-breast feeding groups should share in the blame. At a time when new parents are most varunable, scared and unsecure these groups push for something that not everyone can achieve and have long lasting repercussions. My son in amazing, I love him with all my heart, and I morn the person he could have been. Perhaps that’s selfish on my part but if this is happening to other families, children and is still the status quo something needs to be done. No baby should suffer due to the hubris of the medical community.
I’m so sorry this happened to you. You are not alone. That is why we shed light on the millions of babies and families that have been victimized by the current dogma on exclusive breastfeeding.
Wow! I was one of those babies. I’ve always wondered why it was so hard for me to retain information, pay attention, understand oral directions. I remember my mother telling me with a giggle that she almost starved me to death. I also remember my aunt telling me I was the skinniest baby she’s ever seen. Not that I blame my parents for any wrongdoing. We lived far back in the sticks on gravel roads and no car. My mother caught a ride in the milk truck (can you imagine?!) to take me to the doctor when I had scarlet fever as a tiny infant. The doctor noticed how thin I was and realised my mothers milk was almost nothing but water! Though I’ve had a great life and carrer I have had to do certain things by the skin of my teeth…..always had to work harder that anyone else. Thank you for the good things you’re doing. And thank all you ladies for sharing your stories. I wish you all the very best.
Deb Johnson