My name is Amber, and I am the mother of a charming, beautiful, and vivacious baby boy. I want to share with you a story: the story of my son’s birth and his first few months earthside. It is a multidimensional story full of love and heartbreak, but I think it’s important that other new mothers hear it. I hope they will know they are not alone if their early motherhood experiences are not what they always dreamed of.
I was working in an emergency room as a nurse and heading into my second-to-last semester of school to become a nurse practitioner. My husband and I had only been trying to conceive for a month. Because I have polycystic ovary syndrome (PCOS) and irregular periods, I figured getting pregnant would take longer, but there I was on September 1 with a positive test. We were ecstatic. As a planner, I spent most of the next nine months thinking about and planning everything about my son’s birth. I consider myself a well-educated woman and medical professional, so it was no surprise that the heart of my plans included breastfeeding my son. I spent months researching the best pumps for when I had to return to work, deciding on a storage-and-feeding set, and learning about ways to strengthen the breastfeeding bond. Formula feeding never crossed my mind. After all, I was always told breast was best. Sure, I had some friends who gave some formula here or there, but I just knew I would be one of the ones who would exclusively breastfeed and pump for my son.
Aside from terrible reflux, my pregnancy was fairly uneventful until the end of the third trimester. At my thirty-five-week appointment, my obstetrician pointed out that my blood pressure had increased for a few weeks. She said she didn’t think it was serious, but she wanted me to complete a twenty-four-hour urine total protein test to be sure. On Monday, while I was at work, I received the call—my urine tested positive for protein, an indication that I had developed preeclampsia. I stopped working, had to monitor my blood pressure daily, have ultrasounds every other day, and I was going to be induced at thirty-seven weeks. My world turned upside down. I had planned on a vaginal delivery, preferably without pain medication and with minimal intervention, so the idea of an induction was somewhat horrifying to me. However, I certainly understood the possible consequences of preeclampsia for mom and baby, and so I was completely in agreement with the plan to induce.
My husband and I went to the hospital at 9:00 p.m. on Sunday, April 23, to start the induction process. Twenty-one hours later, my son was born. My labor and delivery weren’t exactly how I’d imagined, but I was delighted to meet my son. He was six pounds, one ounce, nineteen inches long, and beautiful. He latched fairly well with assistance while in the delivery room about twenty minutes after his birth, and then we headed over to the recovery side.
During that time, we went through a number of difficulties. He was latching on almost constantly from his first night forward, and he would only nurse for a few minutes before falling asleep. This happened again and again. I saw the lactation consultant numerous times. She helped correct my latch, gave me a nipple shield on the left side to help my son latch to a flat nipple, and provided me with a hospital-grade pump so I could dry pump before I nursed. She encouraged me to save any colostrum I collected and feed it to him in a syringe. I only ever collected a few drops at a time—the largest amount was three milliliters in a syringe.
The second night was horrible. He was up “screaming and crying” all night long, wanting to latch constantly to my chapped and peeling nipples, but would fall asleep again, and the cycle would continue.
It was never suggested that his latch was poor or that I had any supply issues. No one told me that hormonal imbalances common to PCOS could wreak havoc on milk production. I was simply told that whatever colostrum I was producing was enough.

Thank God for the night nurse. During that second night, she checked on us at 2:00 a.m., and I was near tears from sheer exhaustion and frustration with his constant latching and then falling asleep. The nurse offered to take him to the nursery to weigh and supplement him. I was reluctant—after all, I had been told that formula would ruin his “virgin gut”(This is false) —but at my husband’s urging, I relented. My son came back an hour or two later, sound asleep for the first time since the hours after his birth. She told me he had eaten 30 ml because he was HUNGRY.
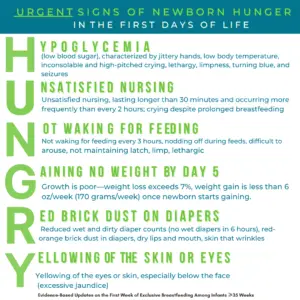
These are the signs of infant hunger while exclusively breastfeeding. Please supplement your baby to protect them from complications of insufficient breastfeeding and hunger and thirst.
His hearing was retested twice while in the hospital, and both times, they had to abort the test because he was crying inconsolably. The LC kept telling me we were breastfeeding fine, but I had the nurse leave some formula anyway “just in case”. I probably fed him five ounces of formula in the hospital. I continued trying to breastfeed him. The same behavior continued. We were told we could go home Wednesday morning. He appeared suntanned and was down to five pounds, eight ounces—a nine percent loss in two days, but were discharged anyway. We were told to bring him to the pediatrician for a first appointment and weight check within forty-eight hours.
At his weight check two days later, he was down to five pounds and seven ounces. During that time, he had continued to feed almost constantly and was nursing my nipples completely raw. I was told to hand express and pump to encourage my milk to come in, but I only ever got drops of colostrum. My milk didn’t come in for six days. When my son wasn’t sleeping, he was crying, or he was agitated, moving all over, sucking his wrists, trying to latch onto anything he could, and constantly rooting for a nipple. He was “cluster feeding,” and I was told that was normal and to keep breastfeeding him on demand. (This is not normal newborn behavior)

He had weight checks every few days for his first ten days. On the sixth day, the LC at the pediatrician’s office suggested doing a weighted feed to calm my nerves and reassure me that he was getting enough.
He weighed less after nursing for forty-five minutes than he did when he started the session. The LC laughed and said she must have weighed him wrong and not to worry about it.
Meanwhile, I was doing everything I could to increase supply as much as possible. I pumped after every feeding. I power-pumped. I drank gallons of water. I took herbs that were recommended to me and baked lactation cookies with brewer’s yeast and oats. Nothing made any difference.
By his tenth day of life, he was up all day and night, constantly screaming and crying. My husband and I were in tears because we had no idea what was wrong with our baby. The pediatrician had not seemed as concerned as we were, so I called her office that morning and insisted he had to be seen again that day. He was starting to seem lethargic to me; it was getting harder to rouse him to nurse, and I thought his fontanels appeared sunken. He was orange. He had not had enough wet diapers in days and was still passing red crystals in his urine. He had only two bowel movements that entire week. Something clearly wasn’t right with my son.
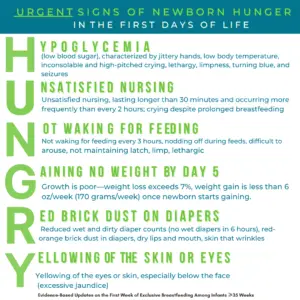
My son had all of the HUNGRY signs except for hypoglycemia. Why aren’t exclusively breastfeeding parents taught the signs of HUNGRY? Why?
She asked how often we were supplementing, and we told her it was only a few times a day because I was trying desperately to breastfeed him exclusively. She gently suggested it was time to supplement him with one or two ounces after every feeding. I was sad about having to use the formula regularly, but we were at our wit’s end with his inconsolable crying, and we (thankfully) decided to follow her advice.
Feeding my son formula had an immediate positive effect on him. His desperate hunger cries eased. He began to open his eyes and look around more often. He stopped looking so sunken. He began having wet and dirty diapers. He started to come to life in a way I hadn’t seen before.
I want to say that everything got much better and was wonderful from then on, but that would be a lie. My son struggled with the standard formula, so we switched to a sensitive variety. He seemed to do well with that for a few days until he started having severe gas pains and green mucous bowel movements. He ended up on hypoallergenic formula, and I cut dairy and soy out of my diet to continue giving him whatever milk I made.
I was still convinced I’d get my supply up enough not to need formula eventually. I started pumping more frequently and giving him pumped milk because he still fell asleep at the breast constantly and never seemed to latch right. He developed significant issues with reflux and eventually ended up on two medications for it. The dairy and soy-free diet wasn’t enough, and after thirteen weeks, we switched him to exclusive formula feeding because he seemed to do better on the formula than on breast milk.
Unfortunately, that wasn’t the last of our troubles. He developed colic, and despite being well-fed, gaining weight, and being happy and comfortable during the day, he would scream inconsolably for hours (usually from six to ten or eleven o’clock) every night. I convinced myself that his colic and reflux were my fault—if I could just have given him breast milk, none of this would have happened. I felt like a failure as a woman and a mom.
I also felt terrible because I am a medical professional, and I felt I should have been able to recognize the signs of starvation. I had starved my son. At times, I’d look at him and feel terrible for the experience he must have had in his early days, the hunger he must have felt. It destroyed me.
I began to resent my son and also turn my anger inward. My husband, meanwhile, had been home with me for our baby’s first two months, and he was drowning in anxiety about our son’s feeding, sleeping, and colic. We were both emotional wrecks.
The colic ended around ten weeks. I continued to pump and store milk until about sixteen weeks. At that point, my depression was so bad that I couldn’t think straight at work, felt like I was moving in slow motion through a fog, and was exhausted all day even though our son had started to sleep much better at night. When I finally reached out for help, I was officially diagnosed with severe postpartum depression (PPD), and I started on medication.
Here I am, a month and a half after starting treatment for PPD, and I feel like I have enough clarity to finally look back on the first few months of my son’s life. We both had a very rough start. I am certain that my feeding difficulties and feeling like a failure of a mom contributed in a huge way to the development of PPD. However, hindsight is 20/20, and while I was so against formula at the start, I am so glad in retrospect that our pediatrician made us supplement. Our son is thriving. He is more than fifteen pounds, happy, alert, playful, and thriving. I can now see that he loves me even though things didn’t work out how I wanted them to. I am finally able to enjoy him now that I am no longer a slave to the pump, producing only about one-third to one-half of what he needed every day. I think about our situation sometimes and realize that if it wasn’t for formula, my son could easily have suffered a significant brain injury or died. That’s the reality of it, and that’s the bottom line. For whatever reason, I couldn’t make enough milk. I’m not a bad person or a bad mom because of it. My son and I are both very grateful for those along the way who finally made us realize the most important truth of all is: Fed is Best.

HOW YOU CAN SUPPORT FED IS BEST
There are many ways you can support the mission of the Fed is Best Foundation. Please consider contributing in the following ways:
- Send us your stories. Share with us your successes, your struggles, and everything in between. Every story saves another child from experiencing the same and teaches another mom how to feed her baby safely. Every voice contributes to change.
- If you need support, we have a private support group– Join
- Join the Fed is Best Volunteer group to help us reach Obstetric Health Providers to advocate for counseling of new mothers on the importance of safe infant feeding.
- Donate to the Fed is Best Foundation. We are using funds from donations to cover the cost of our website, our social media ads, and our printing and mailing costs to reach health providers and hospitals. We do not accept donations from breast- or formula-feeding companies, and 100% of your donations go toward these operational costs. All of the Foundation’s work is achieved via its supporters’ pro bono and volunteer work.
- Share the stories and the message of the Fed is Best Foundation through word-of-mouth, by posting on your social media page, and by sending our resources to expectant moms you know. Share the Fed is Best campaign letter with everyone you know.
- Write a letter to your health providers and hospitals about the Fed is Best Foundation. Write them about feeding complications your child may have experienced.
- Print out our letter to obstetric providers and mail it to your local obstetricians, midwives, and family practitioners who provide obstetric care and hospitals.
- Write your local elected officials about what is happening to newborn babies in hospitals and ask for legal protection of newborn babies from underfeeding and for the mother’s rights to honest, informed consent on the risks of insufficient feeding of breastfed babies.
- Send us messages of support. We work daily to make infant feeding safe and supportive of every mother and child. Your messages of support keep us all going.
Thank you so much from the Founders of the Fed is Best Foundation!
Did your baby have a thorough oral assessment?? Did/does he have oral restrictions?? The symptoms you describe correlate with oral restrictions..
Even if there were, that child should have been supplemented and made to go hungry. Making babies cry for milk and forcing them to go hungry is unsafe, barbaric and illegal.