Sandra Stephany Lozoya combo-feeding her babies
In a world filled with parenting advice and conflicting messages, there emerges a beacon of wisdom and support – the upcoming release of the Fed Is Best book. Set to hit the shelves June 25, 2024, this transformative guide promises to navigate the intricate landscape of infant feeding choices, empowering parents with knowledge and judgment-free support. This highly anticipated book will reshape the conversation around infant nutrition, offering a comprehensive, science-backed, and inclusive perspective on the myriad ways families can safely and optimally nourish their babies.
Fed Is Best Book
What is the difference between this book and so many other breastfeeding manuals? The goal of the book is not to convince to feed your baby in one way or discourage you from feeding another by painting one type of feeding as ideal and the other as suboptimal or undesirable. The goal is to help you find the best way to feed your baby that fits your biology, your ability to produce milk, your baby’s needs, and the many social, economic, psychological, and practical factors that define what “best” infant feeding looks like for your family—which is different for every single family.

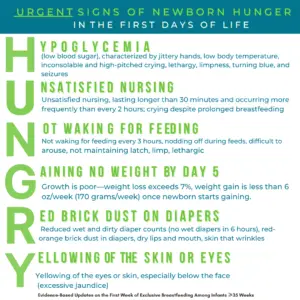
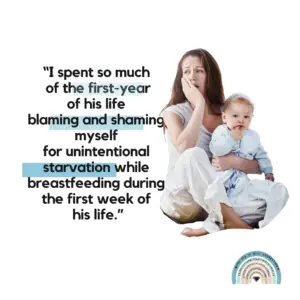
For too long, parents have had to accept a monolithic message that only exclusive breastfeeding provides the best for their infants. Mothers have been told that if they “perceive” that their milk is not enough, they are likely mistaken, under-educated, doing it wrong, or simply not trying hard enough. Little do they know that scientific research has shown that when measured by objective means, true insufficient milk supply is actually quite common. As a result, the message that insufficient milk is rare and supplementation is rarely necessary is putting many infants at risk and many mothers at risk postpartum mental health problems due to the faulty message that low milk supply is their fault. Little do parents know that health professionals have been witnessing a rise in complications of insufficient feeding of exclusively breastfed infants, like jaundice, dehydration, hypoglycemia, and failure to thrive, for as long as parents have been receiving this message. And the most common victims are those who have diligently followed the guidelines they have found in parenting and breastfeeding manuals yet found that their milk supply was truly too low to safely exclusively breastfeed.
This comprehensive and compassionate guide gives you the raw truth of about breastfeeding and formula feeding, dissects the history and science of breast- and bottle-feeding, and helps you prepare to reach your feeding goals in a safe and practical way. It does this by teaching you how to be flexible and respond to problems while working towards your goal, whether it be exclusive breastfeeding, exclusive formula feeding, or combination feeding.
This groundbreaking work is divided into two distinct parts, each addressing crucial aspects of infant feeding.
Fed Is Best Book
Part 1: The History and Science of Infant Feeding
The first section of the book lays a solid foundation by exploring the complex history and science behind infant feeding practices. It starts with Chapter 1, delving into the evolution of breastfeeding, the role of supplemental feeding, and the development of infant formula, providing readers with a broad context to understand how current practices came to be.
In Chapter 2, the book challenges prevalent beliefs surrounding breastfeeding, debunking harmful myths and shedding light on inconvenient truths that often go unspoken in the discourse on infant nutrition. This chapter aims to foster a more nuanced understanding and encourage critical thinking about the information often presented to new parents.
Chapter 3 addresses the polarizing debate between breastfeeding and formula feeding, questioning the notion of a singular “best” method of infant feeding. It presents evidence-based insights that highlight the benefits and considerations of each method, promoting a balanced view that respects individual circumstances and needs.
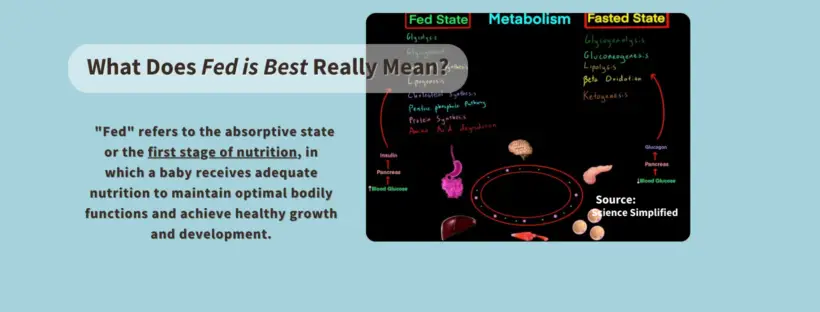
The final chapter of this section, Chapter 4 defines optimal infant feeding through a scientific lens, arguing why “Fed Is Best” is a principle that supports the health and well-being of all infants, regardless of the feeding method chosen by their families.
Part 2: The Fed Is Best Guide to Safe and Optimal Infant Feeding
Transitioning from the why to the how, the second part of the book serves as a practical guide for expectant and new parents. Chapter 5 discusses preparations before birth to ensure that parents are equipped with the knowledge and resources needed for optimal infant feeding from day one.
Chapter 6 focuses on the critical first few days of an infant’s life, offering guidance on how to protect against insufficient feeding and ensure that newborns receive adequate nutrition for a healthy start.
Subsequent chapters delve into the specifics of various feeding methods. Chapter 7 through Chapter 11 cover breastfeeding, pumped milk feeding, formula feeding, combination feeding, and bottle feeding, each chapter providing detailed advice, troubleshooting tips, and support for the respective feeding method. The book emphasizes the importance of honoring and supporting all families and their chosen safe infant feeding practices in Chapter 12, advocating for a non-judgmental and inclusive approach to infant nutrition.
The “Fed Is Best” book promises to be an essential resource for parents, caregivers, and healthcare professionals alike, promoting a more informed, compassionate, and inclusive approach to infant feeding. By combining historical context, scientific evidence, and practical guidance, this book aims to empower families to make informed decisions that best suit their needs and circumstances, ensuring that every infant is fed with love and care. Click the button below to pre-order your copy.
Fed Is Best Book