Dear Colleague and Parent:
My name is Christie del Castillo-Hegyi and I am an emergency physician, former NIH scientist, with a background in newborn brain injury research at Brown University, and mother to a 6-year-old child who is neurologically disabled. I am writing to you because my child fell victim to newborn jaundice, hypoglycemia and severe dehydration due to insufficient milk intake from exclusive breastfeeding in the first days of life. As an expectant mom, I read all the guidelines on breastfeeding my first-born child. Unfortunately, following the guidelines and our pediatrician’s advice resulted in my child going 4 days with absolutely no milk intake requiring ICU care. He was subsequently diagnosed with multiple neuro-developmental disabilities. Being a physician and scientist, I sought out peer-reviewed journals to explain why this happened. I found that there is ample evidence showing the links between neonatal jaundice, dehydration, hypoglycemia and developmental disabilities. I wish to explain to you how I believe this could apply to my son and the many children whose care you are entrusted with.
My son was born 8 pounds and 11 ounces after a healthy pregnancy and normal uneventful vaginal delivery. He was placed directly on my chest and was nursed immediately. He was nursed on demand for 20-30 minutes every 3 hours. Each day of our stay in the hospital, he was seen by the pediatrician as well as the lactation consultant who noted that he had a perfect latch. He produced the expected number of wet and dirty diapers. He was noted to be jaundiced by the second day of life and had a transcutaneous bilirubin of 8.9. We were discharged at 48 hours at 5% weight loss with next-day follow-up. We were told by the lactation consultant before discharge that he would be hungry and we were instructed to just keep putting him on the breast. Upon getting home, he became fussy and I nursed him longer and longer into the night. He cried even after nursing and latched back on immediately. He did not sleep. By the next morning, he stopped crying and was quiet. We saw our pediatrician at around 68 hours of life (end of day 3). Despite producing the expected number of wet and dirty diapers, he had lost 1 pound 5 ounces, about 15% of his birth weight. At the time, we were not aware of and were not told the percentage lost, and having been up all night long trying to feed a hungry baby, we were too exhausted to figure out that this was an incredible amount of weight loss. He was jaundiced but no bilirubin was checked. Our pediatrician told us that we had the option of either feeding formula or waiting for my milk to come in at day 4 or 5 of life. Wanting badly to succeed in breastfeeding him, we went another day unsuccessfully breastfeeding and went to a lactation consultant the next day who weighed his feeding and discovered that he was getting absolutely no milk. When I pumped and manually expressed, I realized I produced nothing. I imagined the four days of torture he experienced and how 2 days of near-continuous breastfeeding encouraged by breastfeeding manuals was a sign of this. We fed him formula after that visit and he finally fell asleep. Three hours later, we found him unresponsive. We forced milk into his mouth, which made him more alert, but then he seized. We rushed him to the emergency room. He had a barely normal glucose (50 mg/dL), a severe form of dehydration called hypernatremia (157 mEq/L) and severe jaundice (bilirubin 24 mg/dL). We were reassured that he would be fine, but having done newborn brain injury research, knowing how little time it takes for brain cells to die due to hypoglycemia and severe dehydration, I did not believe it, although I hoped it.

Born healthy, full-term weighing 8 pounds 11 ounces getting skin-to-skin and immediate breastfeeding after birth

Third day of life after the pediatrician visit. He was no longer crying and he was jaundiced and dehydrated with 15% weight loss. We were reassured that we could keep exclusively breastfeeding

Hypernatremic dehydration and encephalopathy from brain injury. Blank staring is a hallmark of newborn brain injury.
At 3 years and 8 months, our son was diagnosed with severe language impairment, autism, ADHD, sensory processing disorder, low IQ, fine and gross motor delays. He was later diagnosed with a seizure disorder associated with injury to the language area of the brain. Since my child’s diagnosis, I have been researching the scientific literature on breastfeeding insufficiency, newborn starvation, brain injury and developmental disabilities for over three years. In addition, I have collected the breastfeeding stories of tens of thousands of women through social media.
In the September 2015 issue of Hospital Pediatrics, an article was published describing 11 exclusively breastfed newborn babies who developed profound hypoglycemia between the second and fifth day of life from insufficient breast milk intake. The child described in the body of the article was a healthy full-term baby who presented just like my son. He was seen on the third day of life at his pediatrician’s office. Despite that, he was found on the fourth day of life lethargic and unable to feed. He had lost 10% of his birth weight and had a low glucose of 20 mg/dL (normal > 47 mg/dL). This child was given IV glucose after which he developed a seizure. They obtained a brain MRI which showed extensive areas of injury to almost the entire brain. In addition to this child, 10 other healthy term newborns were identified to have developed hypoglycemia from insufficient breastfeeding as well. They were found lethargic, seizing, hypothermic and/or not breathing. 5 out of the 6 MRIs obtained in these babies showed widespread injury to a third to almost the entire brain in varying patterns. They subsequently developed long-term neurological disabilities including seizure disorders, motor weakness, visual impairment and feeding difficulties requiring speech therapy.
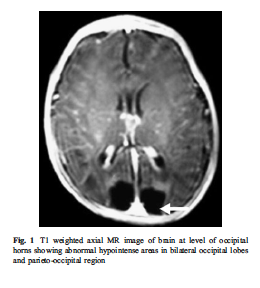
The brain MRI of an exclusively breastfed baby who developed lethargy and hypoglycemia (20 mg/dL) by day 3 of life from insufficient breast milk intake. The dark areas in the posterior part of the brain are the areas of missing brain tissue that resulted one month after the episode of hypoglycemia

Brain MRI of acute hypoglycemic brain injury. The light appearance in the posterior part of the brain is swelling and injury caused by caloric deprivation to brain cells due to hypoglycemia.
The answer to the epidemic of developmental disabilities we are seeing may be found in this vulnerable period. The risk factors for neurological disabilities in children all have to do with brain injury caused by excessive jaundice, loss of oxygen, circulation and glucose delivery to the brain. These include pre-eclampsia, intrauterine growth retardation and prematurity, which are caused by poor function of the placenta and decreased circulation to the baby. Hypoglycemia, umbilical cord prolapse, nuchal cord (cord wrapped around the neck), fetal distress, low Apgar scores, respiratory distress and other labor complications, events that all cause perinatal brain injury also cause long-term neurological disabilities. Although there are many causes of newborn brain injury that we have no control over, we have control over whether or not a child is fed enough for all their neurons to survive. I believe we may be inducing hypoglycemic brain injury to many newborns by asking mothers who may not be producing sufficient milk for their newborn’s physiologic need to exclusively breastfeed. We are potentially putting ourselves at odds with the protective natural instinct to respond to a baby’s cry by telling mothers that their colostrum is enough (which for many it may not be) and by making them fear failure by giving their child supplementation when they need it.
My child’s story is not rare. In a study of 280 mother-baby dyads, 22% of motivated mothers intending to exclusively breastfeed who received close lactation support experienced delayed onset of copious milk production, or lactogenesis II, which put her child at 7-fold increased risk of excessive weight loss greater than 10%. This means more than 1 in 5 newborns are at risk of starvation-related complications if exclusively breastfed from birth. In another study, it has been found that 10% of well-monitored exclusively breastfed babies undergoing the Baby-Friendly Hospital Initiative protocol develop hypoglycemia of less then 40 mg/dL within the first 48 hours. This incidence was even higher in babies born to first-time mothers as 23% developed hypoglycemia. This level of hypoglycemia has been shown in other studies to result in brain injury on MRI and long-term declines in cognitive function. One study showed that a glucose of less than 46 mg/dL within the first 24 hours of life was associated with a 3.7-fold increased risk of brain injury on MRI and a 4.8-fold increased odds of lower motor, cognitive and language scores at 1 year of age. This cognitive impairment persists as evidenced by another study of 1395 newborns showing that newborns who develop transient hypoglycemia of less than 40 mg/dL had a 50% reduction in passing their fourth-grade proficiency test in literacy and math. Even glucose less than 45 mg/dL resulted in a 38% reduction in passing the literacy test. The current standard of care tolerates a glucose between 40 and 45 mg/dL within the first 4 hours of life when there is no evidence that neurons have a greater tolerance for hypoglycemia in the first hours than they do at any other time.
I hope you feel the same sense of urgency that I do. Since we received our diagnosis, I have come to personally know 43 mothers whose children experience starvation-related complications from exclusive breastfeeding, including pediatricians, other doctors, nurses and lactation consultants. All of them have children with long-term neurodevelopmental impairments. While the literature cites poor education in breastfeeding as the cause of these starvation-related complications, in my research of breastfeeding mothers, it is the most educated in breastfeeding that are at the highest risk. The least educated will respond to a baby’s cry by offering a bottle. The mothers that are most educated in breastfeeding are the ones who have been taught that offering just one bottle will ruin her breastfeeding and potentially harm her child. I have learned that this is a distortion of reality created by breastfeeding education to pressure mothers to exclusively breastfeed that can put her child’s life at risk.
I am writing to let you know I believe the current newborn exclusive breastfeeding guidelines of the Baby-Friendly Hospital Initiative are dangerous. My son suffered an incredible amount of weight loss by the third day, which is often when mothers produce milk. How many newborns are experiencing this same fate? To date, there are no rigorously done studies on the safety of newborn weight loss and exclusive breastfeeding before lactogenesis II on the newborn brain. In fact, a study has shown that exclusive breastfeeding at discharge is associated with an 11-fold higher risk of rehospitalization for underfeeding and dehydration. In addition, the Academy of Breastfeeding Medicine jaundice protocol clearly states exclusively breastfed baby develop starvation jaundice from insufficient milk intake, a fact disclosed by no breastfeeding manual.
I would like to advocate for a patient safety initiative to increase monitoring and supplementation to prevent adverse neurologic conditions in all exclusively breastfed newborns as described by the following:
1) Mothers should be instructed on how to manually express to confirm the presence of milk, which is available through this link. Any baby whose mother has little to no colostrum should be offered supplementation immediately.
2) Twice daily weighing for exclusively breastfed newborns in the hospital and at home as it has been shown that the least-fed newborns can lose the maximum recommended weight loss of 7% within the first 24 hours. This practice should be continued at home until breastfeeding meets the child’s full metabolic requirement as signaled by the onset of daily weight gain. The 7% weight loss threshold should be provided to the mother to help signal the need for supplementation in the hospital and at home.
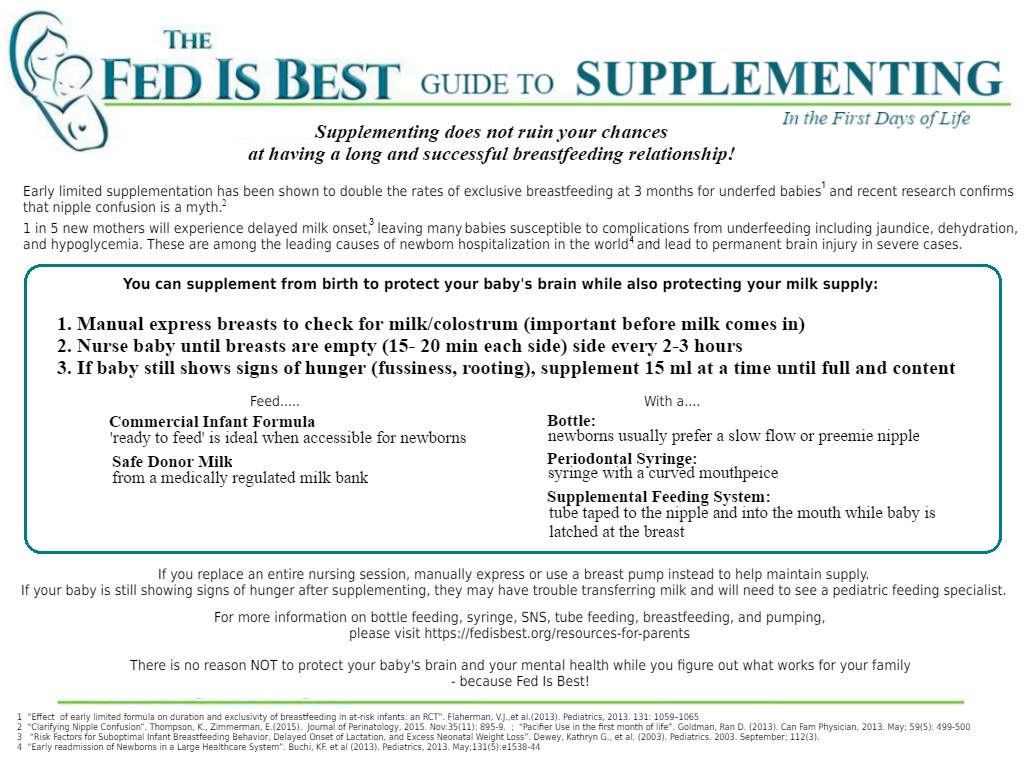
3) Universal daily transcutaneous bilirubin checks and glucose monitoring while in the hospital for exclusively breastfed newborns before the onset of daily weight gain as the scientific literature has now identified them as a high-risk population for hypoglycemia. The physical exam is insufficient to rule out hypoglycemia and pathological hyperbilirubinemia. Any inconsolable child should also have a glucose check as this is an often-missed sign of hypoglycemia. Supplementation with breast milk or formula as well as IV glucose should be given immediately at a glucose level less than 47 mg/dL as this is the only prospectively validated glucose threshold that if corrected immediately prevents the development of developmental delay. Supplementation should also be offered for bilirubin levels exceeding 15 mg/dL or any level considered high risk on the bilirubin nomogram. Not only does supplementation for underfed newborns protect a child’s brain and stabilize glucose but it also doubles the rates of exclusive breastfeeding at 3 months.
4) Pre- and post-breastfeeding weights after lactogenesis II to measure the amount of milk transferred to the baby. The caloric requirement of a newborn baby is 100-120 kcal/kg/day and a mother’s production should be around 2 ounces per feed every 3 hours to meet that demand. This is roughly 5.5 oz/kg/day (2.5 ounces/lb/day, please use kg to prevent feeding errors). Some babies with medical conditions may need more than the above volumes.
5) Next day after discharge follow-up with pediatricians and lactation consultants with universal bilirubin and glucose checks in the office. Children who are crying inconsolably at home especially before lactogenesis II should be supplemented after nursing UNTIL they reach their health care provider in order to prevent the development of hypoglycemia, dehydration and negative neurological consequences.
6) I advocate for mothers to be informed of the possibility that her child can become dehydrated, jaundiced and hypoglycemic from insufficient breast milk intake and that these conditions can cause developmental and neurological disability. Signs of this are a child that is not sleeping or crying repeatedly after breastfeeding as well as nursing near-continuously. Lethargy, poor feeding, seizures, hypothermia (low body temperature) and bradycardia (slow heart rate) are late signs that suggest the presence of profound brain injury from near-complete glucose deprivation to the brain. Lethargic hypoglycemic babies deserve a brain MRI to provide vital information to parents so that they can closely monitor their development and obtain early intervention as needed.
7) Every mother should be educated on supplementation after nursing in order to continue the stimulation needed to promote milk production in case the need for supplementation arises, particularly before discharge if lactogenesis II has not occurred. If a child is hypoglycemic, greater than 7% below the birth weight, hyperbilirubinemic, hypernatremic or crying inconsolably out of hunger, supplementation can be offered 15 mLs at a time as the newborn stomach has been in fact measured to be 20 mL in size at birth, much larger than commonly taught to mothers and health professionals. Supplementation should be offered until a child’s laboratory markers are corrected and the child is no longer in distress. A child’s brain will not wait for food. Once the child is adequately fed, the breastfeeding may then be evaluated to identify the cause of underfeeding. Supplemented breastfeeding is a valid choice as NO BENEFIT of exclusive breastfeeding justifies the risk of life-long disability caused by hypoglycemic brain injury. Any mother sent home without a supplementation plan is being sent home to potentially starve and disable her child if her milk does not arrive on time.

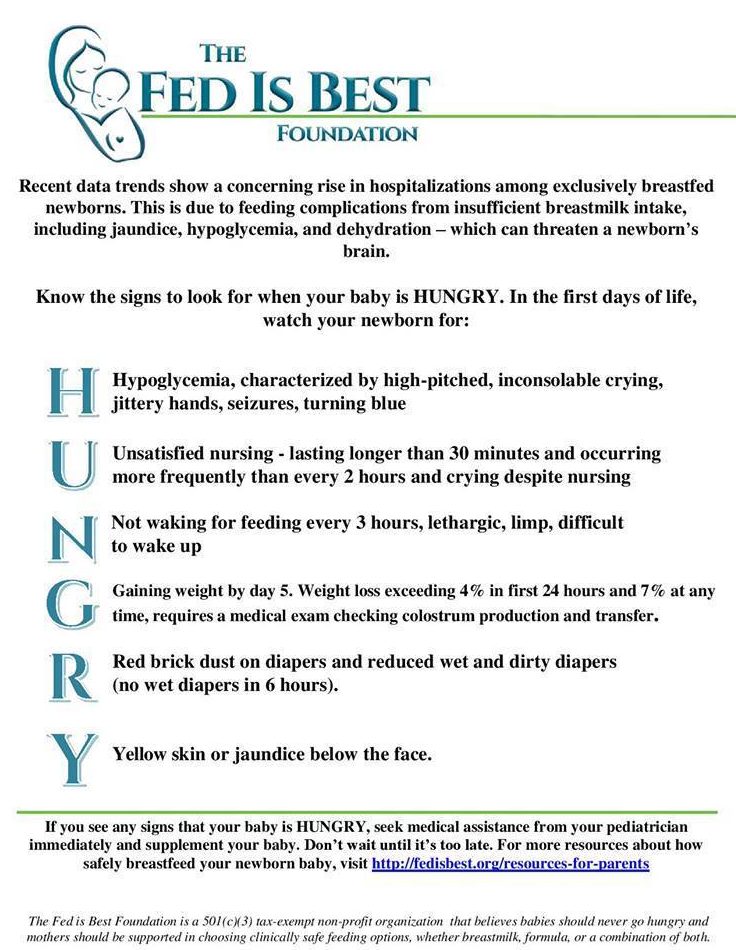
Evidence-based guide to protecting your baby from insufficient feeding complications. Click to download and print
Mothers are taught by breastfeeding manuals that they will uniformly be able to produce enough milk for their baby’s needs and will feed them near-continuously for weeks without question if their doctors and lactation consultants tell them not to give formula. But as you have witnessed as a matter of routine, breastfeeding jaundice is very common and mothers do not uniformly produce enough milk for their babies’ needs. The learned wisdom of grandparents who know instinctively the sound of a hungry baby is being supplanted by breastfeeding manuals that cannot teach that sound to the new parent. If you observe non-Western cultures all around the world, babies are given pre-lacteal feeds or milk through wet nurses when mother’s milk is not enough in the first days of life because instinctively, we as a species protected our newborns by responding to their hungry cry. Thousands of years of evolution have wired mothers to respond to this cry and we are interfering with a biologically protective instinct by telling mothers that their child is getting enough when it is apparent to them that they are not. Babies get admitted to the ICU lethargic, jaundiced and dehydrated every day because their mother did not know it was possible to have insufficient milk. The scientific literature has shown that 1–6% of breastfed babies all around the world are rehospitalized for complications associated with exclusive breastfeeding in the first days of life. The most recent publication on hospitalizations for newborn jaundice at a Baby-Friendly hospital system showed that out of 104,460 babies born in a 3 year period, 10,583 or 1 in 10 babies were hospitalized for phototherapy, the majority of these cases completely preventable with early supplementation. That means millions of babies have been hospitalized since the 1991 publication of the Baby-Friendly Hospital Initiative which codified this protocol. The Baby-Friendly Hospital Initiative and the WHO breastfeeding protocol protects the breastfeeding more than it protects the baby and countless babies have endured days, weeks and even months of hunger in order to meet its goals.
The time for magical thinking has ended. Breastfeeding education is based on many premises not consistent with reality. No time in the history of this planet have we allowed babies to cry out for milk for as long as we tolerate for the purpose of breastfeeding. The first law of nature is and has always been that Fed is Best. Many parents are led to harm their own babies because of what they have been taught about breastfeeding. As you can see, if such a severe case of jaundice and dehydration can occur to two physicians taking home their first-born son, it can happen to anyone.
To all doctors and parents, my message is simple. Feed your baby. Provide your baby its physiologic needs every minute, including the days before milk production. The only person who knows what a newborn needs is that newborn. The accidental starvation of a newborn child is a tragedy by any definition. We are allowing newborns to receive less than their nutritional requirements and telling parents that they are doing what is best for their children. We must be certain an infant is actually getting fed by every available mean. I hope you join me in informing your colleagues, friends and family of the data and make changes to your practice. Please feel free to share this letter with whomever you wish.
Respectfully,
Christie del Castillo-Hegyi, MD
christie@fedisbest.org
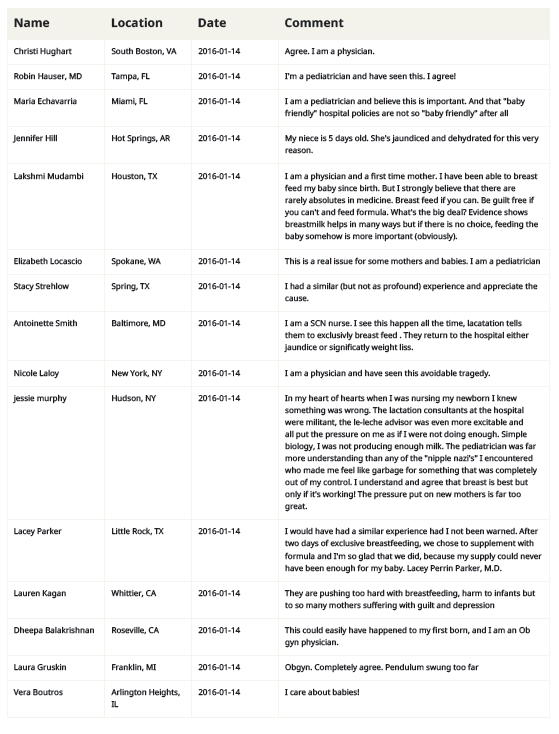
To read the stories and the testimony of thousands of parents, newborn nurses and pediatricians who signed the Fed is Best petition, click the PDF below.
To read about the Fed is Best Foundation’s meeting with the top officials of the WHO Breastfeeding Guidelines Committee, please go here. From the meeting:
Dr. del Castillo-Hegyi: “Can I just ask one more question, are there any plans within the WHO to inform mothers of the risks of insufficient breast milk and the risks of brain injury in order to make sure that they are aware when a child is critically ill at home, that supplementation can protect their child from brain injury?”
Dr. Rollins: “That specific recommendation, that was not identified by the experts in the guidelines scoping as a top priority. Within the guidelines, there is literature in general on the danger signs, things like convulsions, being lethargic and not being able to feed. Those are clinical signs that are routinely included in materials taught to health care workers and when health workers communicate to mothers. Those signs are identified as ‘alert’ signs…The signs that needs assessment to identify the underlying cause is firmly there within the WHO guidelines.”
The citations to scientific articles referred to in the letter are available through the links found within the text of the article.
To learn how to prevent newborn feeding complications, please go to the following:
- Resources for Parents – information on how to supplement while maintaining the breastfeeding relationship and how to closely monitor infants for underfeeding
- Feeding Plan – a way to communicate your feeding preferences to your health providers
- Weighing Protocol – a way to monitor your baby’s growth and prevent dehydration
To learn more about the Fed is Best Foundation, please go to our About page.
Dr. del Castillo-Hegyi provided the Committee data on the rates of insufficient feeding complications, namely jaundice, hypernatremic dehydration and hypoglycemia among exclusively breastfed newborns and the risk of brain injury and developmental disabilities caused by those conditions. She discussed the failures in patient education and patient management that come from Baby-Friendly policies and how they result in thousands of newborn admissions a year.
Jillian Johnson spoke about her son Landon, who she attempted to exclusively breastfeed under the guidance of her Baby-Friendly hospital. He developed cardiac arrest from dehydration and underfeeding 12 hours after discharge despite 2 days of constant crying and nursing in the hospital, which her health professionals deemed normal. He died after 2 weeks on life support. She asked the Committee, “How is a mother to know if her child is in danger if everyone tells her the constant crying and nursing are normal?” She asked the Committee to put in place standard practices and patient education guidelines to prevent these complications from happening to other infants.
Information for Hospitals: Ensuring Safety for Breastfed Newborns
Dangers of Insufficient Exclusive Breastfeeding Grand Rounds Presentation
Donate to Fed is Best
Disclaimer: This document does not replace in-person physician evaluation and treatment. This document is meant to inform parents of the most recent data regarding infant feeding and to increase their knowledge on how to protect their newborns from hyperbilirubinemia, dehydration, hypernatremia, hypoglycemia and extended or repeat hospitalizations due to complications from underfeeding. Earlier supplementation may be needed for babies who are premature or have medical conditions. It is recommended that a parent seeks evaluation by a pediatrician for any concerns regarding the health and safety of her baby if they arise.


This could have been my daughter. She starved with my insufficient colostrum and then milk production for 5 days. I had a normal pregnancy, went into labor spontaneously, and delivered vaginally at 40w3d. At the hospital, the nurses and LCs all said she had a great latch, and we were doing regular feeds. But she cried A LOT and never seemed satisfied. One of the LCs looked strangely at my breasts and asked if they had gotten larger during my pregnancy and I said I think so and that was it.
My daughter was discharged with >7% weight loss at about 40 hours old, and we took her to the pediatrician every day for the next 3 days for weight checks. At the third visit, the pediatrician did a weighted feed that showed she only transferred one ounce. My pediatrician said that was fine, but she was still losing weight and crying inconsolably, which my husband and I told the doctor. My mom told me my daughter needed formula, but I *knew* that would ruin our breastfeeding relationship and that of course I produced enough. I had “researched” and taken a breastfeeding class. I’m so upset that I didn’t just listen to her.
By day 5, I noticed brick dust in my daughter’s diaper, which the written materials the hospital sent home said could be a sign of dehydration (no one told me that; thank God in the exhaustion of going home I took the time to read all the materials). I immediately pulled out the sample can of formula and made an ounce, which she sucked down. She then passed out and SLEPT for the first time. My husband and I were so alarmed because she was so limp that we took her back to the ER—we were afraid something was very wrong with her. When we got there, she peed and pooped everywhere when we tried to undress her to weigh her. She weighed in at 6 lbs, 13 oz, a 1 lb., 5 oz. total loss. I believe that’s a 16% weight loss. I can’t look at the pictures of how skinny her legs got now without crying.
At the ER, they tested her bilirubin and miraculously she wasn’t jaundiced. She sucked down a full 2 oz premade formula bottle and went back to sleep. We switched fully to formula until I could see a laceration consultant on Monday (this was Saturday night when we went to the ER), and she pigged out during that day and a half to catch up for what she had lost. She gained back a pound by Monday morning!!
The LC tried to kill me with a plan where I had to breastfeed with a supplemental nutrition system, then follow up with a bottle if needed, then pump every 3 hours day and night. I made it 2 weeks with the SNS before I was mired deeply in PPD (which was never diagnosed despite numerous pediatrician and LC visits). I dreaded every feed. I made it another 2 months BFing, then supplementing with formula, then pumping. And then I realized it was silly. I still was producing a max of one ounce total from both breasts every 3 hours. I quit BFing and pumping cold turkey and barely got engorged.
And my daughter continued to grow and thrive and I finally had the time to bond with her and enjoy feeding her. I called the LC to thank her (!!!) for all her help and to tell her about how I never even really got engorged after quitting cold turkey. She told me she thought from the beginning that I might have insufficient glandular tissue due to the large,m gap between my slightly tubular breasts and larger than normal nipples. But she didn’t want to “discourage me.” I was so enraged. I could have killed or permanently damaged my child because I physically can never produce sufficient breast milk, and no one thought to tell me????
My daughter is 5 1/2 years old now and so bright and full of life. There are so many times I look at her and hurt so badly for what I did to her, while at the same time I’m *so* thankful she does not appear to be injured. After what I went through, I was traumatized and obsessed with making sure she was eating enough. She’s a little overweight now, which I’m sure is my fault, but I’m permanently scared of starving her again.
I am SO thankful for what you are doing with Fed Is Best. I hope that no other mother has to feel what we do. In our country, no baby should be allowed to starve due to insufficient breast milk when formula is safe and readily available. You hit the nail on the head when you said our mothers and grandmothers know what a hungry baby cry sounds like. We must make sure this generation does, too.
Thank you so much for sharing your story. Every mother’s story helps another mother know the dangers of insufficient feeding and protects a future child from hunger. Thank you!