The shaming began prior to delivery, at the hospital breastfeeding class. A soon-to-be mom asked if she should keep some formula on-hand, just in case she was unable to breastfeed. The lactation consultant (IBCLC) insisted she not keep any formula around because, as soon as you start feeding the baby formula, you will give up on breastfeeding and never forgive yourself! She also said it was rare for a mother to not be able to produce enough milk, which is not true. I told her it was fine to get some formula, if for nothing than to relieve the intense pressure of exclusively breastfeeding that was being forced in our class. The IBCLC also instructed us not to use our pump for at least twelve weeks, and even then, only if we were returning to work–because pumping would interfere our milk supply. I later learned this is also not true.
Category: Baby-Friendly Protocol Complications: Starvation, Jaundice, Hypoglycemia, Dehydration, Newborn Falls
Fed is Best Foundation receives stories from mothers who have been led to harm their infants in the pursuit of increasing exclusive breastfeeding rates. Learn about the dangers of insufficient feeding in breastfed infants caused by Baby-Friendly Hospital Initiative.
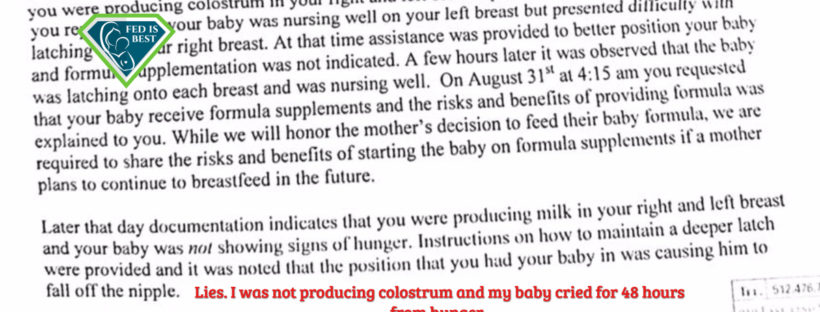
When A Mother Says She Isn’t Making Enough Colostrum, Believe Her The First Time
My son, Jackson, was born healthy and weighed 6lbs 15oz. As a first-time mom, I trusted my hospital would help me to exclusively breastfeed my baby. The nurses and lactation consultants helped me with proper latch and positioning and told me he was doing great. He wanted to nurse every hour, and I was exhausted.

I began to think something was wrong because he cried and cried and continued to cry even after every breastfeeding session. I kept asking the nurses if I was making enough colostrum and they said I was, but they never, ever checked to see if I was even producing colostrum.
I had brought my pump to the hospital so I could learn how to use it since I was going back to work. I asked if I could pump my breasts to check and they said no, that my baby would become nipple-confused. I then asked for formula because I just knew he was hungry. They very strongly discouraged me from using formula every time I asked.
What Happens When Mothers Are Told Being Fed Is The Bare Minimum?
The Fed Is Best Foundation has a private Facebook support group for mothers who need a safe place to talk about their infant feeding challenges without judgement. Mothers told us how they felt when they fed their babies formula.
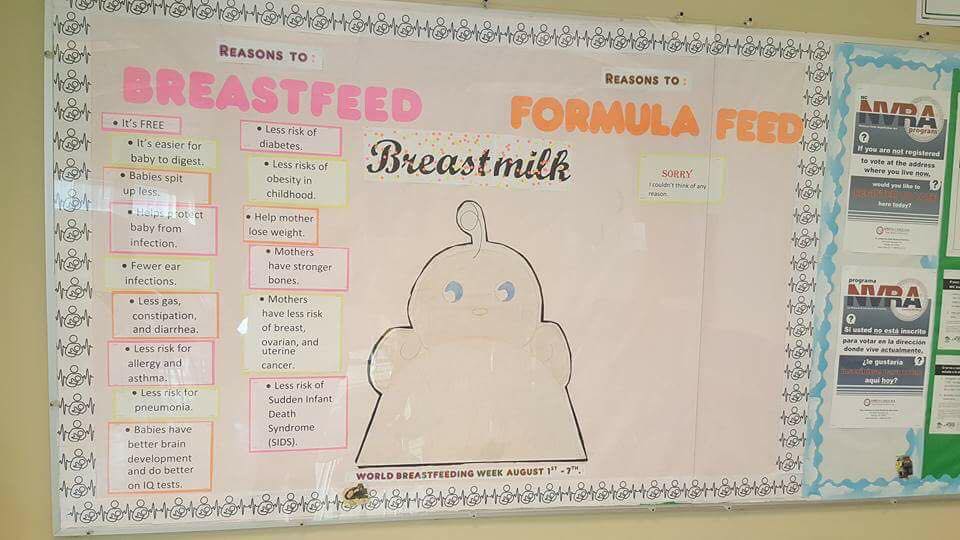
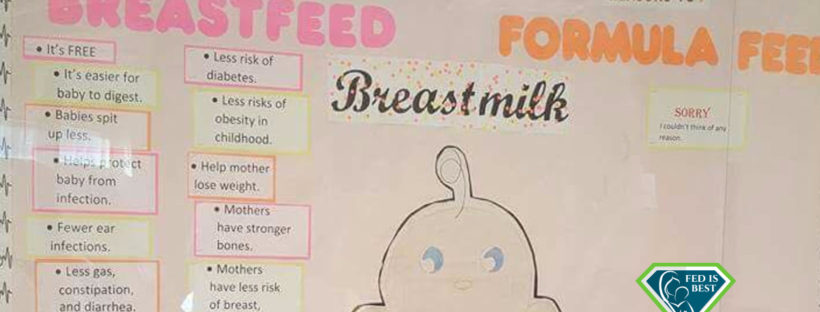
Bulletin Board At A WIC Office
Shannon: I was told my daughter needed formula when she was hospitalized for three days. I cried for those three days because I felt so guilty. I kept telling her “I’m sorry. I’m sorry for doing this to you, baby girl. Mommy is so, so sorry.” The doctors had to bring me food because I refused to leave my daughter alone. Granted, she was only four months old, but at that time, I just couldn’t leave her. I felt like she had to know I was there for her, that I felt terrible for unknowingly starving her. My husband at the time came to visit and he held me for hours as I cried saying “It’s my fault. It’s all my fault. I wasn’t enough. I’m not enough for her. They told me I would be enough and I’m not.” To this day, when I have one of my bad days, it all repeats in my head– the psychological damage is still there.
The Fed is Best Foundation’s Top Priority is Saving Babies’ Lives
Christie del Castillo-Hegyi, M.D., Co-Founder of the Fed is Best Foundation
In response to a letter written by 1000 Days director, Lucy Martinez-Sullivan and follow-up editorial from Kimberly Seals Allers, we wanted to take an opportunity to set the record straight.The mission of the Fed is Best Foundation is to protect infants from complications and injuries resulting from accidental starvation under currently promoted breastfeeding policies. In order to protect infant safety and ensure the patient and human rights of mothers and babies, we have built a non-profit organization committed to: (1) the study of exclusive breastfeeding complications that can result in brain injury and, in the most severe instances, death; and (2) raising public awareness to signs of infant hunger and the consequences that can result based on peer-reviewed research.
As part of our public health awareness commitment, the Fed is Best Foundation has developed and compiled extensive resources for parents and health professionals to promote safe breastfeeding and safe infant feeding policies based on evidence, including, the science of infant feeding, the caloric and fluid requirements of newborns and the caloric yield of exclusive breastfeeding. These core matters of infant feeding are shockingly absent from current breastfeeding curricula and protocols. Our Foundation is not against breastfeeding; it is for safe breastfeeding and close monitoring to prevent complications and injuries to infants reported in the medical literature, the media and by the thousands of mothers who have sent us their stories, which we receive each and every day. Continue reading
I Contacted Every Patient Safety Organization After My IBCLC Withheld Clinical Information From Me Causing My Newborn To Starve.
When I struggled to breastfeed my son, I believed I was failing, not just at breastfeeding, but at motherhood. What was supposed to be the “best” way to feed my new baby was painful, anxiety-inducing, and landed my son back in the hospital for dehydration, eleven percent weight loss, and inability to take a bottle.
My hospital’s solution included many appointments with their lactation consultants, fenugreek from their new mother boutique, and a nurse-bottle-pump (triple-feeding) routine that drove me to the brink of despair and did nothing to increase my milk supply.
At no point in my son’s first two months did any of the lactation consultants, nurses, doctors, or any other medical staff offer a concrete explanation for my low milk supply or my son’s vice-clamp latch. Because no one seemed to know why we couldn’t get the hang of it, I felt I was not trying hard enough.
Sometime after my son’s first birthday (my original “breastfeeding goal”), I came across several online articles that explained insufficient glandular tissue, also called breast hypoplasia. I knew my breasts were an odd shape, but I was taught by the hospital lactation “experts” that breast shape and size didn’t determine breastfeeding ability. Looking at pictures of similar widely-spaced, tube-shaped breasts that produced little or no milk left me feeling a strange cocktail of emotions—validation, disbelief, anger.
I wondered why staff at my hospital, a long-time Baby Friendly Hospital Initiative (BFHI) accredited facility, hadn’t told me that I was at risk of insufficient milk production.