I don’t think I ever thought about infant feeding till I became pregnant. I never looked at a baby and wondered what it was fed. But it seems like everyone nowadays is so concerned; it’s the first question I was asked with each pregnancy. When I imagined myself as a mother, I always saw myself breastfeeding. It’s something I wanted desperately, and yet, I couldn’t produce enough milk for my babies. I have insufficient glandular tissue (IGT) and I don’t make more than a half ounce to an ounce per feeding.
Category: Supplementing and Combination-Feeding
I Had Permanent Tear Streaks On My Face – Thank God For The Fed Is Best Foundation
The act of giving doesn’t have to be physical to be meaningful. When I think of giving, I think of one support group that has given me more emotionally than I could ever imagine. It’s hard to describe how much they have given me. This is my story.
During my first pregnancy, I thought I had done everything right. I read all the books, ate the right foods, went to all of my doctor appointments, and exercised. I had always planned on breastfeeding and never gave a thought to another option. I studied up on the perfect latch, breast shields, nipple pads, and milk production. I was so excited to have that bonding experience that everyone talked about. The day he was born, that dream came crashing down.
I Am Celebrating 20 Months Of Combo-Feeding- Despite All Of The Lies Taught By My Hospital LC
Today, after 20 months of combination feeding, I gave my son his last bottle of milkies. I wasn’t able to keep my supply up after I stopped pumping at work. But I feel so proud of myself. 20 months of combo feeding. I made it 20 months!
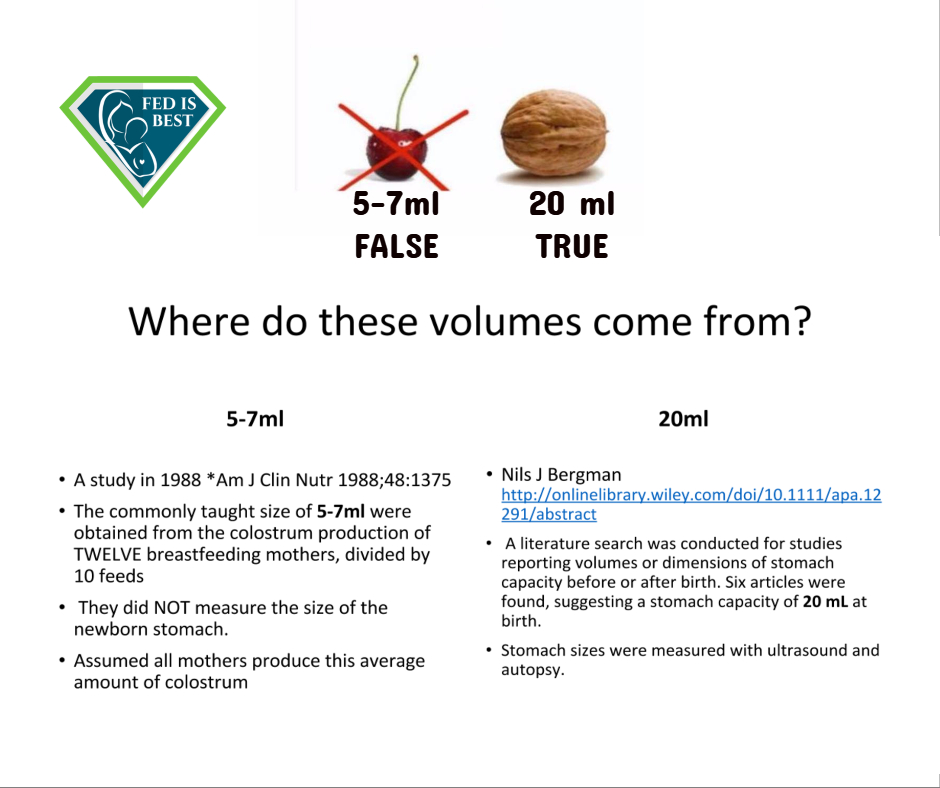
When my son was born, I expressed concern about possible nursing problems because of my history of hormonal issues—but I was repeatedly dismissed. He lost 10% of his weight in the hospital. I was told that supplementing would basically end my breastfeeding relationship. That it would hurt my supply. I was instructed not to pump. I was told about tiny infant stomach sizes and that the constant crying and nursing was normal. I was told not to worry about insufficient feeding until day five. Well, by day five my son had lost 13% of his weight. That’s when we brought him back to the hospital.
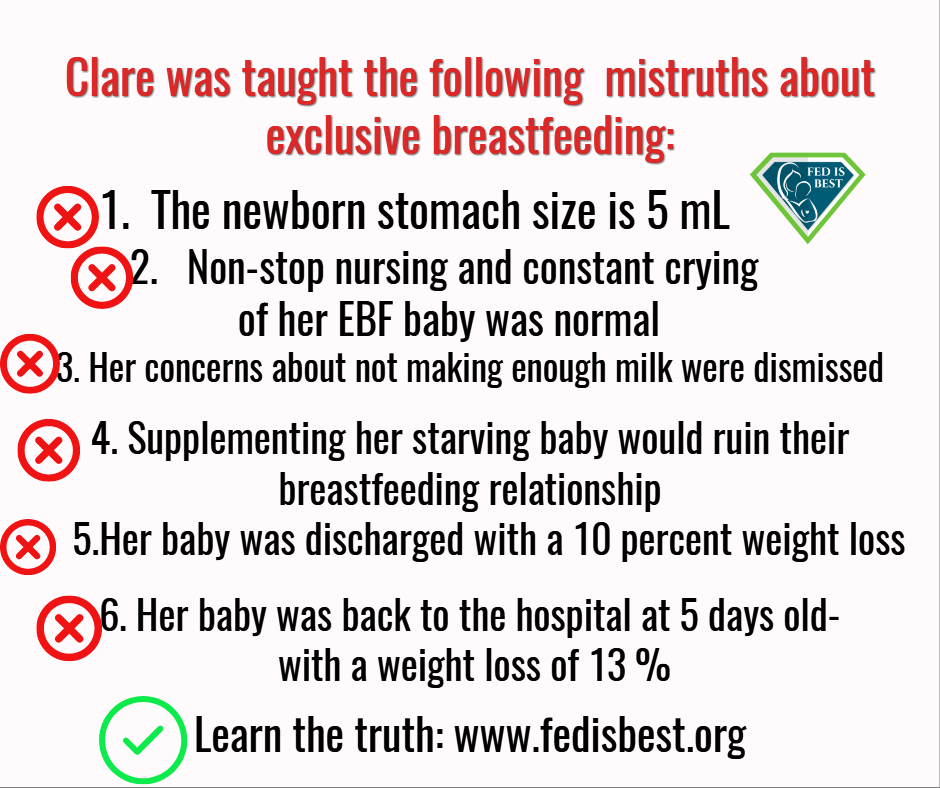
After a weighted feed, we found that my milk hadn’t come in and that I was barely producing any colostrum. My son’s gums and tongue were dry. The nurse admitted he was a day away from hospitalization. She was one of the nurses I called in a panic after we got home. She taught the breastfeeding class and parenting class I attended before my son was born. She visited our room at the hospital several times after the birth. And she simply believed the lie that under supply is rare and that tummy size are tiny. I found out recently that the hospital is still teaching this. That same nurse who, after finally acknowledging my son’s drastic weight loss and recognizing that I actually did have supply issues, developed a triple feeding plan for us. It wasn’t until ten days after my son was born that my milk finally came in.
I was devastated to find out that I couldn’t exclusively breastfeed my son. And I was angry that my risk factors for low supply were ignored. Angry that despite my son’s obvious distress and significant weight loss, my concerns were dismissed. Angry that I was instructed that just one bottle would ruin any chance I had at breastfeeding.
I am now proud that I made it 20 months. 20 long months of combo feeding a child with dairy and soy allergies—despite being told my odds of doing so were pretty much impossible. I shouldn’t be the exception. Women are often told that long-term combination feeding just isn’t possible. It is possible for many of us, but not all of us. I know too many women who—like the Academy of Breastfeeding Medicine is finally acknowledging—believe that one bottle means “the horse is out of the barn” and that they might as well stop breastfeeding. It doesn’t need to be this way.
Sometimes I am asked, “If you truly believe formula is equal to breast milk, then why did you keep nursing despite your struggles?” To that I say, it’s what I wanted to do; it’s something I love doing. And that is good enough. I don’t need everyone to be exactly like me and to find meaning in what I love. I don’t need to feel superior. I don’t need to justify why I continued to nurse by denigrating someone else’s decision or inability to not do the same. One does not cheapen the other. Fed is best!
To learn how to prevent newborn feeding complications, please go to the following:
- Resources for Parents – information on how to supplement while maintaining the breastfeeding relationship and how to closely monitor infants for underfeeding
- Feeding Plan – a way to communicate your feeding preferences to your health providers
- Weighing Protocol – a way to monitor your baby’s growth and prevent dehydration
HOW YOU CAN SUPPORT FED IS BEST
There are many ways you can support the mission of the Fed is Best Foundation. Please consider contributing in the following ways:
- Join the Fed is Best Volunteer group to help us reach Obstetric Health Providers to advocate for counseling of new mothers on the importance of safe infant feeding.
- Make a donation to the Fed is Best Foundation. We are using funds from donations to cover the cost of our website, our social media ads, our printing and mailing costs to reach health providers and hospitals. We do not accept donations from breast- or formula-feeding companies and 100% of your donations go toward these operational costs. All the work of the Foundation is achieved via the pro bono and volunteer work of its supporters.
- Share the stories and the message of the Fed is Best Foundation through word-of-mouth, by posting on your social media page and by sending our resources to expectant moms that you know. Share the Fed is Best campaign letter with everyone you know.
- Write a letter to your health providers and hospitals about the Fed is Best Foundation. Write them about feeding complications your child may have experienced.
- Print out our letter to obstetric providers and mail them to your local obstetricians, midwives, family practitioners who provide obstetric care and hospitals.
- Write your local elected officials about what is happening to newborn babies in hospitals and ask for legal protection of newborn babies from underfeeding and of mother’s rights to honest informed consent on the risks of insufficient feeding of breastfed babies.
- Send us your stories. Share with us your successes, your struggles and every thing in between. Every story saves another child from experiencing the same and teaches another mom how to safely feed her baby. Every voice contributes to change.
- Send us messages of support. We work every single day to make infant feeding safe and supportive of every mother and child. Your messages of support keep us all going.
- Shop and Fed is Best Foundation will earn cash back! We hope to develop our online safe infant feeding classes with these funds.
- If you need support, we have a private support group– Join
Thank you so much from the Founders of the Fed is Best Foundation!
The Medical Professionals At The University Of North Carolina Allowed My Baby To Starve
I wish I had done more research about hospital exclusive breastfeeding policies before my son was born. I’m a registered nurse with a Bachelor of Science in Nursing, but my maternity and pediatric experience was limited to nursing school. I was always on the fence about breastfeeding—I said that it was my goal but that we would see, so I hadn’t bought in to the narrative of “Breast is Best”. Still, I expected the medical professionals at the hospital where my son was born to tell me if they thought my baby was starving while attempting to exclusively breastfeed.
I delivered at the University of North Carolina Hospital, a top medical center. I felt reassured that I was in great hands. They were called “baby friendly” after all. I didn’t look into what that meant, and I thought I was well prepared. I was induced after being diagnosed with preeclampsia, but, thankfully, it was caught very early. I was two days shy of forty weeks. I had a long labor, followed by a C-section due to my son’s position. I’m also thirty-five years old, so by all accounts, I was high risk. It also meant I was at risk for late or low breast milk supply.
First, my husband and I were laughed at when we said we planned to use the nursery. Thank God for my husband—he did the baby care and brought our son to me while I was bedridden so that I could breastfeed. I was told the latch was great. I felt confident things were going well. But my son was inconsolable by the time he was forty-eight hours old.
My baby nursed a lot. I was told everything was normal and he was “cluster feeding”. Later, as my training came back to me, I never remembered cluster feeding being a thing. During my training, babies were supplemented when mothers didn’t have enough colostrum babies were supplemented and were taken to the nursery if a parent requested. I went to Duke University, and I rotated through WakeMed. These are excellent hospital systems.
I was concerned about my baby’s very dry lips, and I was told not to worry. I asked about the few wet diapers that my son produced. Dismissed. I trusted that the medical professionals had my and my baby’s best interests at heart. I asked if maybe my milk hadn’t come in, and I was told all is well. We went home on the evening of the third day after birth, and my baby was looking jaundiced. He cried a lot, but nursing helped soothe him from crying–sometimes.
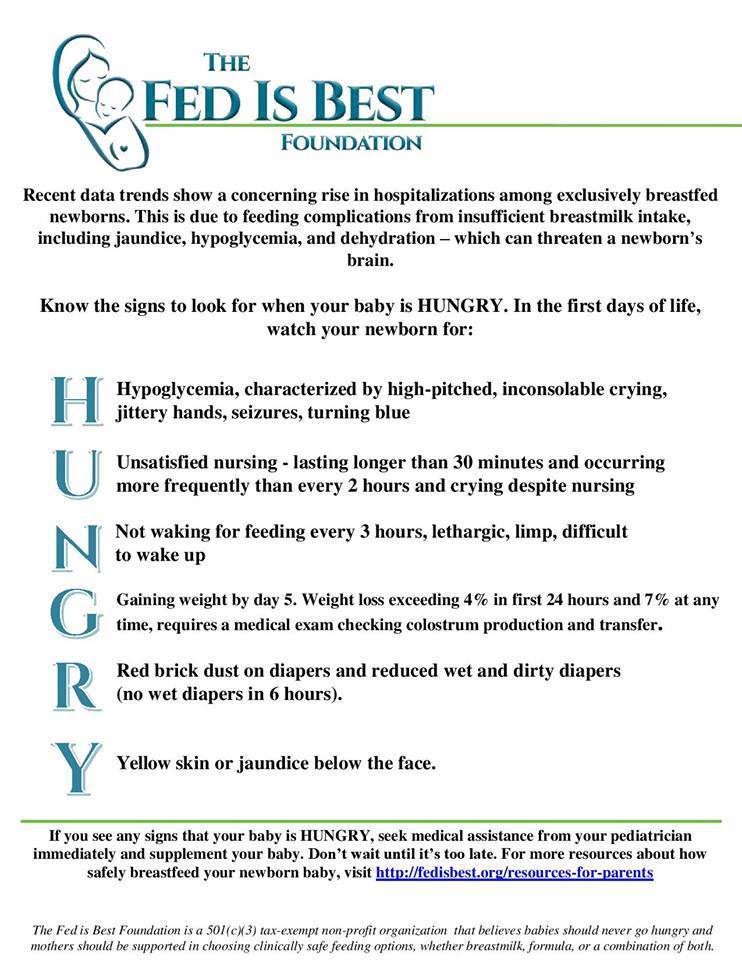
We saw the pediatrician the next day, and I found out my son had lost twelve percent of his weight since birth. We did a weighted feed in the doctor’s office, and his weight before and after nursing were exactly the same. My pediatrician, my husband, and I had a conversation about giving the baby formula. My husband and I had already decided we were going to supplement with formula before we saw the pediatrician, and our son’s weight loss confirmed that we were right to do so. We did not hesitate, and he had his first bottle minutes after we got home. He sucked it down, and he was finally calm and content for the first time in days. I tried to pump and barely got anything. My milk eventually came in, but we continue to supplement. His weight rebounded, and he gained well, but I was beside myself knowing that my baby had starved. It shouldn’t have come to that.
I am upset that the nurses (most of whom were fairly new) don’t know the difference between true cluster feeding and starvation. I am livid that no one even suggested formula.
I Was Producing Drops Of Breastmilk And My IBCLC Denied My Request To Supplement My Baby With Formula.
My son, Harrison, was born 8 weeks ago at a Hospital in Fredericksburg, Va. He decided it was time to meet mom and dad two weeks before his due date and was born via C-section after 22 hours of labor. At birth he was 8 pounds 2 ounces and 21 1/2 inches long.
Before giving birth, my husband and I took every class the hospital offered. We took the two hour infant CPR class, nine hour childbirth class, three hour bringing home baby class, and three hour breastfeeding class. As first-time parents, we were filled with nervous excitement. Harrison is our miracle baby. I went through fertility treatments because PCOS and hyperthyroidism made it impossible for me to get pregnant without medical intervention.
After the unplanned C-section I was in no shape to help with Harrison’s care. The sweet nurses spent time with my husband and showed him how to diaper and swaddle. When it came time to breastfeed, Harrison latched right away and fell asleep soon after.
This continued for 12 hours and I started to become concerned. A lactation consultant was making the rounds and stopped in to check on us. I told her I didn’t think Harrison was actually eating or that I was producing anything. She specifically asked if I had PCOS and said that having that condition could affect my milk production. A few minutes later, she sent in another consultant to hook me up to a pump.
I pumped for 20 minutes and got droplets. The other consultant assured me this was enough to feed my eight pound baby. This was Thursday.
On Friday afternoon my husband left the hospital to install the car seat, set up the bassinet, and buy a few things at Target. I was left alone for the first time since Harrison’s birth. Harrison was born at 10:35 a.m. on Wednesday, so by midday on Friday he was really starting to get hungry. Knowing I wasn’t producing milk and that my baby hadn’t eaten, I started to cry—a lot. A nurse came in and asked what was going on. I explained that I didn’t think Harrison was getting any milk. She sent in a lactation consultant.
I asked the lactation consultant for formula to supplement, but she didn’t give me any. She said to keep trying to breastfeed because I was able to produce droplets the day before and she put me on a pumping regimen.
We left the hospital Saturday afternoon. Harrison was jaundiced and had lost 10% of his birth weight. He hadn’t eaten yet in his life and I still had no milk. We got home and I continued to breastfeed him every two hours. He’d latch, then fall asleep. My husband would try to wake him up and then hand him back to me to feed. The cycle would continue for an hour. Then we took an hour off and tried it again. At this point Harrison didn’t want to latch any more.