Jody Segrave-Daly, RN, IBCLC and Christie del Castillo-Hegyi, M.D.
The Fed is Best Foundation is dedicated to ensuring safe infant feeding for every single child, a goal that can be achieved with exclusive breastfeeding, combination feeding, exclusive formula feeding and tube-feeding. We have no political affiliation. We support all mothers to help their infant thrive with safe, sufficient and sustainable feeding in order to protect their health and optimize brain development. Recent news has broken about the U.S. delegation at the 71st World Health Assembly opposing the first draft of the Infant and Young Child Feeding resolution. We have provided a line-by-line break down of the first draft of the resolution, which was set to be proposed by delegates from Ecuador, as well as the proposed draft submitted by the U.S. delegation along with our interpretation of the lines that the U.S. delegates opposed.
In an editorial published in the New York Post, two pediatricians, Dr. Alma Golden and Dr. Brett Giroir, who were key members of the U.S. delegation attending the 71st World Health Assembly, wrote about the rationale for the U.S. opposition of the first draft:
As pediatricians, US representatives at this year’s World Health Assembly in Geneva and supporters of breastfeeding throughout our professional careers, we were shocked to read recent headlines, in the New York Times and elsewhere, claiming that the administration has somehow called into question the importance of breastfeeding for infants.
The administration fully endorses breastfeeding, and the agencies where we work — Health and Human Services and USAID — communicate this unequivocally…We don’t just affirm these priorities in formal conference rooms in Geneva. For years, the US government…has invested millions of dollars to promote breastfeeding both at home and abroad.
All of which is to say: Breastfeeding wasn’t in dispute in Geneva. Rather, we raised objections to an early draft of the resolution we eventually supported, which made references to a controversial 2016 guidance document. The underlying policy goal of this guidance is unsupported by US nutrition guidelines and inconsistent with the practice of most families in our country…
In particular, the guidance recommends that countries impose stringent new regulations on the marketing of any commercially produced foods suggested for children between 6 months and 3 years old. Such restrictions, in our view, prevent parents from having access to all the factual information they might need. The guidance even advocates for the prohibition of free samples of formula — including in countries and conflict zones where supplies of formula could help save babies’ lives.
Most important, there are good and valid reasons, both medical and personal, why some mothers cannot breastfeed, or choose not to breastfeed exclusively. This is particularly true in situations where displacement, other trauma or malnutrition have made it impossible for mothers to breastfeed their children, and these babies’ lives are at risk without formula or other nutritional supplementation. Parents in these dire situations need all the information and choices available.
The issue of child malnutrition occurring in war torn countries has been reported on by CNN reporter Gayle Lemmon in her article, “Don’t make babies rely on breast milk in war zones,” where she interviewed members of Doctors Without Borders who reported taking care of many infants suffering from severe malnutrition as a result of the strict restrictions of the World Health Organization and UNICEF on formula donations.
‘Over the past couple of weeks we’ve seen an increase in the number of malnourished children needing treatment,” Doctors Without Borders’ Iraq country director Manuel Lannaud said in an interview released on the group’s Web site.
The surprising thing is that Lannaud and his colleagues at the humanitarian aid group didn’t place the blame for these underfed little ones just on war and the fact that the city was under siege. They also put the blame on other international organizations and policies that seek to do good.
“It isn’t a problem of access to food. The malnutrition we see here is primarily due to the scarcity of infant formula,” Lannaud wrote. “International organizations like UNICEF and the World Health Organization (WHO) promote breastfeeding … and provide infant formula, but only by prescription. We believe that distributing infant formula in a conflict situation like Iraq is the only way to avoid children having to be hospitalized for malnutrition.”
Doctors Without Borders says it agrees that breastfeeding promotion is a priority, but one that comes after dealing with the immediate crisis of a baby’s survival. Says Lannaud, if mothers “need formula, we give it to them.”
The mothers who need it are those facing down life-and-death situations each day, often while caring for multiple children in the shadow of war. That giving infant formula to them is so controversial speaks to a policy tripwire few outside the humanitarian realm even know exists: global “breastfeeding first” policies.
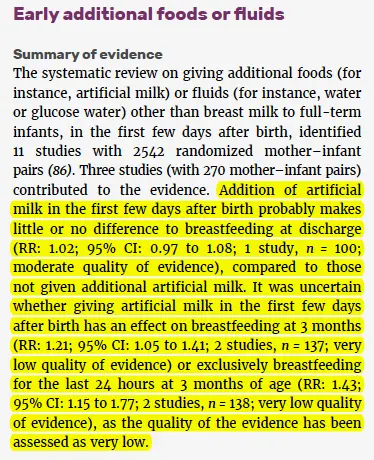
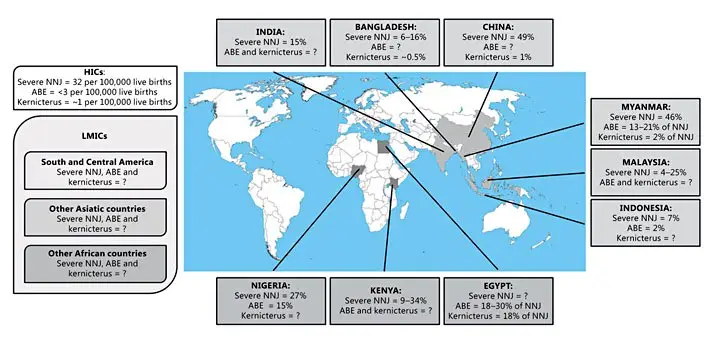
The WHO breastfeeding policies are not without flaws and aggressive promotion of exclusive breastfeeding has resulted in harm, namely an epidemic of newborn hospitalizations for jaundice, dehydration and hypoglycemia, known causes of brain injury and developmental disability, in the U.S. and across the globe. In addition, there has been a rise in accidental suffocation of newborns, called Sudden Unexpected Postnatal Collapse, from prone positioning during to skin-to-skin care and breastfeeding, made worse by maternal exhaustion from 24/7 rooming-in, practices encouraged but the WHO Ten Steps and by Baby-Friendly policies. The promotion of exclusive breastfeeding from birth has contributed to an epidemic of neonatal jaundice in the developed and developing world, which has contributed to an epidemic of perinatal brain injury and cerebral palsy particularly in the developing world, where few health care resources are available to monitor and treat exclusive breastfeeding complications. Promoting exclusive breastfeeding from birth over the local, traditional practices of supplemented breastfeeding (with wet nursing, animal milk or sugar water) until the onset of copious milk production has discouraged a practice that breastfeeding mothers used to prevent hunger and starvation-related complications like jaundice, dehydration and hypoglycemia, which now are the leading causes of newborn rehospitalization in the world.
Continue reading →