Written By Rachel
As a young girl, I knew something was wrong with my breasts when they began to develop. I had asymmetric tubular breasts, and it quickly became my biggest insecurity. At the age of 20, I saw a doctor who told me a breast augmentation would “fix” them. Trusting her medical opinion I had breast augmentation surgery. Now they were double the size and sagging from the weight of the implants. It was worse than what they originally were, making my anxiety and insecurities heightened. After a few years, I decided to get them removed by another doctor who specializes in reconstruction surgeries. I got the implants taken out, a lift of the skin and fat removed from my stomach to fill the empty pouches. With two surgeries comes many scars and of course trauma to the breast tissue.
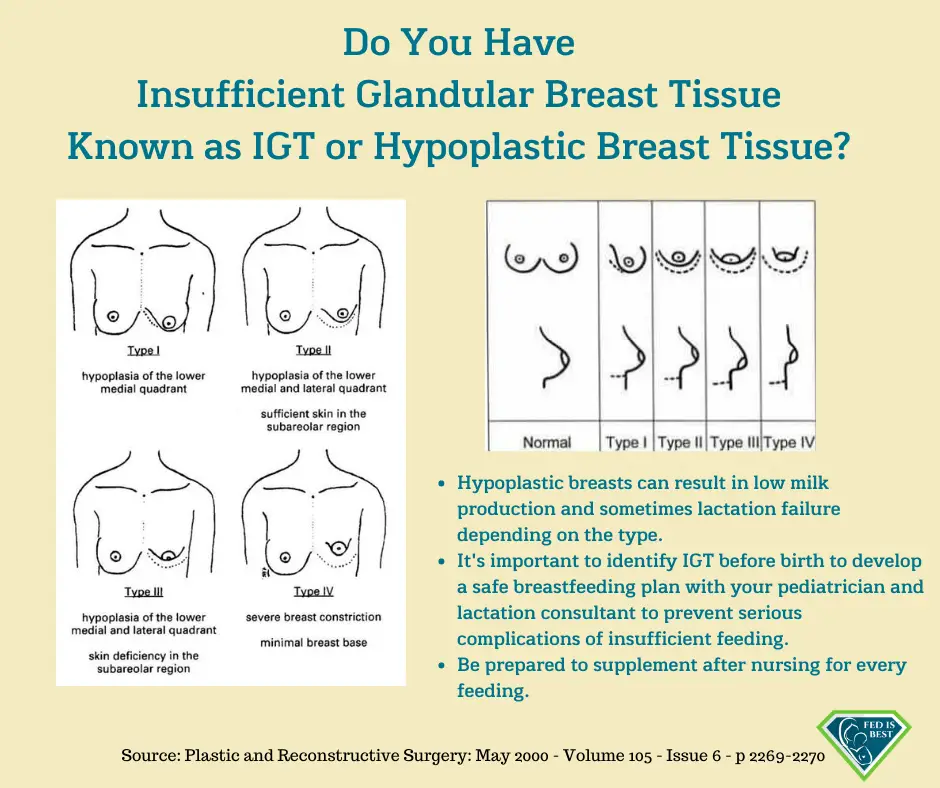
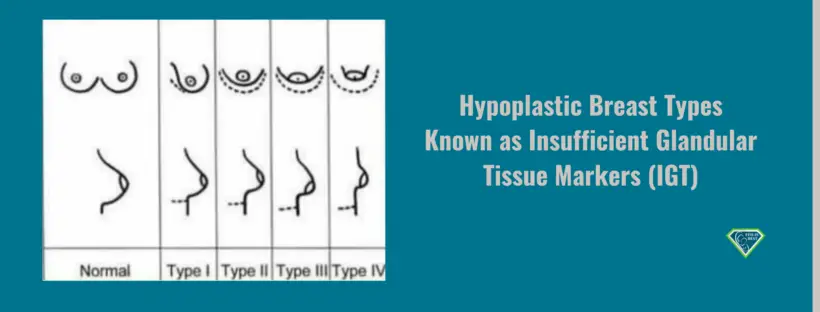
“Tubular breasts” is the name of a condition caused by breast tissue not proliferating properly during puberty. The condition is also called tuberous breasts or breast hypoplasia.
While not extremely common, tubular breasts cannot be considered rare because many women don’t seek treatment. While tubular breasts don’t pose any direct threat to your health, some women may seek to correct it. Tubular breasts can also present problems for women who wish to breastfeed. (source Healthline)
Struggling with my insecurities of developing differently my entire life, I never wanted to breastfeed. Why would these deformed breasts work to give a child nutrients? As a young adult, I also didn’t care if I could or couldn’t breastfeed because again, this was a struggle my whole life and it never seemed like I would be “normal” enough to do something every other woman could. Fast forward seven years after my breast reconstruction, I’m married with a baby on the way. My biggest prayer was to be able to breastfeed my baby, but I knew going into it the likelihood was very, very, low and there was no telling if I could until the baby came. I had the mindset of trying my best but knowing formula would help my baby thrive just as well breastmilk.
My beautiful baby girl was born on June 2, 2020, smack dab in the middle of a global pandemic. With the help of three nurses, we immediately tried to latch her, but no surprise to us all, it wasn’t easy. A shield was given to me and I latched my baby as best as I could, hoping something would come out. I was given the choice to supplement with formula at the hospital until my milk came in, so we did that but continued trying to latch her at every feed. I quickly realized breastfeeding was going to be the hardest thing I’ve ever had to do in my life. Once we brought our baby home, we continued what we learned at the hospital every time she ate. My husband would help position the baby as I would hold on the shield, we would attempt to latch her through her screams, using a syringe to squirt formula into her mouth to get her on and hold our breaths that she’d stay on. Usually, we’d get her on for a few minutes, she’d fall off, and we’d fight through her crying to put her back on again, because “mamas are supposed to breastfeed, and it’s what is best for my baby.”
After a week of headaches and heartache listening to our daughter scream as we fought with her to latch, stay latched, and drink from me, only to have to give her a bottle afterward. I decided to meet with a lactation consultant. I knew this couldn’t be it. There had to be a better way or something that I was doing wrong or that I could do better. Because of being in the middle of COVID, I struggled to find an LC. I called countless companies and the local hospitals, but no one could help, or I would have to pay $300 out of pocket because insurance didn’t cover it. Knowing that there was no way I was doing this right and that I wasn’t ready to throw in the towel, I kept searching and found a company based out of a city four hours from me who offered virtual visits that my insurance covered. For two hours, I worked with an LC through video chat who showed me different techniques to help my baby latch, using her babydoll and jelly breast. After that, we did find more success with feeding, but it was still a struggle for all of us.
The LC recommenced I begin pumping after every feed. So that’s what I did. I started to pump and to my surprise, milk came six days after she was born! A half-ounce each pump, but man, I was excited! We were able to slowly begin making bottles of breastmilk to give our baby along with formula bottles for what I wasn’t able to produce. Our stress level began to dwindle but putting her to my breast was still such a struggle and something I dreaded doing.
After meeting with another online LC and one in person, we decided for our sanity, that I would just pump to give her as much breast milk as I could, and for what I couldn’t, we would continue to give formula. During my LC appointment in person, we did a weighted feed and realized she was getting barely anything from me, 4 grams in 15 mins on one side to be exact. No wonder she would fall asleep and had to eat after—she was working so hard. This decision to pump full time allowed my husband to participate in feedings at night while I pumped, and best of all, the screaming fits and fighting to latch our daughter stopped, and our quality of life drastically improved. My milk slowly started to increase. Now I’m able to pump 0.5–1 oz on my left breast and 0.5–1.5oz on my right at each pumping session.
We still put the baby to the breast for many reasons, but accepting that she isn’t feeding on my breasts until she’s full was a hard pill to swallow.
It’s been a struggle to decide if giving my baby three bottles a day of breastmilk is worth it. Is it worth all the time I’m spending hooked up to the pump to only get a total of 0.5 oz most time? So many days I wanted to quit, because sitting there for 30 mins to get less than an ounce, and then to have the baby not finish a breastmilk bottle and dumping it down the drain, was clearly taxing on my soul! But I’m proud to say, we are five weeks (almost six) in and I am still pumping every 2–3 hours around the clock. I am able to give my baby 3–4 bottles of breastmilk a day. I usually produce 10 oz total in one day of pumping. The most I can get would probably be 12 oz and that’s with pumping extra in a day, which is very hard to find the time to do!
It is still hard to look online and read the stories of over suppliers (how I wish I had that problem!) or watch some women pump 10 oz in one session when that’s what I get in the entire day. It’s discouraging. It’s taken me the whole five weeks to accept that I’m a freaking rockstar mom and if I’m able to only pump three bottles for my baby then so be it. At least it’s three bottles! I’ve come to terms with the fact that this is hard work, and it may be harder for me because of my history; however, I do think breastfeeding is just hard in general—but my baby girl is worth it.
I don’t know how long I’ll keep this up. I don’t know how long my milk will last. I honestly don’t know if my body registers supply and demand like it should, but I know that today I’m not ready to give up, and I hope that continues. And when I decide enough is enough, I’ll be proud of the ten ounces I was able to make in a day to give my baby, because the odds were certainly stacked against me. Trying to find a lactation consultant to help me learn how to breastfeed made me totally understand why so many women feel like they can’t continue breastfeeding.
What I’ve also learned throughout this long month is that breastfeeding looks different for everybody and even though my baby doesn’t eat fully from my breasts, I can proudly say I am able to breastfeed my baby and she is one cute happily fed baby girl!
HOW YOU CAN SUPPORT FED IS BEST
There are many ways you can support the mission of the Fed is Best Foundation. Please consider contributing in the following ways:
- Join us in any of the Fed is Best volunteer and advocacy, groups. Click here to join our health care professionals group. We have: FIBF Advocacy Group, Research Group, Volunteer Group, Editing Group, Social Media Group, Legal Group, Marketing Group, Perinatal Mental Health Advocacy Group, Private Infant Feeding Support Group, Global Advocacy Group, and Fundraising Group. Please send an email to Jody@fedisbest.org if you are interested in joining any of our volunteer groups.
- If you need infant feeding support, we have a private support group– Join us here.
- If you or your baby were harmed from complications of insufficient breastfeeding please send a message to contact@fedisbest.org
- Make a donation to the Fed is Best Foundation. We are using funds from donations to cover the cost of our website, our social media ads, our printing and mailing costs to reach health providers and hospitals. We do not accept donations from breast- or formula-feeding companies and 100% of your donations go toward these operational costs. All the work of the Foundation is achieved via the pro bono and volunteer work of its supporters.
- Sign our petition! Help us reach our policymakers, and drive change at a global level. Help us stand up for the lives of millions of infants who deserve a fighting chance. Sign the Fed is Best Petition at Change.org today, and share it with others.
- Share the stories and the message of the Fed is Best Foundation through word-of-mouth, by posting on your social media page and by sending our FREE infant feeding educational resources to expectant moms that you know. Share the Fed is Best campaign letter with everyone you know.
- Write a letter to your health providers and hospitals about the Fed is Best Foundation. Write to them about feeding complications your child may have experienced.
- Print out our letter to obstetric providers and mail them to your local obstetricians, midwives, family practitioners who provide obstetric care and hospitals.
- Write your local elected officials about what is happening to newborn babies in hospitals and ask for the legal protection of newborn babies from underfeeding and of mother’s rights to honest informed consent on the risks of insufficient feeding of breastfed babies.
- Send us your stories. Share with us your successes, your struggles and everything in between. Every story saves another child from experiencing the same and teaches another mom how to safely feed her baby. Every voice contributes to change.
- Send us messages of support. We work every single day to make infant feeding safe and supportive of every mother and child. Your messages of support keep us all going.
- Shop at Amazon Smile and Amazon donates to Fed Is Best Foundation.
Or simply send us a message to find out how you can help make a difference with new ideas!
For any urgent messages or questions about infant feeding, please do not leave a message on this page as it will not get to us immediately. Instead, please email christie@fedisbest.org.
Thank you and we look forward to hearing from you!

Additional IGT stories:
I Found The Fed Is Best Foundation Before The Birth Of My Third Child – Thank God For Them.
Thanks for sharing your story. I have tubular breasts and nobody talked to me about how it could be an issue. I’m kind of sad as I was told not to pump for the first 6 weeks to not create an oversupply but doing so, my milk production has been really low and I read everywhere that now that I’m more than two months postpartum, it might be too late to make it for it. I’m going to try though and it is really nice to read a story of someone who has a similar experience and not just “low supply is not really a thing, breastfeeding is possible for everyone if you want it hard enough”. Thank you
Thanks so much for sharing your whole experience. Your story is very similar to mine in having tubular breasts, having surgery young me at 19 same thing my doctor told me. Was super unhappy took 7 years to save up to get them removed and do fat transfer. Two lifts later I’m looking at having a baby later on this year and worry of the struggles I may have to breast feed. You’re story gives me hope and great advice as to how to prepare best. . Wishing you and your family the best.