Mothers who experienced delayed onset of milk production or experienced low milk supply with their first baby often contact us for support to try breastfeeding again. They typically have anticipatory anxiety because they have lost trust in their lactation professionals and hospital staff and are unwilling to attempt breastfeeding again without supplementation. They want to know how to supplement their baby until their milk supply becomes sufficient to feed them safely while providing proper breastfeeding stimulation for optimal milk production.
The most common concerns expressed:
- Fear of the pressure to exclusively breastfeed
- Fear of failing to breastfeed again
- Fear of advocating for themselves and their babies while in the hospital
- Fear of being shamed by hospital staff when wanting to supplement until their milk comes in
- Fear of being denied formula or not receiving it promptly
- Triggers from the previous negative breastfeeding experience, such as being touched without consent
Monica writes: “I lost confidence in breastfeeding because I didn’t make enough milk for my first son, who required hospitalization for severe jaundice and a 13% weight loss. I was devastated and furious when the neonatologist told me he was starving. In my birth hospital, my son had been forced to cry from hunger, and I was told my body would make enough milk for him by every lactation consultant and nurse in the hospital. I trusted them. They were wrong! I no longer trusted breastfeeding and decided to pump and bottle feed to ensure he got enough milk. I purposely delivered my second baby at a hospital that didn’t force me to breastfeed exclusively. After starving my son, I was not taking any chances, and I supplemented my daughter after every breastfeeding session. My breastfeeding experience was the opposite of my son’s, and I remember tearing up several times because she was so peaceful and never cried. Thankfully I supplemented her because it took five days for my milk to come in. Supplementing saved my breastfeeding journey, and we are still breastfeeding 19 months later.”
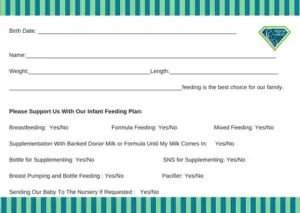
The first step is to review our safe infant feeding plan.

Our infant feeding plan provides detailed guidelines for safe breastfeeding. Countless families have told us they found confidence again with breastfeeding after using our infant feeding plan. You may print out a copy to bring to the hospital and share it with your medical providers. It’s a legal document like your birth plan and will be part of your medical records. It provides a link to the online resource tool called the NEWT (Newborn Weight Loss Tool) to track your newborn’s weight loss, so you will know if their weight loss becomes excessive even if you are supplementing after nursing.
What is the NEWT?

We recommend that parents practice using the NEWT tool before delivery to become familiar with how it works.
With the current breastfeeding protocol that hospitals use, 1 in 45 to 1 in 71 exclusively breastfed babies are rehospitalized from complications of insufficient milk intake, namely from delayed onset of or low milk production. These complications are life-threatening and are very easy to prevent with temporary supplementation.
This NEWT graph is an example of an exclusively breastfed baby that was rehospitalized from insufficient breastfeeding.

According to the NEWT graph, this baby had excessive weight loss, even though it was within the 7–10% weight loss range deemed acceptable by the AAP. As you can see, the baby’s weight loss was excessive. This baby’s rehospitalization could have been avoided if lactation and medical providers had used this tool and supplemented the baby to protect them. You can learn more about this baby here.
The second step is to be informed of your risk factors for delayed onset of full milk production, chronic low milk supply, or overt lactation failure.
Each pregnancy and delivery has different risk factors for timely full breast milk production. Mothers are not told that delayed onset of copious milk production is common. This research suggests that the prevalence of delayed onset of lactogenesis II (milk coming in) has reached epidemic proportions in the United States.
Looking at a list of risk factors might be overwhelming, but no matter your risk factors, risk only means a problem might happen, not that it will. However, you will be prepared this time and know how to keep your baby safe following our supplementing/feeding guidelines.

The third step is to know how much to supplement your baby.
Feeding/supplementing amounts are based on your baby’s birth weight and if they are full-term babies. On day 1, most babies are very sleepy and enter a deep recovery sleep for about 8–12 hours. Sometimes, they won’t be interested in taking a full feeding and it will be challenging to keep them awake. If this happens, do not panic. Simply self-express and supplement your baby.
Feeding Volume Guidelines
- On day one, expect your baby to feed 60–80 ml/kg/day (typically 15–30 ml) every 2–3 hours.
- On day 2, expect about 20–40 ml every 2–3 hours.
- On day 3, expect about 25–50 ml every 2–3 hours.
| Small to average-sized infants may take 15–30 ml (0.5–1 ounce) per feed, usually every 3 hours. It’s normal to take different amounts at each feeding. Always follow their hunger cues and feed on demand. |
What about the newborn stomach size?
The infant’s stomach size is not 5–7 ml as currently taught and is based on research from 100 years ago! The current research tells us a full-term baby’s stomach size is about 20–30 ml.

Facts about the newborn stomach:
- The newborn stomach is a highly elastic organ, expanding four times its size; its biological purpose is to hold food and fluids when eating a meal.
- The food and fluids held in the stomach are continuously emptied into the small intestine to absorb nutrients.
- Your term baby has been swallowing large amounts of amniotic fluid (500–1,000 ml) each day, and their stomach is quite accustomed to expansion after drinking the amniotic fluid.

- It is a myth that a baby’s stomach is permanently “stretched-out” when they are fed according to their caloric requirements and hunger cues. The stomach doesn’t “magically grow” on day 3 when your milk comes in.

Is it true my baby will not tolerate formula supplementation and spit up the formula?
No. All babies have extra spit-up during the first days of their lives, no matter how they are fed. Spit-up is from the amniotic fluid that remains in their stomachs if it wasn’t squeezed out during delivery. Spit-up is often mixed with colostrum or formula in the stomach from feeding. Cesarean section babies usually have more spit up because their stomach contents were not squeezed out during birth.
This is why a bulb syringe is available for babies who may need assistance with oral suctioning from stomach contents being spit up during the first days of life. Babies who are supplemented with volumes higher than recommended amounts can have extra spit-up.
Step 4 is how to supplement your baby.
You may supplement your baby using a bottle, a syringe at the breast, a tube at the breast, a spoon, or a cup. The first two options are the most efficient. There is no evidence that nipple confusion occurs when supplementing with a bottle.

Pasteurized Donor Milk for supplementing
If you prefer to supplement with pasteurized donor milk, check with your hospital about availability during your hospital stay. If it’s unavailable, in some cases, community milk banks have donor milk available to purchase in the hospital and when at home until your milk supply is sufficient. Click here to contact a milk bank.
Ready to feed infant formula
There are only a few brands of infant formula available in ready-to-feed bottles. You have the option to change the formula brand when you get home to a more affordable type for your baby when supplementing. Some brands of formulas promote their product specifically for supplementing, but it’s not necessary and is a marketing strategy. Most babies do well on standard infant formula.
* Note: For families who have a positive family history of atopic disease/allergies/asthma, it may be best to supplement with a hydrolyzed or elemental formula to reduce those risks.
The fifth step is managing and maximizing your milk supply during supplementation.
Despite a large amount of misinformation about supplementation that tells mothers it will interfere with their milk supply production, this is simply not true if you follow these simple steps.
- If your baby is nursing well on both breasts and you plan to supplement until your milk comes in, you will not have to hand express or pump for extra stimulation. “Nursing well” means vigorously sucking on each side for at least 15 minutes, about every 3 hours, with a good latch. Simply supplement after each nursing session.
- If your baby is not nursing well, they will need to be supplemented, and your breasts need to be stimulated and emptied to produce milk. You may feed your baby whatever colostrum you obtain from self-expressing or pumping.
| Every time your baby is supplemented, you must self-express and/or pump both breasts to empty them and signal the milk-making hormone cascade to produce milk. |
The sixth step is to reach out to your hospital and health care provider well before birth to ensure they will support your feeding plan.
- Talk to your OB or CNM about your feeding plan and have them write specific instructions on your medical records to inform the staff you will be breastfeeding and supplementing your baby.
- Call the birthing unit at the hospital and speak to the nurse manager to ensure your infant feeding plan will be honored. Ask them if they support your supplementing choices and provide infant formula when requested, without requiring you to sign a consent form or be educated on the “risks” of using it. You may also ask for an email address for the unit manager to discuss your infant feeding plan.
- Inform your pediatrician about your plan to supplement your baby. You can provide them with a copy of your feeding plan, too.
- If you do not want a lactation consultant to visit you, tell the manager and use one of our door signs included in the feeding plan. Let the staff know if you would like help from a lactation consultant with positioning and latching.
- If anyone shames you for formula feeding, report them immediately. Ask to speak to the nurse manager; if they are unavailable, call the hospital operator and ask to communicate with the hospital nursing supervisor. They will talk with you about your concerns.
- Please fill out your discharge survey to provide feedback about your feeding experience. Provide as many details as possible, negative and positive.
Things to bring with you
Bring infant formula nursette bottles and individually packaged bottle nipples to the hospital.
Parents told us their requests for infant formula were delayed or denied, violating your and your baby’s legal rights. You will need to purchase ready-to-feed formula bottles that come prepared in 2-ounce bottles. It’s the safest type of formula to feed your newborn while in the hospital. You will also need to buy nipples that are individually packaged, sterilized, and ready to twist onto the bottle to use. Please remember that these bottles and nipples are single-use only and must be discarded after use. Bring your own pacifier if you want to use one.
“Mothers, especially first-time mothers, had told us that they gave up breastfeeding the days after birth because they felt that they were not making enough milk when their milk arrival was simply delayed. If mothers were educated about their risk factors for delayed onset of milk or insufficient milk supply, how to safely supplement while waiting for their milk to come in, how to increase their milk production, or how to sustain a combo-feeding relationship if their supply is limited, they could go on to have a sustainable breastfeeding relationship instead of losing confidence and stopping breastfeeding altogether.”
—Jody Segrave-Daly, MS, RN, IBCLC
Fed Is Best Foundation
Additional resources
Join our Facebook support group by clicking here.
I Supplemented My Baby Until My Milk Came In And We Are Still Breastfeeding At 3 Months
https://www.nytimes.com/article/breastfeeding-newborn.html
https://fedisbest.org/resources-for-parents/feeding-plan/
https://fedisbest.org/resources-for-parents/newborn-weight-loss-calculator/
https://fedisbest.org/resources-for-parents/the-newborn-stomach-size-myth-it-is-not-5-7-ml/
https://fedisbest.org/resources-for-parents/cluster-feeding-normal/
https://fedisbest.org/resources-for-parents/second-night-syndrome-abnormal/

Supplementing Resources: https://www.cdc.gov/nutrition/infantandtoddlernutrition/formula-feeding/how-much-how-often.html
Ref: T. Gomella Neonatology: management, procedures, on-call problems, diseases, and drugs 6th ed.

8 thoughts on “How To Prepare For Supplementing When Breastfeeding Your Baby In The Hospital”