By: Michelle Klimczak, Registered Nurse, Population and Public Health, with a focus on health equity.
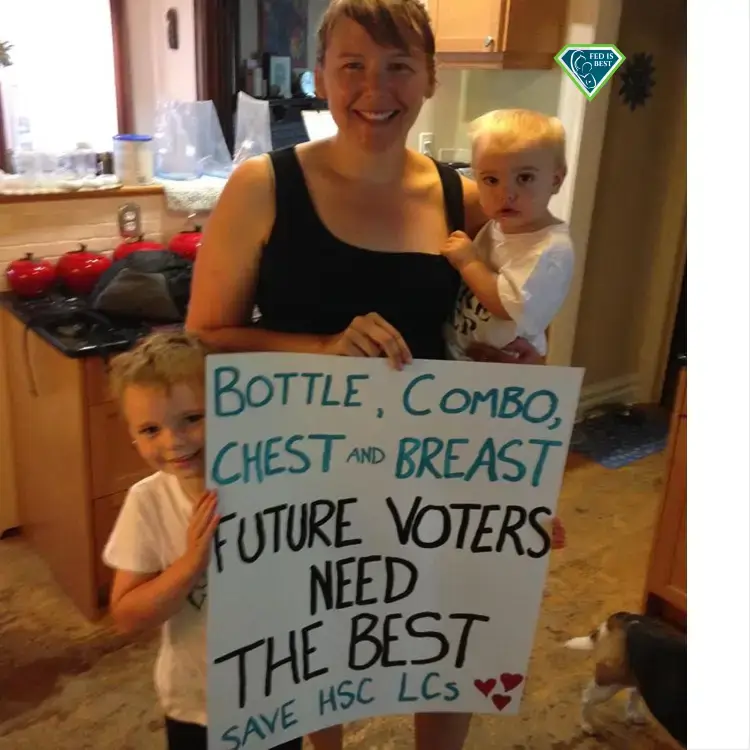
We frame infant feeding success as exclusive breastfeeding, so maybe it’s surprising that I got support with formula feeding through local lactation consultants? In fact, I think the support they offered was exactly the kind of compassion, kindness, and respect that new moms deserve. It’s possible to be inclusive.
When our fourth baby arrived we knew our family was complete, and so I’ve savored every milestone even when it feels a bit bittersweet. He just passed 18 months so a lot of the baby stuff that all 4 of my kids used is now packed up. It’s amazing to think of how I agonized over decisions about strollers and car seats and now those things are just “stuff”. It’s amazing too to think of what was meaningful, like what was actually good advice, what was actually helpful, what was actually supportive. These conversations about support are undoubtedly well-intentioned, but I learned time and time again that there are all kinds of ways to find support for a specific version of mothering, but not much widely available when you don’t match up to that version.
That “version” is largely reflective of the kind of mothering that happens when you have the privileges of wealth, and education, and an able-body, food and water security, and the social status that comes with a hetero-normative/traditional family structure. When you have those privileges, your baby has a pretty good chance of having good outcomes, and so by and large, we try to carry out the practices associated with that version of mothering.
So what happens if you can’t “do the thing”? Well, given that I hold all the privileges I talked about above, it’s quite likely that I never would have had a clue, and could have ascribed my own kids’ greatness to my practices rather than my privileges. But, life has had a way of teaching me big, humbling lessons and as it turns out, it wasn’t that I needed support to do the “right” thing but I did need support (and lots of it) to figure out how to do things differently. All four of my kids were by-and-large formula fed. I desperately wanted to breastfeed because that’s “the thing” but it just wasn’t in the cards. No amount of support would have changed something I couldn’t physically do. The support I needed (and was so lucky to find) helped me figure out the practicalities of feeding and feeling successful.

Tube feeding my baby formula was the best I could do.
It’s tricky though because I think there’s a general impression that feeding supports should exist to minimize formula use, not support it.
Continue reading →