by Alexandria Fischer, PhD candidate at the Rensselaer Polytechnic Institute, studying synthetic microbial communities
It’s a mantra we have all heard, on repeat. “Breast is best.” But what does that really mean? Moms are bombarded by messages about the benefits of breastfeeding, such as increased intelligence, less illnesses, and a decreased risk of cancer. But what mothers are not told, is the quantifiable proof of these benefits.
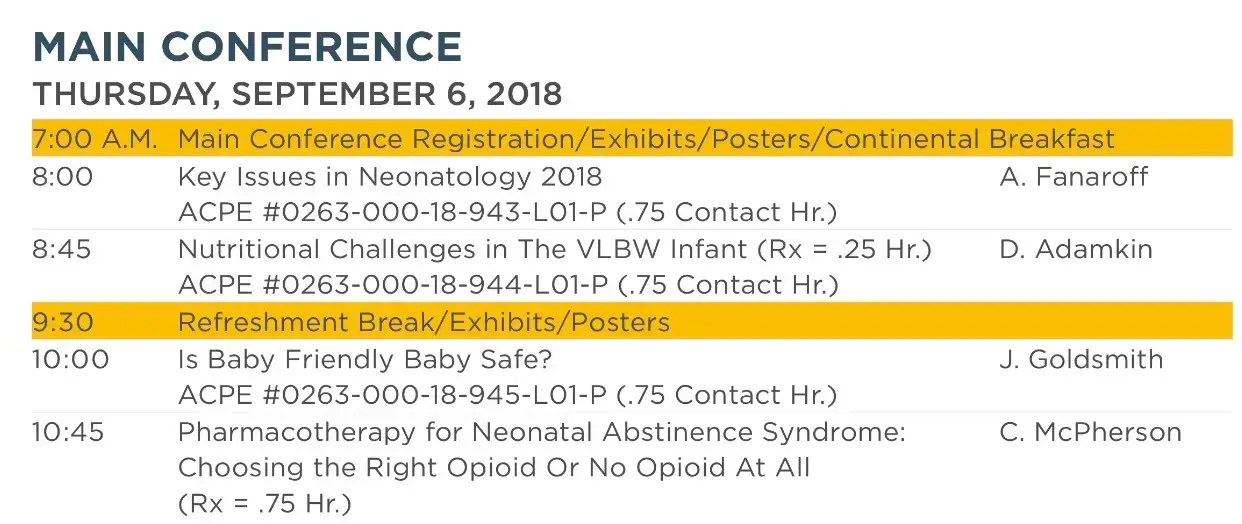
The paper “Is the “breast is best” mantra an oversimplification?“, published in the Journal of Family Practice in July 2018, sought to critically evaluate claims of breastfeeding benefits in an effort to truly understand them. These authors note that the same data has produced a wide range of conclusions about the reported benefits of breastfeeding. They sought to tease apart what variables were truly impacted, and which were not. In this review the authors determined the number needed to treat (NNT) for a myriad of health issues that are often claimed to be reduced by breastfeeding. The NNT simply means how many babies need to be breastfed in order for one baby to benefit. We need to use caution when examining NNTs because they cannot make a causal determination, meaning they cannot be used to say “breastfeeding prevented this infection” they are simply used to determine a correlative relationship.
“The NNT (numbers needed to treat) simply means how many babies need to be breastfed in order for one baby to benefit.”