By the Senior Advisory Board of the Fed is Best Foundation
A key recommendation of the 1989 World Health Organization Ten Steps to Successful Breastfeeding which guides the Baby-Friendly Hospital Initiative (BFHI) is: “give infants no food or drink other than breast-milk, unless medically indicated.” This has led to serious complications from accidental starvation of babies, including dehydration, hyperbilirubinemia (jaundice) and hypoglycemia (low blood sugar) — known causes of infant brain injury and permanent disability. Last week, the WHO issued draft revised breastfeeding guidelines, failing to revise this recommendation. These guidelines define the standard of care for breastfeeding management in all healthcare facilities worldwide. Nearly 500 U.S. hospitals and birthing centers and thousands more worldwide that meet the criteria of the BFHI are certified as Baby-Friendly, adhering to the application of the WHO’s Ten Steps.
On Sept. 22, 2017, senior members of the Fed is Best Foundation, and guests including a neonatologist from a leading U.S. tertiary care hospital and a pediatric endocrinologist, Dr. Paul Thornton, M.D, from Cook Children’s Hospital Fort Worth, lead author of the Pediatric Endocrine Society’s newborn hypoglycemia guidelines, met via teleconference with top officials of the WHO Breastfeeding Program: Dr. Laurence Grummer-Strawn, Ph.D., Dr. Nigel Rollins, M.D. and Dr. Wilson Were, M.D. to express their concerns about the complications arising from the BFHI Ten Steps and to ask what, if any, monitoring, research, or public outreach the WHO has planned regarding the risks of accidental starvation of exclusively breastfed newborns. The Foundation members who attended were 1) Christie del Castillo-Hegyi, MD, Co-Founder, 2) Jody Segrave-Daly, RN, IBCLC, Co-Founder, 3) Julie Tibbets, JD, Partner at Alston & Bird, LLP, Pro-Bono Attorney for the Foundation, 4) Brian Symon, MD, Senior Advisor, and 5) Hillary Kuzdeba, MPH, former quality improvement program coordinator at a children’s hospital, managing infant feeding projects and Senior Advisor.
Emails confirming meeting between the WHO and the Fed is Best Foundation available here.
The WHO officials reported that they have not specifically studied the complications from exclusive breastfeeding and have no studies or grants commissioned to monitor complications of the BFHI. The WHO officials said that it convened a group of global infant nutrition experts, last year to review and revise its guidelines, but no one on the panel raised the issue of complications as a priority for discussion. Unfortunately, none of the experts were experts in breastfeeding complications or newborn brain injury. The WHO officials indicated being close to the end of the BFHI guideline revision process before final publication. The current draft revision does not include recommendations for educating mothers on the risk factors, signs and consequences of starvation from exclusive breastfeeding nor make mention of the prevention of brain injury and disability as the “medically necessary” rationale for supplementation.
Dr. Christie del Castillo-Hegyi, co-founder of the Foundation, presented data on the high rates of starvation-related complications from research conducted at BFHI-certified hospitals and the permanent disabilities that result.
Highlights from the presentation include:
- 10% of vaginally-delivered and 25% of cesarean-delivered exclusively breastfed (EBF) babies born at a BFHI hospital lose excessive weight of >10% in the first days of life.[1]
- 10-18% of exclusively breastfed newborns experience “starvation jaundice” from insufficient milk intake, according to the Academy of Breastfeeding Medicine jaundice protocol.[2]
- Jaundice, the majority from dehydration/underfeeding in exclusively breastfed newborns (approximately 86%) is the leading cause of newborn rehospitalization in the U.S. and in the rest of the world and is a leading cause of perinatal disability.[3, 4, 5]
- Phototherapy-requiring jaundice increases the risk of long-term developmental disabilities including ADHD, cerebral palsy, seizure disorders, lower academic achievement and deficits in language, auditory, visual, sensory, motor, behavioral and cognitive deficits known as Bilirubin-Induced Neurological Dysfunction. [6-10]
- 10% of well-monitored exclusively breastfed babies undergoing the BFHI protocol develop hypoglycemia of less the 40 mg/dL within the first 48 hours. This rises to 23% in babies born to first-time mothers.[11]
- A glucose of less than 46 mg/dL within the first 24 hours of life has been associated with a 3.7- fold increased risk of brain injury on MRI and a 4.8-fold increased odds of lower motor, cognitive and language scores at 1 year of age.[12]
- Cognitive impairment can have lifelong effects as evidenced by a study of 1395 newborns showing that newborns who develop hypoglycemia of less than 40 mg/dL within the first hours of life had a 50% reduction in passing their fourth-grade proficiency test in literacy and math. A glucose less than 45 mg/dL resulted in a 38% reduction in passing the literacy test. Impairments persisted despite aggressive correction of the hypoglycemia. [13]
- 22% of motivated mothers intending to exclusively breastfeed who receive close lactation support experienced delayed onset of copious milk production which put her child at a 7-fold increased risk of excessive weight loss greater than 10%.[14]
- Exclusive breastfeeding at discharge has been associated with an 11-fold higher risk of rehospitalization for underfeeding and dehydration.[15]
- 95% of hypernatremia, a form of severe dehydration that causes brain injury and increased mortality, occurs by 7% weight loss and at this time, over half of exclusively breastfed babies from a BFHI hospital lose greater than 7%.[16,1]
- 10.1% of babies born to one BFHI hospital system were hospitalized for phototherapy, over 10,000 babies in 3 years.[17]
- 1.1 million newborns a year develop severe jaundice. 114,000 of those newborns a year will die from that severe jaundice, the majority in resource-poor countries with insufficient healthcare resources to monitor the complications of exclusive breastfeeding.[18]
A video of the presentation provided to the WHO officials can be viewed here:
References for presentation can be found here.
A PDF of the full presentation is available here.
Dr. del Castillo-Hegyi concluded,
“The pressure to achieve exclusive breastfeeding is contributing to an epidemic of infant feeding complications, preventable hospitalizations, unrecognized brain injury, lower academic achievement and long-term disability. Publicly acknowledging the common problem of insufficient breast milk and the importance of supplementation to protect the brain can prevent millions of complications, hospitalizations and newborn injuries. We are asking the WHO to assist us in making infant feeding safe for all infants by ensuring that all babies have access to enough milk to preserve the integrity of their brain and vital organs. Being fully fed is a basic human right that is not currently met by the standard of care.”

Provided by Hanna Awadzi, pictured in photo. Hannah Awadzi is a professional journalist from Ghana whose first-born daughter Avery suffered from severe starvation-related jaundice and hypoglycemia while exclusively breastfeeding with insufficient milk. Hannah was not advised to supplement despite her daughter developing a severely high bilirubin of 30 mg/dL and glucose level of 9 mg/dL by day 11. Avery subsequently developed cerebral palsy. Bilirubin toxicity and hypoglycemia are known causes of brain injury and cerebral palsy. Avery is one of thousands of children in Ghana who has developed cerebral palsy from severe jaundice. Hannah has documented the struggle of families with children with CP in this video.
In the meeting, the neonatologist in attendance provided an account of what neonatologists are seeing with the BFHI. She described her last three days as a neonatologist taking care of a child in follow-up clinic who had developed starvation-related hypoglycemia from insufficient feeding due to exclusive breastfeeding. This newborn developed intractable seizures and brain injury on MRI to the occipital lobes. The next day, she took care of a newborn who suffocated within the first hour of life while doing unsupervised skin-to-skin with a mother recovering from a c-section. This child required full resuscitation and survived the incident requiring intensive care. Lastly, she described taking care of the more typical case of a newborn losing greater than 10% of their birth weight and developing severe jaundice by the third day of life, discovered at the pediatrician’s office, thus requiring readmission for phototherapy. In discussion with dozens of neonatologists regarding their experiences with the BFHI she stated the following,
“Neonatologists are seeing these cases almost every day every where around the country. The focus is only on the number of women who are exclusive breastfeeding at discharge and not at all on safety; that is the core measure and that’s it.”
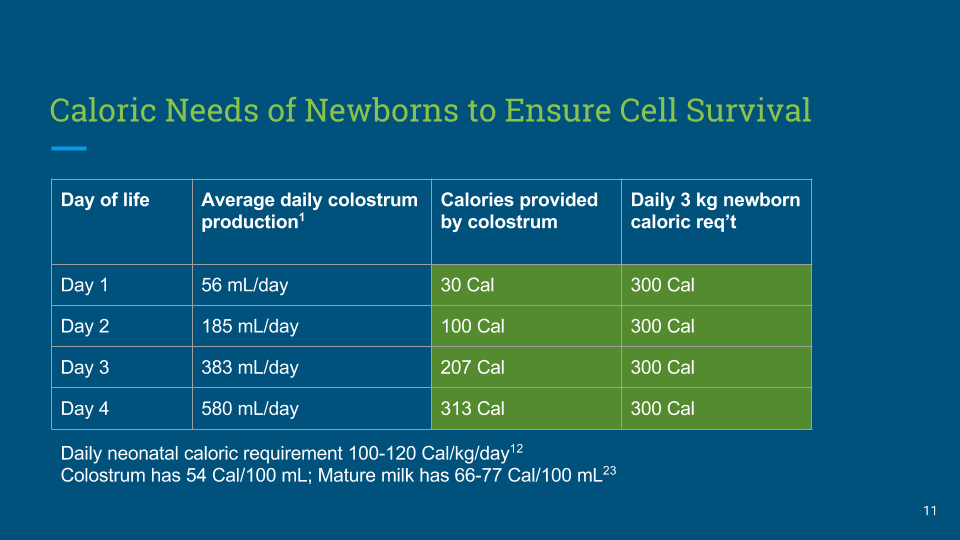
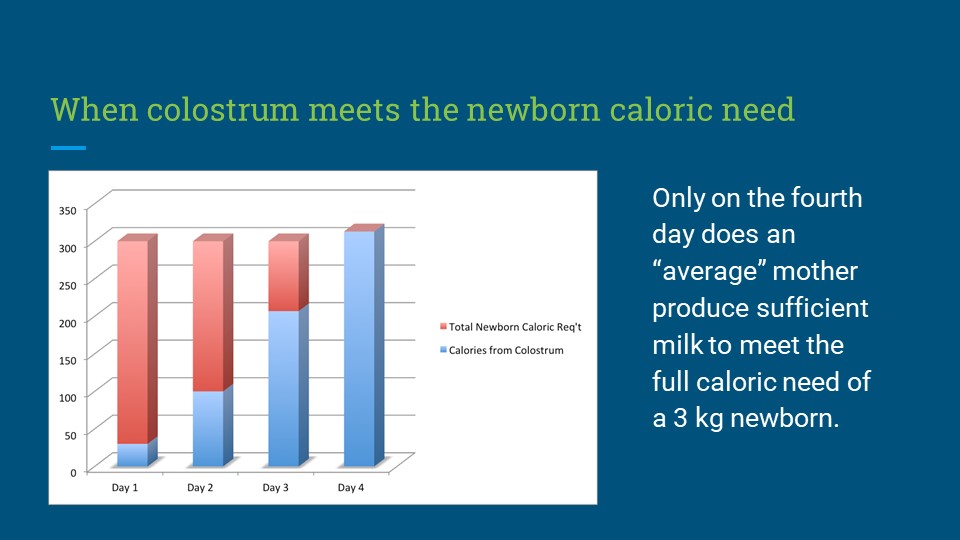
Nurses and physicians who have expressed their grievances with the BFHI to the Foundation have reported these complications arise due to the guidelines’ quality metric goal of high exclusive breastfeeding rates at discharge, which puts pressure on health professionals and mothers to avoid supplementation, even when there is evidence of insufficient breast milk and newborn hunger from exclusive breastfeeding. Furthermore, breastfeeding mothers are commonly told upon discharge from the hospital to avoid supplementation even before they produce sufficient milk to provide the full caloric requirement of a newborn. The starvation-related complications can quickly result in brain injury, permanent disability and rarely, death if a child does not receive supplemental milk before reaching a critical threshold.
Dr. Brian Symon, MD a General Practitioner from Adelaide, Australia whose practice focuses on newborn and infant care offered his experience with the Baby-Friendly protocol in Australia. He described in the meeting having developed a protocol early in his practice in a country community with a large Aboriginal population offering supplementation to breastfed newborns the first days of life until a mother’s full breast milk supply was sufficient to satisfy the baby. He reported excellent outcomes with continued breastfeeding rates of 75% at 12 weeks compared to 50%, which was then the national average. Furthermore, he reported, in the 17 years of practice in that community using this protocol, he did not admit a single newborn for jaundice in order to provide phototherapy. Once he came to the city where the Baby-Friendly protocol was used, “it was a completely different world.” He reported babies were regularly losing 5-12% of their birth weight.
“Mothers were tearful, exhausted, nipples were bleeding, and babies clearly weren’t doing well, needing admission for phototherapy.” He said it was very clear that there was something wrong with patient management. He closed his statement by saying, “I would argue in any forum that breastfeeding success rates could be increased by the appropriate use of supplementation, in particular in those early transition days until the mother’s lactation has been established.”
Dr. Thornton, pediatric endocrinologist also provided the WHO directors his perspective on the Baby-Friendly guidelines. He stated,
“It is known that newborns have a short period of time where there is a drop in the glucose to a mean glucose of 56 (mg/dL) in the first hours of life, even as low as a glucose of 30. In the past, doctors have thought that to be benign.” He stated, “the recent paper [published in JAMA Pediatrics] where [the study investigators] screened blood glucose in all babies and looked at long-term outcomes is a little concerning.”[13]
This paper showed 50% declines in the ability to pass 4th grade standardized tests in literacy and math in newborns developing glucose levels of 40 mg/dL and below within the first 3 hours of life, even with aggressive correction. Passing rates in the literacy test were 38% lower in newborns developing glucose levels below 45 mg/dL. At this time, 10% of all exclusive breastfed newborns develop hypoglycemia below 40 mg/dL, which rises to 23% in first-born exclusively breastfed newborns.[11] He noted,
“There is data out of New Zealand, the CHYLD study, that shows that in at-risk babies [for hypoglycemia], we are seeing some poorer outcomes. As a pediatric endocrinologist, in my practice, when a breastfed baby is supplemented with glucose gel or formula, I do not see that as a contributor to breastfeeding failure.” He believed, “it might be important to discuss what the risks are and when ’medical necessity’ occurs and how proper supplementation can minimally affect long-term breastfeeding rates. I think the idea that you put one bottle in the mouth and they are done with breastfeeding is not really true.”
Dr. del Castillo-Hegyi asked the WHO directors, “Are there any plans within the WHO to inform mothers of the risks of brain injury from insufficient breast milk in order to make sure that they are aware when a child is critically ill at home, that supplementation can protect their child from brain injury?”
Dr. Rollins responded, “That specific recommendation was not identified by [our] experts as a top priority.” Dr. Rollins acknowledged that the WHO is aware of the complications, stating that the guidelines do include danger signs, such as “convulsions, being lethargic and not being able to feed,” to alert healthcare providers to intervene.
However, according to the clinical evidence presented, those signs signify that brain injury is already present.[13,17,18] The BFHI guidelines, as written by the Academy of Breastfeeding Medicine, require informing patients of the risks of formula, but do not require health workers to inform parents of the risks of hospitalization or brain injury from avoiding supplementation while exclusively breastfeeding. The guidelines offer no patient education on these danger signs for when critical conditions requiring supplementation occur at home.
Dr. del Castillo-Hegyi, MD offered the services of members of the Fed is Best Foundation and other recruited experts in this field to the WHO directors in order to increase attention within the revised guidelines on prevention of complications, patient education on the signs of newborn hunger and critical illness and the role of supplementation in preventing brain injury in underfed breastfed newborns. The WHO officials stated that the revision process was well underway and that it was too late in the process to accept any new experts for this round of revisions. The officials did ask for a copy of the presentation given by the Foundation along with the list of supporting peer-reviewed references. They stated that experts present at the meeting may be invited for future revisions of the guidelines, although they noted the next cycle of revisions may be a few years away.
In response to this news, Jillian Johnson, a mother and advocate whose newborn son Landon died five years ago from complications of starvation at a BFHI hospital states,
“I am appalled by the lack of concern shown by the WHO regarding such an important issue. I shared with the world the pain of losing my son by a senseless practice and they aren’t interested in preventing it from happening to other families.”
The Fed is Best Foundation has grave concerns about the safety of the WHO BFHI guidelines. The Foundation is deeply concerned that the secretariats of the guidelines are aware of the safety issues, namely the potential for brain injury and disability, and yet are unwilling to inform the public about these complications that can be prevented with guidelines that require monitoring of newborns for signs of hunger, supplementation of breastfeeding when those signs are present, and education of new parents and professionals regarding the risks of newborn hunger and its outcomes. This fails to meet the core obligations of health professionals and health organizations to provide patients full disclosure of risks and benefits of health care decisions, including those of exclusive breastfeeding, particularly in the days before full production of breast milk. We are disappointed that the WHO has not placed priority on reducing the incidence of preventable complications and has not investigated the clinical evidence in this area, including the expected prevalence of brain injury and developmental disability associated. We feel that the WHO’s attempt to prevent these complications, which consists of merely telling health care workers to look out for signs of newborn distress, including “convulsions, lethargy and not being able to feed,” late signs of newborn brain injury, is grossly inadequate. Furthermore, not informing mothers about the possibility and the signs of infant starvation can put a child in danger once the family is released from medical care.
Dr. Thornton commented after the meeting,
“We agree that it is important to support mothers who wish to breastfeed and whose realities make optimal management of breastfeeding critical in promoting infant health. But starving a small percentage of breastfed babies out of the misguided opinion that properly managed supplemental feeds will interfere with breastfeeding is wrong. We support supplemental feeds when babies are showing signs of distress or to prevent medical harm.”
Our Foundation, health professional supporters and the affected families we represent feel that this is a serious failure of the WHO to meet the basic obligations of health professionals to act in the best interest of patients, to do no harm and to respect the autonomy and human rights of mothers and babies all around the world. The complications of the Baby-Friendly protocol costs the U.S. health care system millions of dollars in neonatal hospital admission every year, an estimated $49 million a year for just one Baby-Friendly hospital system in phototherapy admissions alone based on recent published data and data from the American Hospital Association on the average cost of such admissions. The cost of care for previously healthy newborns who sustain brain injury or medical complications from the Baby-Friendly protocol can amount to millions per child over their lifetime.
It is the opinion of The Fed is Best Foundation that the World Health Organization has failed to collect the necessary expertise and has failed to research the most basic information on the minimum requirements of newborns and the caloric yield of their protocol to ensure infant safety in the BFHI. We recommend that the United States and all other countries who want to ensure infant health and safety and to reduce the health care costs of preventable newborn hospitalizations and lifetime care for accidentally starved brain-injured newborns disengage from the BFHI. Decades of peer-reviewed literature has documented the safety issues of the Baby-Friendly protocol, including higher rates of hyperbilirubinemia, dehydration and hypoglycemia in exclusively breastfed newborns, all of which can cause mild to severe brain injury, lower academic achievement and developmental disability. The methods of the BFHI to gain compliance from patients constitute clear violations of a patient’s rights to complete and honest information regarding risks. Finally, it unacceptable for a health policy to require children to endure days of hunger and thirst in order to achieve high exclusive breastfeeding rates, a routine practice of the Baby-Friendly protocol. In fact, the calculated caloric allowance of the Baby-Friendly protocol makes it a violation of the United Nation’s Declaration of Human Rights protecting a person’s right to food and water.
We hope health facilities and health providers all around the world choose to adopt safer, more individualized and humane infant feeding practices. We hope that evidence-based policies on infant feeding change from prioritizing exclusive breastfeeding rates to prioritizing infant safety by ensuring delivery of sufficient calories and fluid to protect the integrity of the brain and vital organs, a standard that is not guaranteed by the BFHI. The Fed is Best Foundation has extensive resources for health providers and families to help them ensure safe feeding of infants at https://fedisbest.org/resources-for-parents/. We believe the current standard of care allows unacceptable complications to occur routinely and we cannot allow the system that creates these complications to continue unchecked.
Patient safety is paramount and the BFHI not only fails to guarantee safety but actually increases serious and preventable complications. You cannot implement any policy in medicine without extensive safety data. Then as you implement policies, the expectation is that you collect data to analyze within your institution to confirm positive outcomes and no increased morbidity and mortality while implementing the policy. The best policies are constantly changing based on newest literature and data. Neither exists for the BFHI as we have learned from our meeting. This implies that the policy is flawed and does not meet the local, national or global standards to stand as the gold standard of practice.
The WHO is accepting comments on these draft guideline revisions until October 24, 2017. The Foundation urges health care providers, parents, and the public to demand that the WHO not place exclusive breastfeeding before infant safety in their guidelines and commit to informing parents of the real risks of insufficient feeding. Comments can be made on the WHO BFHI comments page or emailed to [email protected], to be forwarded to the WHO.
Send Comments to WHO before Oct 24Please sign this petition to demand that the WHO make preventing newborn brain injury and death from their breastfeeding guidelines a priority.
Sign Our WHO PetitionThe Fed is Best Foundation’s full critique of the Academy of Breastfeeding Medicine WHO BFHI supplementation guidelines has been submitted to the WHO and can be found here.
Update on Final Draft Revision of WHO BFHI guidelines
The WHO released their final draft revision of the BFHI Guidelines several weeks after the publication of this post. It can be found here. Sadly, they made no changes to the least safe guideline Step 6: “Give no food or water other than breast milk,” yet provided no scientific evidence showing that supplementation had any causal relationship to failed breastfeeding. In addition, no mention of the risk brain injury or disability were made with regard to breastfeeding complications
References:
[1] Valerie J. Flaherman, MD, MPH, et al., Early Weight Loss Nomograms for Exclusively Breastfed Newborns, Pediatrics, 2015 Jan; 135(1): e16–e23.
[2]] ABM Clinical Protocol #22: Guidelines for Management of Jaundice in the Breastfeeding Infant Equal to or Greater Than 35 Weeks’ Gestation, The Academy of Breastfeeding Medicine Protocol Committee, Breastfeeding Medicine, Vol. 5(2):87-93.
[3] Janet H. Muri, et al. From the American Hospital Association: Reducing Avoidable Obstetrical and Neonatal Readmissions http://www.aha.org/content/11/PerinatalReadmissionscall1.pdf
[4] Lee BK, et al. Haemolytic and nonhaemolytic neonatal jaundice have different risk factor profiles. Acta Paediatr. 2016 Dec;105(12):1444-1450.
[5] Olusanya BO, Osibanjo FB, Mabogunje CA, Slusher TM, Olowe SA. The burden and
management of neonatal jaundice in Nigeria: A scoping review of the literature.
Niger J Clin Pract. 2016 Jan-Feb;19(1):1-17.
[6] Wei CC, et al. Neonatal jaundice and increased risk of attention-deficit hyperactivity disorder: a population-based cohort study. J Child Psychol Psychiatry. 2015 Apr;56(4):460-
[7] Maimburg RD, Olsen J, Sun Y. Neonatal hyperbilirubinemia and the risk of
febrile seizures and childhood epilepsy. Epilepsy Res. 2016 Aug;124:67-72.
[8] Hamdy NE, et al. Cerebral palsy in Al-Quseir City, Egypt: prevalence, subtypes, and risk factors. Neuropsychiatr Dis Treat. 2014; 10: 1267–1272.
[8] Hokkanen L, Launes J, Michelsson K. Adult neurobehavioral outcome of
hyperbilirubinemia in full term neonates-a 30 year prospective follow-up study.
PeerJ. 2014 Mar 4;2:e294.
[9] Wusthoff CJ, Loe IM. Impact of bilirubin-induced neurologic dysfunction on
neurodevelopmental outcomes. Semin Fetal Neonatal Med. 2015 Feb;20(1):52-57.
[10] El Houchi SZ, et al. Prediction of 3- to 5-Month Outcomes from Signs of Acute Bilirubin
Toxicity in Newborn Infants. J Pediatr. 2017 Apr;183:51-55.e1.
[11] Purnima Samayam, et al., Study of Asymptomatic Hypoglycemia in Full Term Exclusively Breastfed Neonates in First 48 Hours of Life, J Clin Diagn Res. 2015 Sep; 9(9): SC07–SC10.
[12] Emily W.Y. Tam et al., Hypoglycemia is associated with increased risk for brain injury and adverse neurodevelopmental outcome in neonates at risk for encephalopathy, J Pediatr., 2012 Jul; 161(1): 88–93.
[14] Dewey KG, et al., Risk factors for suboptimal infant breastfeeding behavior, delayed onset of lactation, and excess neonatal weight loss, Pediatrics, 2003 Sep;112(3 Pt 1):607-19.
[15] Escobar GJ, et al., Rehospitalization for neonatal dehydration: a nested case-control study, Arch Pediatr Adolesc Med., 2002 Feb;156(2):155-61
[16] Uras, et al., Moderate hypernatremic dehydration in newborn infants: retrospective evaluation of 64 cases. J Matern Fetal Neonatal Med. 2007 Jun;20(6):449-52.
[17] Seske LM, et al. Late-Onset Hypoglycemia in Term Newborns With Poor Breastfeeding. Hosp Pediatr. 2015 Sep;5(9):501-4.
[18] Olusanya BO, et al. Management of late-preterm and term infants with
hyperbilirubinaemia in resource-constrained settings. BMC Pediatr. 2015 Apr
12;15:39.


29 thoughts on “World Health Organization Revised Breastfeeding Guidelines Put Babies at Risk Despite Pleas from Experts—Informing the Public “Not a Top Priority””