Christie del Castillo-Hegyi, M.D.
The WHO health policy that has been responsible for millions of preventable hospital admissions of newborns for insufficient feeding complications is Step 6 of the Ten Steps to Successful Breastfeeding: “Give no additional food or fluid other than breast milk unless medically indicated.” Complications of insufficient feeding from exclusive breastfeeding before copious milk production are now among the leading causes of newborn extended and repeat hospitalization, namely jaundice (hyperbilirubinemia), dehydration and hypoglycemia.
In 2017, the World Health Organization published its guidelines updating its recommendations for “Protecting, Promoting and Supporting Breastfeeding in Facilities Providing Maternity and Newborn Services,” which outlines the evidence for the WHO recommendations on breastfeeding support for newborns in health facilities based on the Ten Steps to Successful Breastfeeding. Here is the evidence presented to justify the recommendation to avoid supplementation in breastfed newborns.
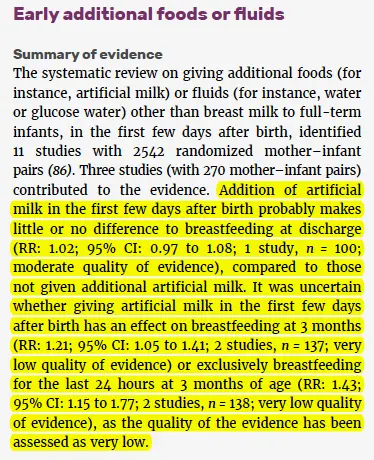
The WHO guidelines authors went on to conclude the following:
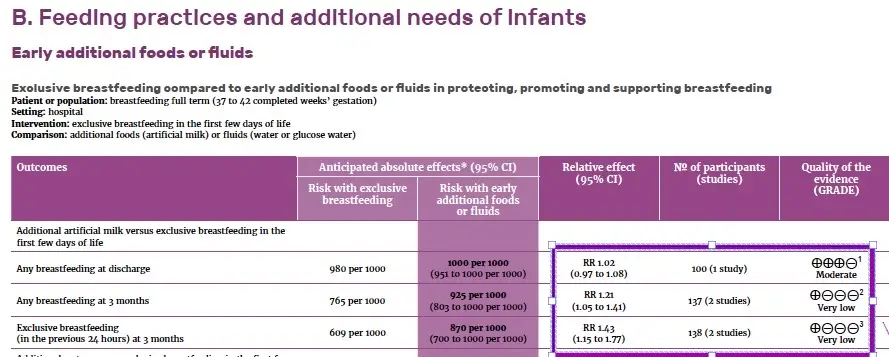
How did very low quality of evidence turn into moderate-quality evidence for exclusive breastfeeding particularly when the evidence showed improvement of breastfeeding rates in supplemented breastfed newborns?
What are the studies that were used to evaluate this evidence? They used a Cochrane Review, which is a type of study that takes all the relevant studies regarding a clinical question, puts them together and tries to come up with the best recommendation given the outcomes of those studies. This review looked at the differences between exclusive vs. non-exclusive breastfeeding on long-term breastfeeding rates and other effects on infant health. The only studies of adequate quality that could be included were by Flaherman et al. and Straňák et al. What that review said regarding “artificial milk” supplementation was the following:
“Providing breastfeeding infants with artificial milk, compared to exclusive breastfeeding, did not affect rates of breastfeeding at hospital discharge (risk ratio (RR) 1.02, 95% confidence interval (CI) 0.97 to 1.08; one trial, 100 infants; low-quality evidence).
At three months, breastfeeding infants who were provided with artificial milk had higher rates of any breastfeeding compared to exclusively breastfeeding infants (RR 1.21, 95% CI 1.05 to 1.41; two trials, 137 infants; low-quality evidence).
Infants who were given artificial milk in the first few days after birth before breastfeeding, had less “obvious or probable symptoms” of allergy compared to exclusively breastfeeding infants (RR 0.56, 95% CI 0.35 to 0.91; one trial, 207 infants; very low-quality evidence).
No difference was found in maternal confidence when comparing non-exclusive breastfeeding infants who were provided with artificial milk with exclusive breastfeeding infants (mean difference (MD) 0.10, 95% CI -0.34 to 0.54; one study, 39 infants; low-quality evidence).
All other studies in the published literature showing lower breastfeeding rates in supplemented newborns were retrospective, a type of study that can result in the mistaken belief that supplementation is the cause rather than the result of poor lactation. In other words, we know that mothers who don’t produce much breast milk are more likely to supplement with formula. One can mistakenly believe that the supplementation is causing the poor breast milk production when it is just as likely that the mom’s lower ability to lactate is the cause of supplementation. No study to date using the gold-standard of a randomized controlled trial has been published showing reduced rates of long-term breastfeeding with judicious formula supplementation.
Here are the same data in the updated WHO guidelines:
What was the effect of Giving complementary food to infants at 4 months versus 6 months?
According to the same Cochrane Review, exclusively breastfeeding until 6 months had the following effect on the following health outcomes. There were no differences in multiple health outcomes between starting solids at 4 months vs. 6 months. So for moms who feel like their infants are not satisfied by breast milk or formula at 4 months and your child is showing developmental readiness for starting solids (check with your doctor), starting at 4 months instead of 6 months is just fine. In fact, some mothers who have avoided solids until 6 months in order to follow the WHO exclusive breastfeeding rule, even when their infants were showing persistent hunger, have found their babies develop failure to thrive.
Infant Morbidity |
Starting solids at 4 months vs. 6 months |
| Fever (from 16-26 weeks) | No difference |
| Upper Respiratory Illness | No difference |
| Diarrhea | Less common with complementary feeding at 4 mo. |
| Food Allergies | No difference |
| Eczema | No difference |
| Food protein-induced enterocolitis | No difference |
| Anemia | No difference |
| Infant weight gain | No difference |
| Overweight at 18 – 38 months | No difference |
What Did the WHO committee decide to recommend based on the evidence?
Despite little to no differences in health outcomes, slightly increased long-term breastfeeding rates among formula-supplemented newborns and even evidence of harm (increased rates of allergies) from exclusive breastfeeding, the WHO breastfeeding recommendation still stands at—you guessed it—recommending exclusive breastfeeding to all babies from birth to 6 months. Despite providing this “very low quality” evidence that shows the opposite of their recommendation, they inexplicably say the following:
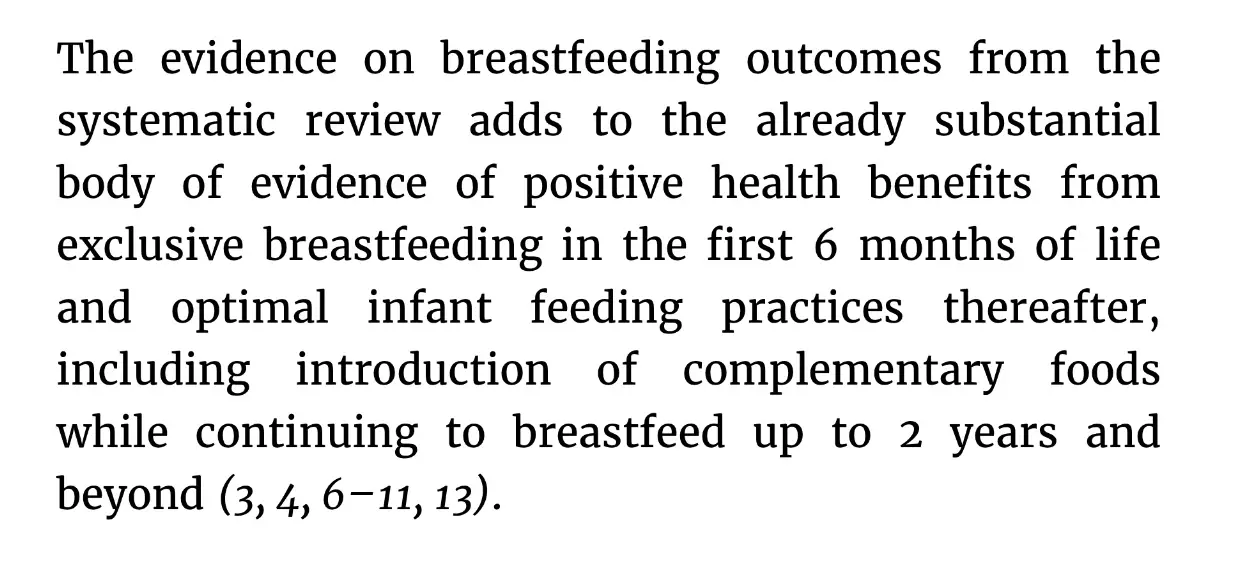
They provide evidence that there is no additional benefit from exclusive breastfeeding in comparison to non-exclusive breastfeeding while increasing an infant’s risk for harm from jaundice, dehydration, hypernatremia, hypoglycemia, and failure to thrive by continuing to recommend exclusive breastfeeding from birth to 6 months for all infants. They have no data on the number of mothers for whom exclusive breastfeeding from birth to 6 months is unsafe for their newborn. They provide no public health education on the common and serious consequences of exclusive breastfeeding with insufficient breast milk, strongly discourage supplementation that may, in fact, protect an infant’s brain and life, and fail to disclose the serious and irreversible health risks to newborns who are accidentally starved from exclusive breastfeeding.
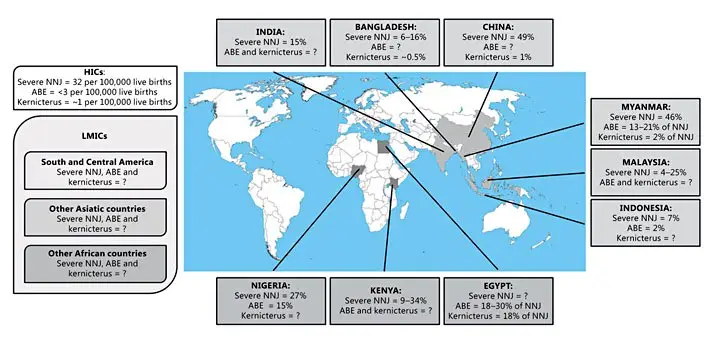
Incidence of severe neonatal jaundice (bilirubin ≥ 20 mg/dL) in Low- and Middle-Income countries. The data reported corresponding to hospital statistics. [Greco, et al, Neonatology 2016;110:172-180]

Jaundice from dehydration/underfeeding in exclusively breastfed newborns are among the leading causes of newborn hospitalization across the globe. Photo provided by Firefly.
What have we done?
Exclusive breastfeeding at discharge is the only quality metric measured by the Baby-Friendly Hospital Initiative. It has hospitalized millions of newborns for brain-threatening complications of jaundice, dehydration, and hypoglycemia, all preventable with donor breast milk or properly-prepared formula. It has created a global epidemic of newborn jaundice and dehydration hospitalizations that are contributing to an epidemic of cerebral palsy in the developing world and a still unmeasured epidemic of developmental disabilities among affected newborns even in places where safe breast milk substitutes exist. Meanwhile, by the WHO breastfeeding experts’ own criteria, the evidence supporting avoidance of formula supplementation in breastfed newborns until 6 months of age does not exist.
The World Health Organization has acknowledged the risk of brain injury from the exclusive breastfeeding guideline and yet has declined to inform the public of this risk. Nowhere in the entire updated WHO guidelines or the BFHI guidelines is there mention of brain injury or impaired brain development as the rationale for medically-indicated supplementation. Therefore, many health professionals are unaware of what they are protecting babies from, particularly those who are on the front line of monitoring newborns for complications like nurses and lactation consultants. From health professional reports and our review of the training modules, little to no education on the serious risks of brain injury and disability from jaundice, dehydration, and hypoglycemia is provided by the BFHI training program.
The Baby-Friendly guidelines have failed to protect babies from feeding complications by failing to adequately monitor glucose, sodium, bilirubin, and weight while discouraging supplementation for the most obvious signs of newborn starvation, namely persistent crying and nursing. Their updated supplementation guidelines recognize that evaluation must happen for persistent crying but provide no guidelines for laboratory evaluation to determine the need for rescue supplementation to prevent brain injury. Mothers have reported being denied formula supplementation in the hospital or discouraged from using it at home even when their newborns have exhibited these obvious signs and their babies were subsequently forced to develop feeding complications even to the point of brain injury and death. Mothers are sent home before they have sufficient breast milk to safely breastfeed exclusively while given no instruction on the signs and serious consequences of newborn starvation. For mothers whose milk does not come in time, their babies can be found lethargic and critically ill from feeding complications that would have been prevented with responsible and honest breastfeeding education as well as timely and adequate supplementation.
The ethical violations of the World Health Organization and the BFHI are unspeakable. Until the strict exclusive breastfeeding policy of the BFHI is amended, we strongly discourage mothers from delivering at BFHI-accredited hospitals. Those who wish to breastfeed, we encourage you to prepare by:
- watching instructional videos on the latch and manual expression of breast milk
- employing the help of health professionals trained in breastfeeding who will respect your feeding choices and your baby’s right to be safely fed
- discussing your feeding plan with your pediatrician and obstetrician before delivery
- learning the signs of a HUNGRY breastfed newborn
- learning methods of supplementation to prevent feeding complications while maintaining breast milk supply in case breastfeeding is inadequate to meet your infant’s full caloric and fluid requirement
Safe and sufficient infant feeding is a human right. Delivering safe and sufficient calories and fluid to an infant is perhaps the single most important determinant of that infant’s future health and brain development. The aggressive promotion of exclusive breastfeeding over ensuring every baby is sufficiently fed has caused maternal and newborn suffering, newborn hospitalizations and a still unmeasured epidemic of developmental disabilities among infants who experience breastfeeding complications. We call on Baby-Friendly USA, the Academy of Breastfeeding Medicine and the WHO/UNICEF to honestly inform mothers regarding the lack of evidence that supports the exclusive breastfeeding BFHI metric, the risks of injury to the brain and vital organs from insufficient feeding of infants and the role of supplementation to prevent serious and irreversible harm to newborns.

There are many ways you can support the mission of the Fed is Best Foundation. Please consider contributing in the following ways:
- Join the Fed is Best Volunteer group to help us reach Obstetric Health Providers to advocate for counseling of new mothers on the importance of safe infant feeding.
- Make a donation to the Fed is Best Foundation. We are using funds from donations to cover the cost of our website, our social media ads, our printing and mailing costs to reach health providers and hospitals. We do not accept donations from breast- or formula-feeding companies and 100% of your donations go toward these operational costs. All the work of the Foundation is achieved via the pro bono and volunteer work of its supporters.
- Share the stories and the message of the Fed is Best Foundation through word-of-mouth, by posting on your social media page and by sending our resources to expectant moms that you know. Share the Fed is Best campaign letter with everyone you know.
- Write a letter to your health providers and hospitals about the Fed is Best Foundation. Write them about feeding complications your child may have experienced.
- Print out our letter to obstetric providers and mail them to your local obstetricians, midwives, family practitioners who provide obstetric care and hospitals.
- Write your local elected officials about what is happening to newborn babies in hospitals and ask for the legal protection of newborn babies from underfeeding and of mother’s rights to honest informed consent on the risks of insufficient feeding of breastfed babies.
- Send us your stories. Share with us your successes, your struggles and everything in between. Every story saves another child from experiencing the same and teaches another mom how to safely feed her baby. Every voice contributes to change.
- Send us messages of support. We work every single day to make infant feeding safe and supportive of every mother and child. Your messages of support keep us all going.
- Shop and Fed is Best Foundation will earn cash back! We hope to develop our online safe infant feeding classes with these funds.
- If you need support, we have a private support group – Join
We believe all babies deserve to be protected from hunger and thirst every single day of their life and we believe that education on Safe Infant Feeding should be free. If you would like to make a donation to support the Fed is Best Foundation’s mission to teach every parent Safe Infant Feeding, please consider making a one-time or recurring donation to our organization.

7 thoughts on “WHO 2017 Revised Guidelines Provide No Evidence to Justify Exclusive Breastfeeding Rule While Evidence Supports Supplemented Breastfeeding”