Step 7 of the Baby-Friendly Hospital Initiative (BFHI) policy requires parents to room in with their baby 24 hours a day immediately after delivery.
Mothers are commonly sleep-deprived and profoundly exhausted after labor and delivery, some laboring for > 24 hours, some recovering from major surgery. They are required to nurse and care for a newborn almost immediately after delivery with few exceptions. Maternal exhaustion has lead to tragic and preventable accidental newborn falls from bed and suffocation from falling asleep while breastfeeding in bed. These accidents have resulted in brain injury, severe disability, and rare deaths in previously healthy infants. The elimination of newborn nurseries by hospitals has increased as a result of the Baby-Friendly policy. These tragic events received the attention of pediatricians and the Neonatology Section of the American Academy of Pediatrics who has published their concerns in the medical journals of JAMA and JAMA Pediatrics and Pediatrics.
In this recent article that was published in pediatrics, In-hospital Neonatal Falls: An Unintended Consequence of Efforts to Improve Breastfeeding, falls that occur when caregivers fall asleep is a consistent theme in the reported series. In a review of patient safety data over a 9-year period, Wallace reported that 150 of 272 neonatal falls occurred after a caregiver fell asleep while holding the newborn.7 Several smaller series report that 36% to 66% of in-hospital neonatal falls involved caregivers falling asleep.1,3,4,12 Not surprisingly, these falls transpired most commonly during the night or early morning hours. Similar to our series, Galuska13 described 5 cases at a single center in which all neonates fell from their mothers’ arms in the early morning hours, continuing to implicate fatigue as a factor.
Nicole Writes:
I delivered my baby shortly after midnight via emergency c-section at 36+4 weeks. I was doing lots of skin-to-skin contact and breastfeeding with assistance, but his blood sugar was low, and formula milk was needed to stabilize his blood sugar. It felt like we had to force him to drink it and that concerned me.
Thankfully, my mom was staying with me to care for me and my baby on the first day. I was medicated with narcotics every few hours for pain from my surgery and I developed body shaking and my skin was itching constantly. My mom had to leave for a bit, so I was alone; but my mom told the nurses, so they knew I was alone caring for my baby in this condition.
I hadn’t slept in 36 hours or eaten in 24 hours, and I was profoundly exhausted, emotional, and in pain and was expected to care for my baby anyway.
I hadn’t seen a nurse in a while, so I called my mom to see when she would be back, and she said it would be an hour. I woke up to my mom shaking me and two nurses hovering over my baby. I dropped him from my bed. I was so sleep-deprived and very sedated from being medicated that I didn’t even hear him screaming. According to my mom, I was completely unresponsive. The nurses took my baby to the NICU to check him out, and I couldn’t even react; I didn’t know how to. I just kept going over everything in my mind.
What if I killed my baby? What if I hurt him? What if he has a brain injury? Do I even deserve to have this baby? What if he gets taken away? He literally fell a few feet from my arms to the ground. A tiny, not even 24-hour-old preemie.
Why are new mothers expected to take care of their babies when they are recovering from major surgery? Why isn’t there a nursery to take your baby to when you need one, for safety? Why hadn’t the nurses checked on me? I hadn’t seen them in at least 1 hour before I fell asleep. Why didn’t they check on us when he was screaming bloody murder? The nurse’s station was right outside my room and my mom heard him all the way down the hall. Why was I given a dangerous amount of Percocet and expected to take care of myself and my baby? I WAS ANGRY!

Because I was medicated and profoundly exhausted and alone with my baby, he fell out of my hospital bed easily.
In this recent article that was published in pediatrics, In-hospital Neonatal Falls:An Unintended Consequence of Efforts to Improve Breastfeeding, falls that occur when caregivers fall asleep is a consistent theme in reported series. In a review of patient safety data over a 9-year period, Wallace reported that 150 of 272 neonatal falls occurred after a caregiver fell asleep while holding the newborn.7 Several smaller series report that 36% to 66% of in-hospital neonatal falls involved caregivers falling asleep.1,3,4,12 Not surprisingly, these falls transpired most commonly during night or early morning hours. Similar to our series, Galuska13 described 5 cases at a single center in which all neonates fell from their mothers’ arms in the early morning hours, continuing to implicate fatigue as a factor.
What is more ludicrous is that the 24-hour rooming-in policy has been shown to have no effect on increasing sustained breastfeeding after discharge. The 2017 WHO revised breastfeeding guidelines reviewed all the data regarding this policy and showed no effect of 24-hour rooming-in on breastfeeding rates at 3-4 months. Despite the negative short-term effects of this policy on parental sleep and rare serious effects on the infant in the form of falls and sudden unexpected postnatal collapse (SUPC), neither the WHO nor Baby-Friendly USA has changed this recommendation. In fact, health professionals are scripted to try to discourage parents from sending their infants to the nursery if they express the need for sleep, which ultimately puts infants at risk by perpetuating the unsafe condition of being cared for by an impaired parent.
Nicole continues:
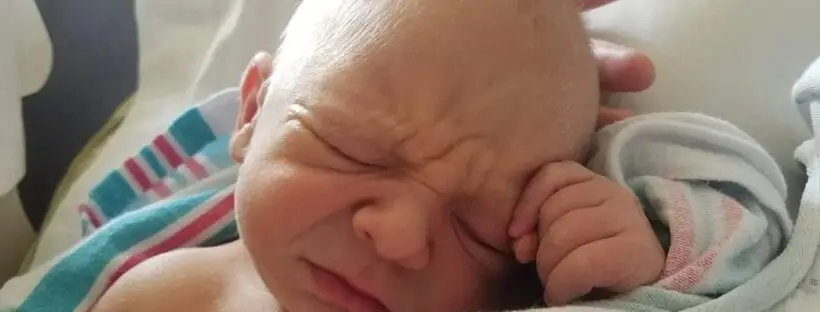
I don’t know how he wasn’t severely hurt, but I was beyond thankful. Minus being slightly hypothermic, his exam was normal. Despite being high risk, 4 weeks early, having low blood sugar, and being dropped, we avoided a NICU stay. I had a super easy recovery at home, having a little trouble gaining weight, we are both doing wonderfully. He is growing, meeting or exceeding all of the milestones, and I couldn’t be more in love with him.
More information and stories about newborn falls:
Breastfeeding Improvement Initiatives May Increase Risk of Newborn Falls
“Is Baby-Friendly Baby Safe?,” Fetus & Newborn Conference 2018
My Baby Was Put in a Dangerous Situation By Rooming-In with an Exhausted Mom
Neonatal Nurse Practitioner Speaks Out About The Dangerous Practices Of The BFHI
U.S. Study Shows Baby-Friendly Hospital Initiative Does Not Work
Nurses Are Speaking Out About The Dangers Of The Baby-Friendly Health Initiative
Nurses Quit Because Of Horrific Experiences Working In Baby-Friendly Hospitals
NICU Nurse Discloses Newborn Admission Rates From Breastfeeding Complications in BFHI Unit
Pediatrician and Other Physician Views on the Baby-Friendly Hospital Initiative

One thought on “I Dropped My Baby in a Baby-Friendly Hospital While I Was Alone Recovering from a Cesarean Section”