by Jillian Johnson with commentary from Dr. Christie del Castillo-Hegyi
Landon would be five today if he were still alive. It’s a very hard birthday–five. It’s a milestone birthday. Most kiddos would be starting kindergarten at this age. But not my little guy. I wanted to share for a long time about what happened to Landon, but I always feared what others would say and how I’d be judged. But I want people to know how much deeper the pain gets.
I share his story in hopes that no other family ever experiences the loss that we have.
Jarrod and I wanted what was best for Landon, as every parent does for their child. We took all of the classes. Bought and read all of the books. We were ready! Or so we thought….every class and book was geared toward breastfeeding and how it’s so important if you want a healthy child. Landon was born in a “Baby-Friendly” hospital. (What this means is everything is geared toward breastfeeding. Unless you’d had a breast augmentation or cancer or some serious medical reason as to why you couldn’t breastfeed, your baby would not be given formula unless the pediatrician wrote a prescription.)

Sleeping comfortably a few hours after birth
Landon was born full-term weighing 3360 g or 7 lbs. 7 oz, born by urgent cesarean due to fetal intolerance to labor after the water had broken. [Previous publication of this blog said he had an emergency c-section. He was delivered by low transverse incision over 12-14 minutes, which is considered an urgent, not a STAT section.] Apgars were 8 and 9 and he was stabilized. He was transferred 2.5 hours later to the Mother-Baby Unit and returned to his mother. He exclusively breastfed with excellent latch for 15 – 40 minutes every 1-2 hours.

Landon, is 12 hours old.
Landon was on my breast —ALL OF THE TIME. The lactation consultants would come in and see that “he had a great latch and was doing fine,” but there was one who mentioned Imay have a problem producing milk. The reason she gave was that I was diagnosed with PCOS (polycystic ovarian syndrome), and it was just harder for women with hormone imbalances to produce milk. She recommended some herbs to take when I got out of the hospital.
While in the hospital, his mother’s risk factors for failed and delayed lactogenesis II (copious milk production) were identified by the IBCLC-lactation consultant. They were borderline diabetes, PCOS, issues with infertility, small, widely spaced breasts with minimal growth during pregnancy, being a first-time mom, and emergency c-section. Despite that, she was encouraged to exclusively breastfeed. She was closely monitored by a nurse, lactation consultant, and physician support. Her baby’s latch was rated as excellent.
By the first 24 hours, he had nursed a total of 9.3 hours, had zero wet diapers and four dirty diapers. By 27 hours, he had lost 4.76%. His nursing sessions became longer and longer until he was on the breast continuously by the second day of life. On the second day, he produced 3 wet diapers and 6 dirty diapers and nursed for almost 14 hours total. By53 hours of life, he had lost 9.72%.
At this time, the scientific literature on wet and dirty diaper production has shown that the number of diapers produced have no correlation with adequacy of milk intake in the first 4 days of life. The only study on diaper counts has shown that even newborns who lose excessive weight can produce up to 6 wet and dirty diapers a day. In addition, at this time, the Baby-Friendly Hospital Initiative has produced no data on the safety of newborn fasting and weight loss caused by exclusive colostrum feeding and what degree of weight loss protects a child from brain-threatening complications like hyperbilirubinemia, hypernatremic dehydration, and hypoglycemia. So far, the scientific literature shows that babies who lose greater than 7% of their birth weight are at the highest risk of developing excessive jaundice and hypernatremia to levels that can cause long-term developmental disability. It has also been found that 10% of healthy, term, exclusively breastfed babies undergoing the Baby-Friendly protocol experience hypoglycemia to levels that are associated with 50% declines in the ability to pass the literacy and math proficiency test at 10 years of age, even if aggressively corrected.
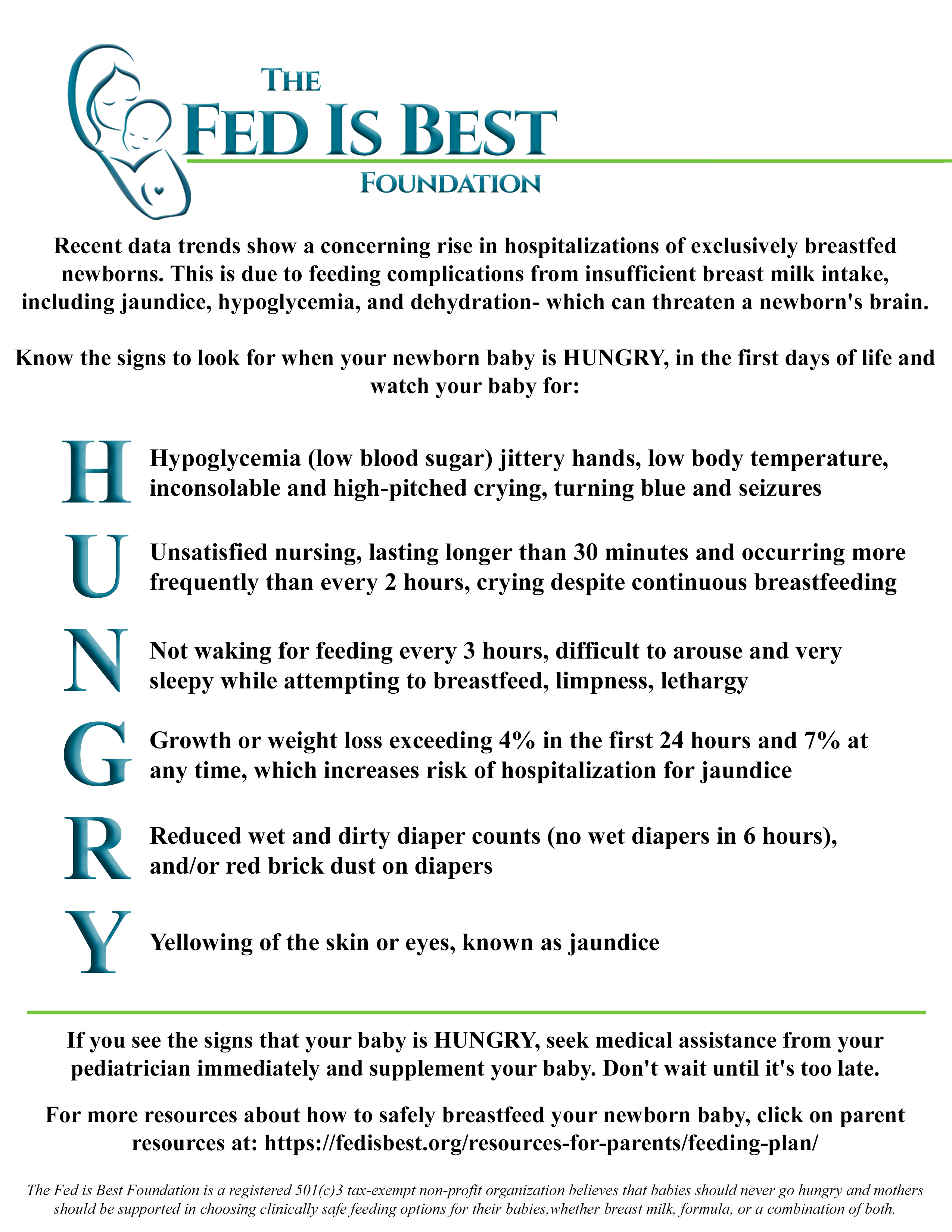
Constant, unsatisfied nursing and inconsolable crying are two of the signs of newborn starvation that lead to brain-threatening complications. If a child is receiving a fraction of their caloric requirement through early exclusive breastfeeding, they can experience severe hunger and thirst, which is why they will cry inconsolably and breastfeed continuously when it is the only source of calories and fluid they are offered. If a mother’s colostrum does not meet the child’s caloric requirement, they will breastfeed for hours a day in an attempt to relieve their hunger. A child who is “cluster-feeding” may actually burn more calories breastfeeding than they receive in return, which can result in fasting conditions and accelerated weight loss. The constant nursing and crying often found in newborns by the second day of life have been called“The Second Night Syndrome” in the breastfeeding industry. This is also whenmothers receive the most pressure to avoid supplementation in order to increase rates of exclusive breastfeeding at discharge. Babies who reach critically low levels of reserve fuel and fluids before their mother’s milk comes in can be found lethargic with compromised vital signs after hours of constant nursing and fussing, at which time they are often diagnosed with hypoglycemia, excessive weight loss, and/or hyperbilirubinemia, all markers of starvation.
Did you know that newborns aren’t supposed to cry all of the time? They’re supposed to eat and sleep and dirty their diapers. I had no idea he was inconsolable because he was literally starving. And when a baby is only on the breast, how do we gauge how much they’re actually getting out? Sure, there should be wet and soiled diapers and weight checks, right? And where is the limit as to weight loss and a minimum for the diapers changed?

Being discharged with visible weight loss.
Landon was discharged at 64 hours (2.5 days) of life having lost 9.7% of his birth weight continuously and exclusively breastfeeding with a mother whose milk had not come in. These are routine and unremarkable findings in newborn babies discharged home to exclusively breastfeed. At this time, there are no studies using standardized developmental testing or serum markers of starvation that show that allowing babies to lose up to 10% of their birth weight protects them from brain- and life-threatening complications, despite wide-spread perception that it is normal for exclusively breastfed babies to lose. Therefore, Landon’s mother was given no instruction to supplement. He was discharged with next-day follow-up.
So we took him home….not knowing that after less than 12 hours home with us, he would have gone into cardiac arrest caused by dehydration from unintended starvation because I was the mother who had no colostrum for my baby. The best advice I was given by one of his NICU doctors while he was on life support is that the breast is best, but follow with the bottle if they are still hungry.
This way you know your baby has eaten enough….if only I could go back in time.
Landon continued to breastfeed at home continuously and was found unresponsive, pulseless, and blue after eventually falling asleep from cluster feeding. His parents called 911. Per EMS, he was asystolic (no heart rate), and he received CPR en route to the local ER. By the time they arrived at the ER, he was found to have pulseless electrical activity (heart rate with no blood pressure). There, he was intubated and received several rounds of epinephrine. He was hypothermic with a temperature of 93.1 F. After 30 minutes of CPR, no cardiac activity was found on ultrasound. With parental consent, CPR was stopped, and he was left on the ventilator while continuing to receive IV saline. Twenty minutes later, with IV fluids, he regained his pulse. He was transferred to a Level III NICU to get the head cooling protocol for babies that experience a brain injury. He was diagnosed with hypernatremic dehydration and cardiac arrest from hypovolemic shock.

Landon is in the NICU on full life support.
I still have many, many days of guilt and questions – what if I had just given him a bottle? And anger because how would I have known? I trusted my healthcare professionals to protect my baby from harm. I remember when Stella, my daughter was born, and she was always quiet. I kept asking the nurses what was wrong with her. They said nothing. She’s doing what she’s supposed to. Sleeping and eating. And it was then that I realized that it wasn’t normal for a newborn to cry as much as Landon did. He was just crying out from his hunger. But I didn’t know. I should’ve known. I still struggle daily, feeling as though I failed him.
Landon received a brain MRI in the hospital which confirmed brain injury consistent with hypoxic-ischemic encephalopathy or brain injury from oxygen deprivation due to low blood pressure from dehydration and cardiac arrest. He was diagnosed with diffuse seizure activity on EEG, the consequence of severe, wide-spread brain injury. Given his poor prognosis, he was taken off life support 15 days later. The autopsy report deemed the causes of death were hypernatremic dehydration followed by cardiac arrest causing hypoxic-ischemic encephalopathy (diffuse brain injury).

Jill held Landon as he took his last breaths.
That little boy gave me ten of the most incredible life-changing months. I’ve been humbled. Challenged. My relationships have fallen apart. Some have come back together. I’ve learned forgiveness. And the true meaning of “life is short.” I love hard – to a fault. But I couldn’t live with myself knowing his death was in vain. I’ve learned so many lessons. I’ve learned the true meaning of compassion and unconditional love.
— Jillian Johnson
To Learn More About Ensuring SAfe and ADequate Feeding While Breastfeeding Your Newborn
Order the Fed Is Best book at all major retailers or by clicking on the button below. With it comes the Fed Is Best Book Resource Page, a free online guide to safe and adequate breastfeeding.
The Fed is Best Foundation is dedicated to the prevention of newborn and infant starvation from insufficient exclusive breastfeeding. We do so by studying breastfeeding stories sent by mothers and the scientific literature on breastfeeding complications that lead to infant brain injury and death. Since the beginning of our campaign almost two years ago, we have received tens of thousands of newborn and infant starvation stories leading to the complications of hyperbilirubinemia, dehydration, hypernatremia, hypoglycemia, and failure to thrive. These complications occur because the current breastfeeding guidelines have not been studied for safety and operate with little awareness of the caloric and fluid requirements of newborns nor the amount transferred to babies until complications have already occurred. “Just one bottle” can save a child from these tragedies as it is often a mother’s first clue that a child is, in fact, starving from exclusive breastfeeding.
If your baby is experiencing distress and signs and symptoms of starvation, we encourage you to advocate for your child. We encourage mothers to notify hospital administrators if they are pressured to avoid supplementation to alleviate their child’s hunger. You have the right to feed your child, and your child has the right to be fed. No one but your baby knows how close they are to empty. The only way they can communicate distress is by crying. Listen to your baby and listen to your instincts.
Our message is simple. Feed your baby. Feed them as much as they need to stay safe and satisfied.
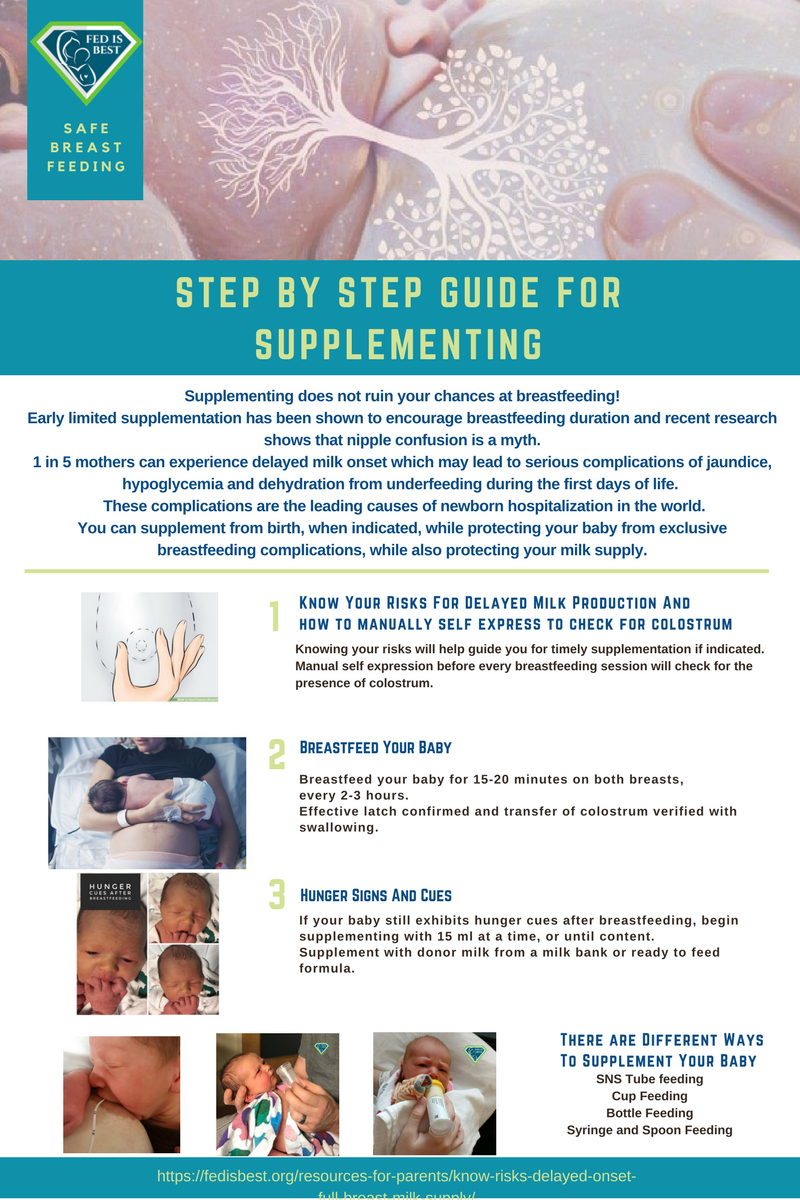
How to supplement your baby until your milk comes in:
How To Prepare For Supplementing When Breastfeeding Your Baby In The Hospital
Jillian Johnson: My Message To Parents During World Breastfeeding Week-Just One Bottle
https://fedisbest.org/2022/01/nigerian-mother-speaks-out-about-her-babys-death-after-being-told-to-keep-exclusively-breastfeeding-what-she-wants-human-rights-organizations-to-know/
My Baby Suffered And Almost Died–Why Are The Risks Of Exclusive Breastfeeding Not Taught To Mothers?
Just One Bottle Would Have Prevented My Baby’s Permanent Brain Damage from Hypoglycemia
Feeding Your Baby—When Supplementing Saves Breastfeeding and Saves Lives
U.S. Study Shows Baby-Friendly Hospital Initiative Does Not Work
NICU Nurse Discloses Newborn Admission Rates From Breastfeeding Complications in BFHI Unit
Nurses Are Speaking Out About The Dangers Of The Baby-Friendly Health Initiative
https://fedisbest.org/2018/11/neonatal-nurse-practitioner-speaks-out-about-the-dangerous-and-deadly-practices-of-the-bfhi/
Hospital Drops Baby Friendly Program After Doctors Baby Was Harmed
Letter to Doctors and Parents About the Dangers of Insufficient Exclusive Breastfeeding
Two Physicians Describe How Their Baby-Friendly Hospital Put Their Newborn in Danger
I Supplemented My Baby Until My Milk Came In And We Are Still Breastfeeding At 3 Months
Fed is Best Statement to the USDA Regarding the Harms of the Baby-Friendly Hospital Initiative
Nurses Quit Because Of Horrific Experiences Working In Baby-Friendly Hospitals
Nurses Are Speaking Out About The Dangers Of The Baby-Friendly Health Initiative
“Is Baby-Friendly Safe?”: BFHI Safety Issues Discussed at National Neonatology Conference
CONTACT US/VOLUNTEER
THANK YOU FOR YOUR INTEREST IN THE FED IS BEST FOUNDATION!
Our mission statement is:
The Fed Is Best Foundation works to identify critical gaps in the current breastfeeding protocols, guidelines, and education programs and provides families and health professionals with the most up-to-date scientific research, education, and resources to practice safe infant feeding, with breast milk, formula or a combination of both.
Above all, we strive to eliminate infant feeding shaming and eliminate preventable hospitalizations for insufficient feeding complications while prioritizing perinatal mental health.
HOW YOU CAN SUPPORT FED IS BEST
There are many ways you can support the mission of the Fed is Best Foundation. Please consider contributing in the following ways:
- Join us in any of the Fed is Best volunteer and advocacy, groups. Clickhereto join our health care professionals group. We have: FIBF Advocacy Group, Research Group, Volunteer Group, Editing Group, Social Media Group, Legal Group, Marketing Group, Perinatal Mental Health Advocacy Group, Private Infant Feeding Support Group, Global Advocacy Group, and Fundraising Group. Please send an email to Jody@fedisbest.org if you are interested in joining any of our volunteer groups.
- If you need infant feeding support, we have a private support group–Join us here.
- If you or your baby were harmed from complications of insufficient breastfeeding please send a message tocontact@fedisbest.org
- Make adonationto the Fed is Best Foundation. We are using funds from donations to cover the cost of our website, our social media ads, our printing and mailing costs to reach health providers and hospitals. We do not accept donations from breast- or formula-feeding companies and 100% of your donations go toward these operational costs. All the work of the Foundation is achieved via the pro bono and volunteer work of its supporters.
- Sign our petition!Help us reach our policymakers,and drive change at a global level. Help us stand up for the lives of millions of infants who deserve a fighting chance. Sign theFed is Best Petition at Change.orgtoday, and share it with others.
- Share the stories and the message of theFed is Best Foundationthrough word-of-mouth, by posting on your social media page and by sending our FREE infant feeding educationalresourcesto expectant moms that you know. Share theFed is Best campaign letterwith everyone you know.
- Write a letter to your health providers and hospitals about the Fed is Best Foundation.Write to them about feeding complicationsyour child may have experienced.
- Print out ourletter to obstetric providersand mail them to your local obstetricians, midwives, family practitioners who provide obstetric care and hospitals.
- Write your local elected officialsabout what is happening to newborn babies in hospitals and ask for the legal protection of newborn babies from underfeeding and of mother’s rights to honest informed consent on the risks of insufficient feeding of breastfed babies.
- Send us your stories.Share with us your successes, your struggles and everything in between. Every story saves another child from experiencing the same and teaches another mom how to safely feed her baby. Every voice contributes to change.
- Send us messages of support.We work every single day to make infant feeding safe and supportive ofeverymother and child. Your messages of support keep us all going.
- Shop atAmazon Smileand Amazon donates to Fed Is Best Foundation.
Or simply send us a message to find out how you can help make a difference with new ideas!
For any urgent messages or questions about infant feeding, please do not leave a message on this page as it will not get to us immediately. Instead, please email christie@fedisbest.org.
Thank you and we look forward to hearing from you!

Parents tell us they were not taught how to supplement their babies safely, if necessary to prevent exclusive breastfeeding complications.
For more information on how to protect your baby from feeding complications due to early exclusive breastfeeding, please read and download the Fed is Best Feeding Plan, a way to communicate your feeding choices to your health care providers.
In addition, please read and download the Fed is Best Weighing Protocol to prevent newborn dehydration and failure to thrive.
Lastly, for more detailed information, please watch our educational videos onPreventing Feeding Complications.
Our full list of parent resources can be found on our Resource Page.
If you wish to help parents learn how to protect their newborns from accidental starvation, please share this story and sign our petition to demand that the CDC, the AAP, the U.S. Surgeon General and the WHO/UNICEF Baby-Friendly Hospital Initiative warn parents about the dangers of newborn and infant starvation from insufficient exclusive breastfeeding. Go to https://fedisbest.org/sign-our-petition/.
Please consider making a donation to the Fed is Best Foundation to support its mission of providing safe infant feeding education and support and raise awareness on the harms of insufficient infant feeding.
We believe all babies deserve to be protected from hunger and thirst every single day of their life and we believe that education on Safe Infant Feeding should be free. If you would like to make a donation to support the Fed is Best Foundation’s mission to teach every parent Safe Infant Feeding, please consider making a one-time or recurring donation to our organization.
Donate to Fed is BestThank you so much from the Founders of the Fed is Best Foundation!




I am so sorry for your loss. I cried so hard reading this because I almost had the same thing happen to me. After coming home from the hospital with my daughter Madison, my first child, she was the same way. Always crying and constantly on my breast. My fiance saw how much of a toll it took on her and I (me because I hadn’t slept since she was born). He went out and got formula because I told him there is no way she should be constantly on me, I felt something was wrong. After giving her a bottle she slept for almost 4 hours and I finally got sleep after being awake almost 3 days. I didn’t go back to breastfeeding after that. It was apparent my daughter was starving. I wanted to do the natural thing and breastfeed but I wasn’t producing. Being a first time mom, I’m relieved to see I wasn’t the only one that’s had that problem. Again, I’m so sorry for your loss and I will pray for your family!
Thank you for sharing your story! I’m so sorry for your loss. I am a nurse, although this area is not my area of practice. When I had my son, after an emergency c-section, I felt very unsupported. Of course I wanted to breastfeed but I felt as though he was not getting enough milk because he was always crying. When I expressed my concerns, I didn’t get much response from the nurses, until one angel showed me SNS feeding, which allowed my to have my son at the breast but receive formula via a tube attached to my breast. In the end, breastfeeding didn’t work out for us. I carried a lot of guilt with me when I decided to stop. Now, my son is six, he’s healthy and active. Breastfeeding or formula feeding seems such a little decision in the big picture these days. I wish there was more support to allow mom to make decisions to breastfeed or formula feed. Obviously, the majority of mom’s aren’t going to intentionally do anything that isn’t in their child’s best interest.
Please share this with the La Leche League,
I had a family member go through this same thing. The discharge pediatrician for my nephew just blew off her concerns that he was not eating well. They went home and the issues continues. I called the La Leche League on the second day he was home to ask for advice and they said just to keep it up and he that it would be OK. The next day he was admitted to the hospital for dehydration. He recovered but it was very worrying that my cousin was dismissed by so many when she knew he was not getting enough to eat. No one mentioned supplemental feedings or the hospitals donated milk supply. I am glad in the end that he was OK but this shows that it could have turned out so much worse. Thank you for sharing you story with the world.
Your story breaks my heart. I’ve literally been bursting into tears for days just thinking about it, about how preventable it was, but how easily it could happen with poor advice and lack of appropriate monitoring by healthcare staff. I have also caught myself saying prayers to your sweet little Landon up in heaven (if you believe in it) and reassuring him that you loved him with all your heart and that you only did what you believed was best for him, although of course he already knows that. Although part of me wishes that I had never read your story (it’s just so sad!), I am so glad that you are starting to heal and that you are now able to share it. Sharing this knowledge is important to help prevent other parents and babies from suffering the same fate.
I am incredibly fortunate that our local hospital encourages breastfeeding while also monitoring for signs of hydration and suggesting formula top-ups if thought necessary. I also had formula on my baby essentials list (following Lucie’s List!) just in case for some reason I was unable to feed him or felt that I needed to top him up as the advice I was given was the last thing you want is a hungry baby with no way to feed them. I am so lucky that I received that advice, even if I never actually needed to use it (although my son did feed for 10 hours out of 24 for the first two or three months of life, he always gained weight and, while a slow eater, was fortunately getting enough). The small tub of formula is still unopened in the cupboard, still in date and ready for baby number two, and thanks to you and the good advice I received previously, I will not be afraid to use it, if needed. A small tub of formula should really be on everyone’s baby essentials list, even if they plan to exclusively breastfeed.
You didn’t fail your son, you did the very best that you knew how at the time. My son actually ended up back in hospital with an awful bladder infection that had spread to his blood at 21 days old and I still feel guilty about that and think about ways I maybe could have prevented it. (We were using cloth wipes and I didn’t know they needed to be boiled/sterilized and was just washing them on cold; maybe I didn’t change his diaper enough; the weather was really hot which promotes bacteria growth – maybe I should have used the air conditioner more…). His pediatrician said that type of infection could take a life that young in just 24 hours.
That experience certainly humbled me and I now have such a huge appreciation for just how fragile and vulnerable newborns are, but also how vulnerable and helpless we are as (particularly first time) mothers. I am happy to hear that you now have a healthy little girl and happy that this website and initiative exists. I wish you all the luck in the world getting the message out to healthcare staff and future moms. No one should ever be made to feel guilty for (let alone prevent from!) feeding their baby formula whether out of caution, necessity, or just to maintain sanity. RIP sweet little Landon.
Your post hit so close to home. When my son was born, I was also very militant about breastfeeding him. I thought he was nursing successfully, but he wasn’t. His latch on wasn’t good enough. The morning after we brought him home, my husband looked at our son and said “he looks like a pretzel. I think he’s dehydrated and needs some formula.” I was horrified, offended and defiant. I absolutely refused to give him formula. In my mind at the time it seemed like a poison to me (ludicrous, I know!). Fortunately my husband remained very calm and diplomatic. He offered a compromise -we’d bring him in for a check-up, and if the pediatrician said he was okay, then all was good. I agreed. When the pediatrician walked into the exam room, she took one look at my son from afar and ran out of the room, returning moments later with formula, saying “You have to fed him this NOW!” What a wake-up call. Thank goodness my husband could see what I could not at the time. After reading your story, I realize now how dire my son’s situation was, and how close he could have been to death. I’m so sorry for the loss of your son.
Bless you. I can only imagine how difficult it was for you to share this story with the world along with pictures of your sweet boy. Happy birthday, Buddy!
To the mother of this beautiful little boy: you did your best. The hospital never should have released – they saw the signs and should have known your body wasn’t producing the milk Landon needed. You did everything right. there was no way you could have known that Landon was starving except that your motherly instincts knew something was wrong. You had no way of actually knowing what because the doctors and nurses kept insisting every thing was fine. Landon will be in your heart forever more and he lives through you. Thank you for sch a heart breaking yet touching story. Let yourself heal – that’s what Landon wants for you.
I am so sorry to read this. I feel that this could so easily have happened to me too, had it not been for the fact that the community midwife had my daughter admitted to the Children’s Ward due to weight loss on Day 3. I had previously breast fed my son without any difficulties and still don’t really understand what the problem was with breastfeeding my daughter. I find it hard to look at photos of her in the first couple of days because she looks dehydrated and I remember her crying all the time because I now realise she was hungry. Once I realised what was going on, I switched to bottle feeding and we never looked back. I guess every baby and time is different. You are absolutely doing the right thing to raise awareness of this issue.
My first born son ended up in hospital for a week when he was 10 weeks old. He was literally starving. I had read so much literature on Breast is Best.
I am so sorry for your loss.
God Bless you Jill and your family. You’ve been through so much, I am praying for you. May your little Angel Landon always be looking over you. I hope in time your pain will ease knowing you did nothing wrong, trusted those who were professionals and they failed you and your beautiful boy. I admire your courage, thinking of others. Your story will now help so many, your little Landon will now save other babies whose mother’s are in the same situation. He is a hero in his own right. God Bless xox
As a a first time mother to be this story is needed. Thank you for sharing it and much love to you and your loss. I am constantly worried will my baby get enough milk, and just want to be as informed as possible, I have had a few friends go home form hospital in my opinion to early only to return as the baby isn’t receiving enough/or none at all of breast milk. I will be making sure I am not belittled or harassed if about what is best for my baby.
Oh Jillian!
Thankyou for sharing Landon’s story. I can only imagine how hard it must have been to do that. You have so much courage!
I am a mother of three in Australia.
My son Liam is now 20, but I came so very close to having the same story to tell as you have shared.
Liam was born 10 days post-dates by vaginal birth in the USA. He was a healthy 3.8 kgs and well at birth. He breastfed soon after birth and continued to feed well and frequently. Excellent latch, good long feeds. We were discharged within 24 hours. He was my second baby and my first had breastfed for 2 years, so I wasn’t expecting any issues.
Liam fed frequently and when he wasn’t feeding he was crying. My eldest was 5 and I couldn’t recall her crying so much, but put it down to Liam just being a fractious baby. I had him on the breast all. the. time! My parents were visiting and they both remarked on his crying, but I felt he was latching well, so assumed he had some pain and fed him some more. He didn’t have many wet nappies, but was passing meconium regularly. I was a midwife and committed to exclusively breastfeeding. I really didn’t think there was a problem. I was sleep-deprived and just couldn’t see what was happening.
The hospital where Liam was born had just introduced a follow-up well baby check on day 5, so I duly went along to see the paediatrician with my baby. Thank God I did! Liam had lost 20% of his birth weight and just lay there on the examining bed, not crying now, just laying listlessly. It wasn’t until I saw him lying there that I realised how sick he was. It was like I had not been able to see the big picture before this moment.
Liam was immediately admitted to NICU and commenced on IV fluids. He was severely hypernatraemic and it took 4 days for his blood levels to return to normal. My poor little guy was dying of starvation and dehydration! And I had no idea.
I thank God every day that my hospital had initiated the 5 day checkup because if I had not taken Liam to the Dr that day I dread to imagine what story I would be telling today. I am still wracked with guilt that I, a midwife and a mother, could not see what was happening to my baby boy. At every stage in Liam’s development I have been overcome with shame and guilt if there was any hiccup in him meeting his milestones. Fortunately my beautiful baby boy has grown into an intelligent, caring young man, but I still feel very responsible for all he went through in his first days.
I was encouraged to continue breastfeeding Liam once he was discharged from the hospital, but I had no confidence in my ability and he thrived on formula.
I am still an advocate for breastfeeding. I breastfed my third child exclusively for 6 months and continued to feed her for 2 years. But I was vigilant in observing her behaviour and weight gain and output. I continue to work as a midwife and encourage and support women to breastfeed if that is what they wish to do. Breast is best, yes, but only if that is what is working for both Mum and baby. The most important thing, as this article states, is that FED is best and we need to ensure that babies are being nourished, not just breastfed.
Thankyou again for sharing your story. This is the first time I have been able to put into words the feelings I have had for the past 20 years. The guilt will always be there, but I have come to be a little more forgiving to myself.
Dear Jill, my heart goes out to you! I read your story a few days ago and cannot stop thinking about you and little Landon. I can’t imagine the pain you endured five years ago and the pain you have endured since then. I’m so sorry this happened to you! I know the pressure society puts on us, and we put on ourselves, to exclusively breastfeed. My daughter lost 11% of her bodyweight during her first few days of life because my milk had not come in. I too thought it was normal (although I was really freaking out inside). Luckily and thankfully for me, my husband, and my daughter, she is OK. I am now pregnant with our second child – a little boy – and I am so glad you posted this before I had him so that I can be more vigilant and careful with him. Thank you.
I am so sorry for your terrible loss. My heart broke for you as I read these words and I realised how easily this could have been my story. We thought we had a baby who was just a good sleeper (about 7 hours at a time) but he would scream every time I tried to feed him. This went on for about a month, under the supervision of a clinic sister, until a family member (also a paediatric nurse) was in tears as she watch me trying to feed my baby. After 4 weeks She rang one of the heads of department at the Children’s Hospital and after asking about 5 simple questions – he said “that kid is starving. Go and buy bottles and formula IMMEDIATELY”. That gave me the confidence to push back when my clinic nurse continued to advise me to breastfeed, almost to the point of telling me I was being negligent. No other time in my life have I felt so inadequate and bullied by other women as I did when I brought my first child into the world. My story has a very happy ending but it really distressed me reading your story as it highlighted just how close I came to a much different outcome. Again, I am so sorry for the loss of your gorgeous Landen but I thank you for sharing your story to help others find their voice when faced with the same advice.
So sad, losing a infant is so so sad. I’m sorry and know losing a child is painful having to think about could’ve would’ve shoulda for the rest of your life Is well you know I pray for you and anyone who has lost a child thanks for sharing
A note to Jillian (the mom)– It is hard to know what to say to you. I am sorry for your loss of your beautiful baby, over four years ago. I did not lose my baby, but I had trouble with feeding my first baby. When I was pregnant I did a lot of reading and studying so that I would know how to take care of a (my) baby, especially in the first days, weeks and months. I tried breastfeeding while in the hospital. I had a cesarean section to have my baby, so I did not feel good the first night. Early in the morning the nurse would check on me and tell me it’s time to feed my baby. For some reason I did not do it right away. I ended up asking them for a bottle of formula. They seemed to wonder why I did not ask for it sooner. But this was my first baby and I wondered why they were talking in a rude, or seemingly rude, tone of voice. After three days I took my baby home. I only breastfed my baby over the following weekend because I was believing that I should follow the doctors stern suggestion. I thought of calling the pediatrician but I didn’t because it was the weekend. My baby cried a lot when I tried to feed her. I thought that maybe she wasn’t latching on very well. I was frustrated and my baby was frustrated. I think it was after the weekend on Monday that I called the pediatrician. He told me to bring my baby in to see him. He told me to feed my baby with formula. But it did not work very well. So, some days later, when my baby was 13 or 14 days old, the doctor told me to take my baby to the Children’s Hospital. My daughter was in the hospital for four days. They gave her IV liquids and bottle fed her. She finally improved just enough to go home. It still took at least two weeks before she improved some more. And then, in a few weeks after that she was starting to drink too much. Or it seemed like it after what we had been through. I thought that she had gained a little too much weight at that point. While my daughter was in the hospital they were saying that her jaw was week. When I bottle-fed her they showed me how to support her lower jaw. That was the main problem, that her lower jaw was weak. I sure wished that I had solely bottle fed my baby from the beginning, or had at least done both with mostly relying on the bottle (formula). I have felt guilt ever since that time, every time I remember what happened. I was afraid that I was going to lose my baby. That was just over 17 years ago. My daughter is doing fine. I (we) have three wonderful daughters now. Jillian, may God give you peace and strength and provide for your needs.
I can not even imagine the heart ache you indure daily , nightly with out your baby boy.
I am so so very sorry for the loss of such a precious gift . Please , please know you did nothing wrong and have no guilt in his passing .
Please also accept my apology on behalf of the medical community . Please believe the staff would never have wanted this to happen to your family !
As a maternity nurse for 17 years and mother of 3 – we NEVER mean any malice in PROVIDING OUR nursing skills , education or in the care we try to give –
I can assure you !!! No Maternity Nurse or Doctor or provider of care would have ever wanted your son to die .
WE are told how we are to provide care and we are to follow protocols in giving that care –
I do belive that the ” breast is best ” movement has been shoved down the medical fields throats .
I am truly grateful that yours and landons story has been told , as it needs to be heard !!!
It is a story that should help educate the administration on tragic outcomes if we are too rigid in giving —-
” cookie cutter ” patient care –
Every mom and every baby are different .
The medical community should not force everyone to conform to the norm .
I have taken this telling of your darkest day and put it in my heart to help future mothers – I promise
Again , I am soooo sorry . Your angel with be with you always .
My love to your family , Jill R. Rn
You never could have known! What a brave woman you are, my heart breaks for you. Be strong for little Landon. Sending so much love
I am so sorry for your loss!
I am reading your story thinking is this my story being re told by someone else the only difference is on performing CPR we where lucky enough to bring back signs of life!
After arriving back at the hospital they gave my daughter her 1st bottle and it was at this moment I realised that a new born is not ment to cry and cry non stop! She was a completely different baby! I felt horrible because I’m her mum and I feel like I should have known but as a new mum you have no idea and trust what the nurses tell you!
God bless him and the parents. This is so unfair. Please receive all our LOVE ❤️ And I admire your courage to share the heartbreaking story, at least people can learn from your experience and maybe save another baby. Bless you!!!
I’m so very sorry about your son. Reading your story brought tears to my eyes this morning but also a great sense of validation. You see, my hospital was also one of those pro-breastfeeding ones that essentially receives a GRANT for convincing 100% of all moms to at least attempt breastfeeding. I remember in the tour, the guide told us that formula is not given to babies as everyone is encouraged to breastfeed. After having the experience of ONLY formula feeding my first child (she was adopted), I knew that given my daughter’s growth and development during her first year, formula feeding couldn’t be as bad as they made it sound like in the breastfeeding class I attended and in all of the literature I was given through the hospital. I even snuck formula into my diaper bag just in case, feeling very much like it was “contraband.” I tried breastfeeding for 3 weeks but also supplemented with formula, so my son didn’t even lose weight in the first week and gained steadily. But I knew it was because I was giving him formula rather than breastmilk only. Yet even my hubby wanted me to exclusively breastfeed, so I was trying to wean him onto only breastmilk. He grew more and more fussy and began to cluster feed for 6-8 hours a day and longer. I knew he must have been hungry because he wasn’t sleeping for very long — if at all. (My huge passion with my kids when they were babies was sleep training, which actually saved our lives, but that’s another whole story/issue). I knew if my son was constantly latched onto my breast for 8 hours at a time and not sleeping, it wasn’t healthy. One night I did an experiment and gave him only bottles while I pumped. I only got 2 ounces AFTER waiting about 3 hours from the last time I’d breastfeed him! The following morning, I got 4 oz. My son was already taking 3-4 oz per bottle. He was clearly not getting what he needed. That right there was the only proof I needed to know that it was time to switch to formula. Breastfeeding can be a very lovely and wonderful bonding experience, but any benefits that might exist from solely breastfeeding will not happen if a baby is not properly fed. Period. Once I transitioned him to mostly formula, my son began to sleep much better, eat much better, and became an overall happier boy. I’m sure there are many moms who don’t have these experiences, and for whom breastfeeding works well, but that wasn’t our case, and I wasn’t going to let all of the pro-breastfeeding propaganda guilt me into feeling like I was a bad mom because I gave him formula. My heart genuinely weeps for you and other moms and babies who attempt to exclusively breastfeed and it doesn’t work. I’ve seen babies diagnosed with Failure to Thrive in my mommy group, and it’s heartbreaking because they refuse over and over again to offer the babies formula. What’s more important? An agenda or a child’s life? 🙁 Hugs your way and so very very sorry that your son had to pay the ultimate price for this propaganda. 🙁 I’m so very thankful you are sharing your story, though, because it is exactly what I suspect could have happened very easily to my son!
Thank you for sharing your story. If it hadn’t been for a wonderful, caring nurse who was subbing from the gynecological ward, my story would have had the same exact ending. I was in the hospital almost seventeen years ago with my second child. The first child I could not breastfeed because of complications, so this was my first go of it. She constantly screamed and no matter how many times I put her to breast, she wasn’t satisfied. I begged the lactation consultant to please, PLEASE, just let me give her a bottle; she’s starving! And the horrible snot actually said to me, “You just don’t want to be bothered with producing a healthy child because the bottle is easy!” She flat-out REFUSED my requests! Finally, on the day we were to be checked out, a nurse from the gynecological ward was substituting for a regular nurse and she came into our room and found my daughter hoarse from screaming and me bawling. She asked me what was going on and I spilled my guts out to her, right down to the nasty lactation consultant. She exclaimed, “Bullsh*t! This baby is hungry! Hang on a minute.”, went down the hall and brought me a six-pack of formula bottles. She prepped one, handed it to me, and my daughter inhaled that bottle and part of another one! It was the first time she fell asleep and stayed asleep! The nurse told me “For the next 24 hours, if that baby gets hungry, feed it. If you decide to try breastfeeding when your milk comes in, do it. But keep these bottles on hand.” She brought me a week’s supply of bottles! I put in a formal complaint on that stupid lactation consultant, as did I suspect the subbing nurse. It was a nightmare that made me think twice about EVER breastfeeding, as I was afraid I’d run into another dictator consultant. My daughter is now sixteen and in her junior year of high school, thanks to a compassionate nurse. I only wish you had had the same experience. I’m really sorry for your loss.
As I read this blog, I reflect on my personal experience with my son’s birth. We just celebrated his 7th birthday yesterday. At the time of his birth, he was severely dehydrated. The nurses said nothing as they took him from my room and didn’t return. They closed the shades on the infant room and headed me off at the door. I was scared, but I knew my son needed me and I insisted to be there to comfort them. I watched in horror as he screamed while they poked him over and over again with the needle in attempts to find a vein for the IV. They had him under a warming lamp since he was stripped down to his diaper. I noticed he was extremely hot to the touch and beet red. They didn’t have the heat sensor on him to monitor the temperature, so not only was he dehydrated but he was roasting under the lights.
I told them, if he is dehydrated, give him a bottle first then try for the IV. They assumed because he was breastfed, that we would oppose the bottle so they didn’t even bother to offer it. Sure enough, poor baby was hungry. I had inadequate support at the hospital for breastfeeding and no-one thought to check if he was eating enough. I thank God everyday for speaking to me during this time, alerting me that my son was in trouble, and giving me the wisdom and courage to speak up to the nurses.
I am sorry for your little angel and what he went through. I am saddened by your loss and countless others who have experienced the same. Thank you for your bravery and sharing your story. I pray God’s comfort and blessings daily over your family.
Thank you for sharing your story. You did nothing wrong. I too was bullied by nurses, midwives, friends, books, media into breastfeeding exclusively after c-section. My child cried all the time I was exhausted and he was constantly on me. Conflicting confusing advice about bottle preference and latching problems and cup feeding confused me. At 4 weeks I walked out the house and my husband gave him a bottle and thank god we did. He had not returned to his birth weight and looked like a skinny unhappy rat. From that day I saw him smile and he slept his first 6 hours in his short life. Oh how different it could have been. My marriage suffered and my child has mild autism and ADHD which may or may not have been from this. God’s blessings and peace to your family I hope you can move on.
Wow. Thank you for sharing your story. I sobbed through most of your story -remembering my experience as a first time mother. My daughter is now 14. When she was born, she seemed to have a good latch. She cried all the time and I often wondered how much nourishment she was getting. I saw lactation consultants in the hospital and for many months to address feeding issues and concerns about breastfeeding. I spent long hours in the middle of the night with LA Leche league volunteers – supporting me or so I thought. I cried often and felt like a failure that even though I did all that was requested of me, it seemed that I could not satisfy my new baby. I pumped after each feeding (because they said I would produce enough milk if the demand was there). I barely got a tablespoon. They assured me that is was because our daughter was so good at nursing that she barely left any milk. At work, I would pump and only get 1/4-1/2 of an ounce each time after hours….Again they assured me that my milk must be high fat and that she was fine. Her suckle became weak. At that time, they had me use a SNS (supplemental nursing system) a small bottle filled with formula with a very small tube that I taped near my nipple to encourage her to suckle and nurse well. I continually questioned why I was not producing enough. They assured me that my milk may not be plentiful, but was high fat and she was just fine. I listened. I was desperate to breastfeed my daughter. She continued to lose weight. I was continually told that she was fine. I asked questions and the doctors did not seem concerned. Finally I asked to have my thyroid tested as I had been diagnosed with hypothyroidism many years before, but during pregnancy, my levels adjusted and I was told that I no longer needed medication. 4months post partum I was diagnosed with post partum hypothyroidosis. I was taking meds along with several other supplements to increase milk production – tea, fenugreek, brewers yeast reglan etc and nothing worked. I was told that the thyroid had nothing to do with milk production. We now know that the two are related and the medical community now mostly recognizes this. At the time I researched often and finally found a woman’s story that paralleled my own I sobbed feeling that I had finally found my answer. Shortly after this I confronted my doctor. They ran blood tests on my daughter and found abnormal liver results and the beginning of starvation. She was listed as failure to thrive. I was horrified, but as a new mother and not getting answers, I was unsure of all of the right questions to ask and how to proceed. After the failure to thrive diagnosis, we went to formula…. I am truly grateful that we were able to change things. I am so sorry for your loss. Thank you so much for sharing your story and bringing awareness to other moms!!! of note, my thyroid was monitored during my second child’s pregnancy and after and all was within normal limits. Had great milk production and was able to nurse successfully.
Surprised to see that nobody here mentions another breast-feeding problem that we experienced with our first-born. We also had to deal with a baby that would constantly cry and wanting to breastfeed, but was losing weight instaed of gaining. Luckily, my mother, who had raised 8 children, saw that the sucking motions were not what she remembered. The second day, the pediatrician took her worries seriously, examined my baby’s mouth and saw that the frenulum (thin piece of tissue below the tongue) was too large, limiting the tongue to such the milk out of my breasts. It took him 10min to cut the excess frenulum and everything went right after that.
So sorry that black and white thinking wins over mother instincts time and time again.
Thank you for your incredible bravery in sharing your story. When my first daughter was born I took her back to the local hospital after four days because she was not producing enough wet nappies and would not stop crying and feeding. I too was told she was just cluster-feeding and to keep breastfeeding. The next day I took her back to get her weighed for her five day check and they told me to drive her straight to the city hospital because she was dehydrated. She ended up in hospital for five days. Thankfully she completely recovered. I trusted the midwives but they couldn’t look beyond ‘Breast is Best’. I believe that reading this story will give many new mums the courage to trust their instincts and babies will be saved from harm. Thank you.
I am balling my eyes out reading your struggle. My heart is in my stomach, scanning each word as if I wrote it myself. I, too, struggled along this same path until my mother pushed me to begin supplementing after my son cried, and cried, and cried. Always on the breast. Lactaction consultants said, “great latch, good eater”. But he always cried. He kept screaming and “cluster feeding” all the time. My 88 y/o grandma told me he was hungry. I objected. I’d been to several lactation consultants, and they all said he was doing well. Society wouldn’t let me supplement. I would have been a failure at the most important job of my life. But he cried. And he cried. He was hungry. Starving. Deprived. But it’s so ingrained in us that breast is best, and if you don’t BF you’re a bad mom. Well my own mom said, “I give you permission to stop BFing. You’re done. Let’s give him formula.” The mommy-guilt was horrendous. But her essentially, one woman from another, giving “permission” gave me peace.
I am so sorry for your loss and so sorry for your pain. I wish so bad someone would have stepped in for you. Everything after child birth is so chaotic. Sleep deprivation makes it so much harder to have cognitive thoughts and rationalization. God bless you. Your story is so important. Thank you for sharing it. You are a such a strong person. Sending love from Colorado.
This story made a shiver go down my spine when I think how easily we could have had the same outcome for my son, Brendan. My hospital stay was 24 hours, starting from the time he was delivered. Like his sister and brother before him, I made the choice to breast feed. His latch was insufficient and I kept telling the nurses and the Dr. but they insisted he was wetting enough diapers, so home we went. Less than 24 hours after, we were back in the ER. He was dehydrated and weak. The Dr. set me up with a lactation consultant who came to my house a few times a week to help Brendan find his latch. That was 20 years ago. It’s time the “experts” listen to mom’s and their instincts. Thank you for sharing your ordeal; I am so sorry for your loss.
Dear Jillian,
I was heartbroken to read your story. I’m so terribly sorry to read about Landon’s story – I can’t imagine the pain you’ve been through – and still go through. I felt I had to write to you to say thank you for your courage in telling your story. It’s doubly heartbreaking that you say you were scared to tell your story because you were worried you would be judged. I understand those feelings that you could/should have known what was going wrong (you couldn’t) must be so strong some days but please, please know that you were an excellent mother to your son. You followed the medical advice, you tirelessly fed him, you loved him with all your might. You did nothing, nothing wrong.
Your story resonated with me for two reasons. Firstly because you’ve made me see what a near miss I had with my daughter Ally, who is now six. Ally was sent home with me within a few hours of birth. She was my first child. My milk hadn’t come in and her latch wasn’t great. How did I know what a good latch felt like anyway? Everyone at the hospital seemed so delighted that I was breastfeeding, they weren’t too concerned that my milk hadn’t come in. I took her home. The 24 hours we spent at home together are a haze. She tried to feed. She slept a lot. I think there were some dirty nappies – not sure about wet ones… And then suddenly things weren’t right. Her left arm went purple while I was trying to feed her. She seemed a bit floppy. (The woman on the phone from the hospital asked “is she alert? Again how did I know how alert a two day old baby should be? I had nothing to compare her with.)
Anyway we rushed her to hospital and suddenly we were plummeted into the world of very worried doctors crowding round her, putting her on drips, taking needles to her and absolutely failing to tell us that everything would be ok. Her blood sugar was dropping fast. Thankfully I guess we got medical help just in time. They gave her sugars and she seemed to stabilise. Then followed five days of Ally and I stuck in a paediatric ward, trying to make breastfeeding work while the doctors and breastfeeding counsellors argued over whether I should or shouldn’t give her a bottle. I did give her a bottle (despite judgemental questions from a breastfeeding counsellor like “you do know what nipple confusion is, don’t you?”) and we persevered with an insane routine of breastfeeding, pumping and bottle feeding (no-one was there to help me to work, clean and sterilise the pump and my husband wasn’t allowed to stay; so I barely slept at all; no one on the paediatric ward knew much about breastfeeding – we weren’t allowed in the maternity ward because we’d been discharged before we were readmitted). At one point the most helpful breastfeeding support I got was from a hospital cleaner who had breastfed her own children.
Anyway, Ally and I eventually learned to breastfeed and on day five my milk came in. It could have been so different. I’m so incredibly sorry that for you it was. Thank you for showing me how lucky I was. I do hope that sharing your story will help to save lives. Landon looks like such a beautiful little boy. And it sounds like he was so brave and determined. I’m so sorry that the medical system around you let him down. But all he ever knew was your love and care. I don’t know if that brings you any comfort. But I hope you find comfort and strength somehow.
The second reason why your story resonates with me is that my darling nephew Axel, born a couple of years after Ally, died when he was a few weeks old. It was a different story – a seemingly insignificant viral infection that took hold quickly and doctors didn’t pick up on until he suddenly went into cardiac arrest – but I know (only as an outsider, with only a fraction of the intensity of heroic bereaved parents like you and my brother and sister-in-law, Axel’s wonderful parents) how devastatingly strong is the sense that we fail our babies if they die – that we could or should have known how to protect them.
I just wanted to write to you to say you did your best. You loved your son. You fed him night and day. I know that the guilt won’t go because of anything I say but I do hope you will stop feeling scared to talk about what happened. I have nothing but admiration for you. I do hope all is well with your little girl. My second daughter is called Stella too. Xxx
Thank you so much for sharing your ordeal. May God Bless your family always. I am so very sorry for your loss. Your words can educate new Moms and Dads about what can happen after childbirth.
My sons have autism and apparently this developmental disability can sometimes keeps the baby from latching on. This I was unable to breastfeed, so I tried U Tim I cried, and then pumped while Dad bottle fed. I was being bullied to “try harder” to breast feed which of course didn’t work. After some time, we just switched to formula.
I thank you for sharing your story but am so sorry you had to go through this experience. Please do not feel quilts any longer, as I am certain you’ve saved many other babies by education so many adults.
This story brings back sooooo many memories. I had the same beginnings. A healthy 7.6 pound baby girl down to 6.4 at her 4 day appointment, which was 2 days after leaving the hospital. The dr said it was normal and my milk would be coming in very soon. I was still concerned and went to the kactation department at kaiser. They weighed her before and after breast feeding. She latched and seemed to be eating great. They said she was t getting enough and to try to feed her with a tube atttached to my breast. An hour after we got home, I tried to wake up my baby to feed her and she was not moving. I screamed for my husband and we drove like crazy ppl (now I know to call 911). We were not thinking. I thought my baby was dead. We got to the hospital ER the nurse said she is fine, she’s pink. I said, I’m not a crazy first time mom. Something Is wrong. She’s not moving. My daughter was fiesty in uterine and in her first few days of life. The dr tested her blood sugar and it was 51. He said if it went below 50 she could have had brain damage or death. The NICU nurse was called and gave her a bottle. They kept her in the hospital for several days running tests. At one point gave her a test for meningitis because her body temperature went down one night. It was what I thought was my biggest nightmare. The lactation nurse that saw me after I gave birth also came in the NICU. I told her I never had any milk. She said yeah I didn’t think your breast had milk. I think she said she could tell by my breasts. I said why didn’t you tell me that. She said she didn’t want to discourage breast feeding. I said so you’d rather me have a dead baby???? My daughter was released and is now 7 1/2. I knew it was great luck that she survived and with no brain damage. From then on, I preach feed a bottle after breastfeeding. I try and share our story. I am crying with the memories and with the heartbreak for the families that lost their babies by trying to do the right thing and breastfeed like they told us. It is sickening that the lactation department didn’t tell me that my baby was starving to death. It’s criminal. Thank you for sharing this story.
Thank you for sharing. Would you be interested in having us publish your story?
Thank you Jillian. What you shared is so moving and I sobbed reading it. It is a powerful message to new mothers, even second time around as I will be soon – especially those with PCOS as I also have. My daughter cried inconsolably for the first couple of months of life and we tried everything with her, but the only thing that worked was when I started taking Domperidone to increase my milk supply. She lost more than 10% of her birth weight and took a month to gain it back. I’m thankful I had enough milk to keep her alive but for the next baby I will use the medication earlier and be much more watchful and informed this time – thanks to you. Landon is saving many other little babies with his experience and he is their guardian angel. Much love to you Jillian.
I am so so sorry for your loss and thank you so much for being so brave and sharing your story. Although the story has been shared with such a sad ending, it’s great for this information to actually be out there for people who need to be wary of what my husband and I call the “breastfeeding Nazis”. My son is 11 months and luckily very healthy – however he was purely formula fed from 5 months onward. Whilst in the hospital after giving birth, my boobs/nipples got so incredibly sore (bleeding, cracked etc) that I was in agony actually even trying to feed him. Plus, he lost over 10%, but not once was I offered formula to feed him in the meantime and I was watched by the nurses while in tears due to the pain. Once we went home, my husband rushed to the chemist to get some formula as I physically could not put him on my boob again that day without sobbing in pain. After those first few days at home, the guilt of “knowing” I should exclusively breastfeed him kicked in and I went back to just doing that by using nipple shields or expressing milk. For our first 2 weeks at home, we thought we were living in hell. He screamed and cried hysterically sometimes for up to 6-8 hours straight (without sleeping) and this would happen most days. We didn’t realise that babies should really just feed/sleep and not cry that much. After 3 weeks we booked into a Paediatrician as I was beside myself and had no idea what to do. Thankfully, our Paediatrician was amazing gave us some simple advice, most importantly that he wanted me to top up every feed with formula (as I told him I was often breastfeeding up to 1.5-2 hours per feed and he just wouldn’t stop feeding). Being told by a professional that I needed to use formula alleviated the ridiculous guilt I had about doing so. And from that day onward, the hysterical screaming and crying stopped, and our boy loves his bottle.
Unfortunately the push on women to solely breastfeed is so common, but makes me so mad. Of course we all know the phrase “breast is best” and I’m sure it may be, but i totally am with you that “fed is better” and midwives and lactation consultants need to give more rounded information to mums. Sure, give advice on latching issues and how to get more milk in, but never discourage formula. If anything, encourage it and explain that every mum is different and as long as our babies are fed and happy then that’s the most important thing.
My husband and his sister were formula fed and they have turned out fine (besides when he drives me insane 🙂 ) so let’s cut the shit and stop putting so much unwarranted and unneeded pressure on new mums who are already going through enough.
Thinking of you and your family and sending you big hugs from Australia. xx
I’m so sport for your loss!!! How painful!
This article has increase my awareness of how vital it is that babies get milk but also be supplemented when they show signs that they are starving… My baby (now 9 yrs old but struggles with math) cried the first 48 hours and I know she was starving but thank goodness the nurses told me to supplement her with a feeding tube and formula she had lost 1 pound and I was very nervous to think that she wasn’t getting enough milk since my colostrum hadn’t even come in after day three! I’m so thankful for the hospital stuff and I caring lactation nurse!!!
Sorry!