by Jillian Johnson with commentary from Dr. Christie del Castillo-Hegyi
Landon would be five today if he were still alive. It’s a very hard birthday–five. It’s a milestone birthday. Most kiddos would be starting kindergarten at this age. But not my little guy. I wanted to share for a long time about what happened to Landon, but I always feared what others would say and how I’d be judged. But I want people to know how much deeper the pain gets.
I share his story in hopes that no other family ever experiences the loss that we have.
Jarrod and I wanted what was best for Landon, as every parent does for their child. We took all of the classes. Bought and read all of the books. We were ready! Or so we thought….every class and book was geared toward breastfeeding and how it’s so important if you want a healthy child. Landon was born in a “Baby-Friendly” hospital. (What this means is everything is geared toward breastfeeding. Unless you’d had a breast augmentation or cancer or some serious medical reason as to why you couldn’t breastfeed, your baby would not be given formula unless the pediatrician wrote a prescription.)

Sleeping comfortably a few hours after birth
Landon was born full-term weighing 3360 g or 7 lbs. 7 oz, born by urgent cesarean due to fetal intolerance to labor after the water had broken. [Previous publication of this blog said he had an emergency c-section. He was delivered by low transverse incision over 12-14 minutes, which is considered an urgent, not a STAT section.] Apgars were 8 and 9 and he was stabilized. He was transferred 2.5 hours later to the Mother-Baby Unit and returned to his mother. He exclusively breastfed with excellent latch for 15 – 40 minutes every 1-2 hours.

Landon, is 12 hours old.
Landon was on my breast —ALL OF THE TIME. The lactation consultants would come in and see that “he had a great latch and was doing fine,” but there was one who mentioned I may have a problem producing milk. The reason she gave was that I was diagnosed with PCOS (polycystic ovarian syndrome), and it was just harder for women with hormone imbalances to produce milk. She recommended some herbs to take when I got out of the hospital.
While in the hospital, his mother’s risk factors for failed and delayed lactogenesis II (copious milk production) were identified by the IBCLC-lactation consultant. They were borderline diabetes, PCOS, issues with infertility, small, widely spaced breasts with minimal growth during pregnancy, being a first-time mom, and emergency c-section. Despite that, she was encouraged to exclusively breastfeed. She was closely monitored by a nurse, lactation consultant, and physician support. Her baby’s latch was rated as excellent.
By the first 24 hours, he had nursed a total of 9.3 hours, had zero wet diapers and four dirty diapers. By 27 hours, he had lost 4.76%. His nursing sessions became longer and longer until he was on the breast continuously by the second day of life. On the second day, he produced 3 wet diapers and 6 dirty diapers and nursed for almost 14 hours total. By 53 hours of life, he had lost 9.72%.
At this time, the scientific literature on wet and dirty diaper production has shown that the number of diapers produced have no correlation with adequacy of milk intake in the first 4 days of life. The only study on diaper counts has shown that even newborns who lose excessive weight can produce up to 6 wet and dirty diapers a day. In addition, at this time, the Baby-Friendly Hospital Initiative has produced no data on the safety of newborn fasting and weight loss caused by exclusive colostrum feeding and what degree of weight loss protects a child from brain-threatening complications like hyperbilirubinemia, hypernatremic dehydration, and hypoglycemia. So far, the scientific literature shows that babies who lose greater than 7% of their birth weight are at the highest risk of developing excessive jaundice and hypernatremia to levels that can cause long-term developmental disability. It has also been found that 10% of healthy, term, exclusively breastfed babies undergoing the Baby-Friendly protocol experience hypoglycemia to levels that are associated with 50% declines in the ability to pass the literacy and math proficiency test at 10 years of age, even if aggressively corrected.
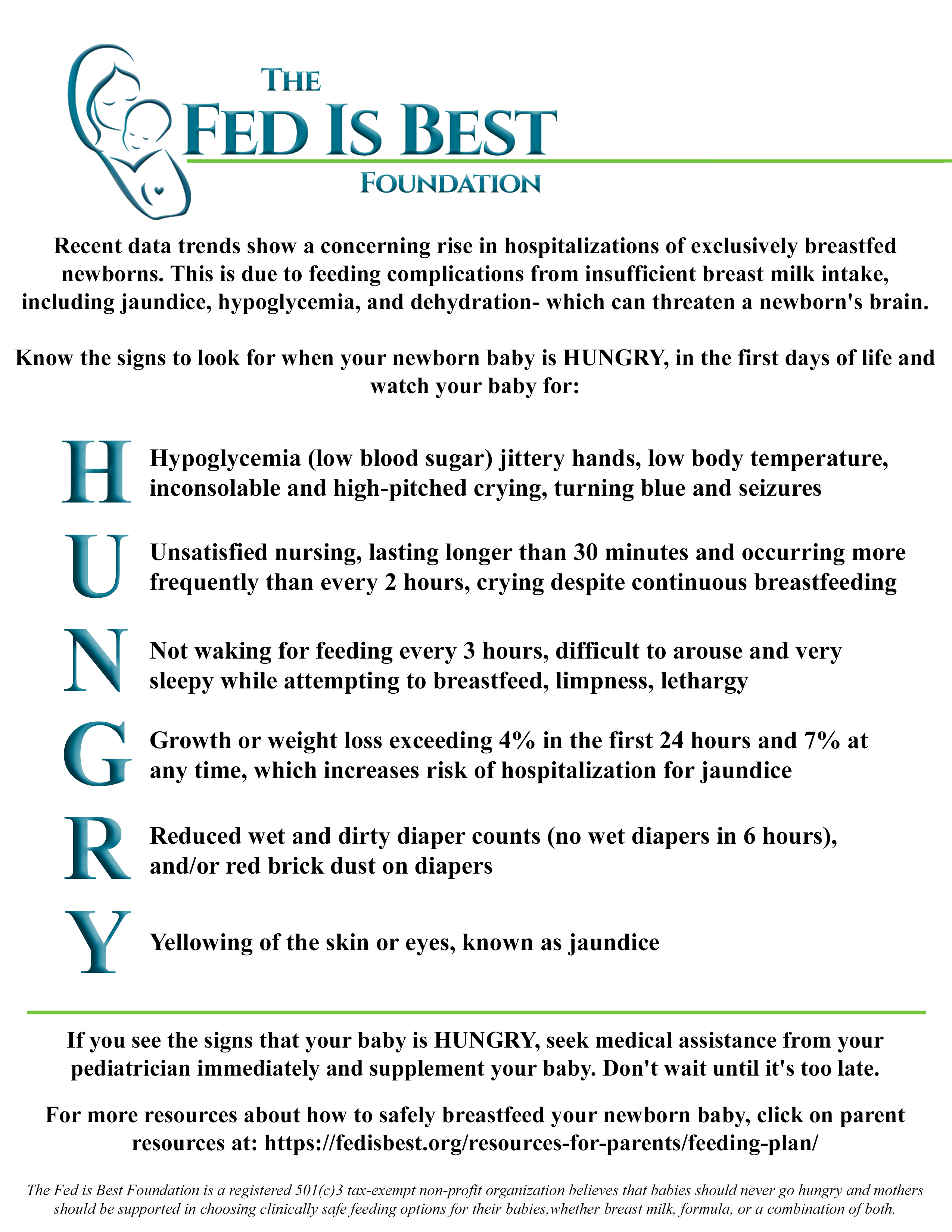
Constant, unsatisfied nursing and inconsolable crying are two of the signs of newborn starvation that lead to brain-threatening complications. If a child is receiving a fraction of their caloric requirement through early exclusive breastfeeding, they can experience severe hunger and thirst, which is why they will cry inconsolably and breastfeed continuously when it is the only source of calories and fluid they are offered. If a mother’s colostrum does not meet the child’s caloric requirement, they will breastfeed for hours a day in an attempt to relieve their hunger. A child who is “cluster-feeding” may actually burn more calories breastfeeding than they receive in return, which can result in fasting conditions and accelerated weight loss. The constant nursing and crying often found in newborns by the second day of life have been called“The Second Night Syndrome” in the breastfeeding industry. This is also whenmothers receive the most pressure to avoid supplementation in order to increase rates of exclusive breastfeeding at discharge. Babies who reach critically low levels of reserve fuel and fluids before their mother’s milk comes in can be found lethargic with compromised vital signs after hours of constant nursing and fussing, at which time they are often diagnosed with hypoglycemia, excessive weight loss, and/or hyperbilirubinemia, all markers of starvation.
Did you know that newborns aren’t supposed to cry all of the time? They’re supposed to eat and sleep and dirty their diapers. I had no idea he was inconsolable because he was literally starving. And when a baby is only on the breast, how do we gauge how much they’re actually getting out? Sure, there should be wet and soiled diapers and weight checks, right? And where is the limit as to weight loss and a minimum for the diapers changed?

Being discharged with visible weight loss.
Landon was discharged at 64 hours (2.5 days) of life having lost 9.7% of his birth weight continuously and exclusively breastfeeding with a mother whose milk had not come in. These are routine and unremarkable findings in newborn babies discharged home to exclusively breastfeed. At this time, there are no studies using standardized developmental testing or serum markers of starvation that show that allowing babies to lose up to 10% of their birth weight protects them from brain- and life-threatening complications, despite wide-spread perception that it is normal for exclusively breastfed babies to lose. Therefore, Landon’s mother was given no instruction to supplement. He was discharged with next-day follow-up.
So we took him home….not knowing that after less than 12 hours home with us, he would have gone into cardiac arrest caused by dehydration from unintended starvation because I was the mother who had no colostrum for my baby. The best advice I was given by one of his NICU doctors while he was on life support is that the breast is best, but follow with the bottle if they are still hungry.
This way you know your baby has eaten enough….if only I could go back in time.
Landon continued to breastfeed at home continuously and was found unresponsive, pulseless, and blue after eventually falling asleep from cluster feeding. His parents called 911. Per EMS, he was asystolic (no heart rate), and he received CPR en route to the local ER. By the time they arrived at the ER, he was found to have pulseless electrical activity (heart rate with no blood pressure). There, he was intubated and received several rounds of epinephrine. He was hypothermic with a temperature of 93.1 F. After 30 minutes of CPR, no cardiac activity was found on ultrasound. With parental consent, CPR was stopped, and he was left on the ventilator while continuing to receive IV saline. Twenty minutes later, with IV fluids, he regained his pulse. He was transferred to a Level III NICU to get the head cooling protocol for babies that experience a brain injury. He was diagnosed with hypernatremic dehydration and cardiac arrest from hypovolemic shock.

Landon is in the NICU on full life support.
I still have many, many days of guilt and questions – what if I had just given him a bottle? And anger because how would I have known? I trusted my healthcare professionals to protect my baby from harm. I remember when Stella, my daughter was born, and she was always quiet. I kept asking the nurses what was wrong with her. They said nothing. She’s doing what she’s supposed to. Sleeping and eating. And it was then that I realized that it wasn’t normal for a newborn to cry as much as Landon did. He was just crying out from his hunger. But I didn’t know. I should’ve known. I still struggle daily, feeling as though I failed him.
Landon received a brain MRI in the hospital which confirmed brain injury consistent with hypoxic-ischemic encephalopathy or brain injury from oxygen deprivation due to low blood pressure from dehydration and cardiac arrest. He was diagnosed with diffuse seizure activity on EEG, the consequence of severe, wide-spread brain injury. Given his poor prognosis, he was taken off life support 15 days later. The autopsy report deemed the causes of death were hypernatremic dehydration followed by cardiac arrest causing hypoxic-ischemic encephalopathy (diffuse brain injury).

Jill held Landon as he took his last breaths.
That little boy gave me ten of the most incredible life-changing months. I’ve been humbled. Challenged. My relationships have fallen apart. Some have come back together. I’ve learned forgiveness. And the true meaning of “life is short.” I love hard – to a fault. But I couldn’t live with myself knowing his death was in vain. I’ve learned so many lessons. I’ve learned the true meaning of compassion and unconditional love.
— Jillian Johnson
The Fed is Best Foundation is dedicated to the prevention of newborn and infant starvation from insufficient exclusive breastfeeding. We do so by studying breastfeeding stories sent by mothers and the scientific literature on breastfeeding complications that lead to infant brain injury and death. Since the beginning of our campaign almost two years ago, we have received tens of thousands of newborn and infant starvation stories leading to the complications of hyperbilirubinemia, dehydration, hypernatremia, hypoglycemia, and failure to thrive. These complications occur because the current breastfeeding guidelines have not been studied for safety and operate with little awareness of the caloric and fluid requirements of newborns nor the amount transferred to babies until complications have already occurred. “Just one bottle” can save a child from these tragedies as it is often a mother’s first clue that a child is, in fact, starving from exclusive breastfeeding.
If your baby is experiencing distress and signs and symptoms of starvation, we encourage you to advocate for your child. We encourage mothers to notify hospital administrators if they are pressured to avoid supplementation to alleviate their child’s hunger. You have the right to feed your child, and your child has the right to be fed. No one but your baby knows how close they are to empty. The only way they can communicate distress is by crying. Listen to your baby and listen to your instincts.
Our message is simple. Feed your baby. Feed them as much as they need to stay safe and satisfied.

How to supplement your baby until your milk comes in:
How To Prepare For Supplementing When Breastfeeding Your Baby In The Hospital
Jillian Johnson: My Message To Parents During World Breastfeeding Week-Just One Bottle
http://fedisbest.org/2022/01/nigerian-mother-speaks-out-about-her-babys-death-after-being-told-to-keep-exclusively-breastfeeding-what-she-wants-human-rights-organizations-to-know/
My Baby Suffered And Almost Died–Why Are The Risks Of Exclusive Breastfeeding Not Taught To Mothers?
Just One Bottle Would Have Prevented My Baby’s Permanent Brain Damage from Hypoglycemia
Feeding Your Baby—When Supplementing Saves Breastfeeding and Saves Lives
U.S. Study Shows Baby-Friendly Hospital Initiative Does Not Work
NICU Nurse Discloses Newborn Admission Rates From Breastfeeding Complications in BFHI Unit
Nurses Are Speaking Out About The Dangers Of The Baby-Friendly Health Initiative
http://fedisbest.org/2018/11/neonatal-nurse-practitioner-speaks-out-about-the-dangerous-and-deadly-practices-of-the-bfhi/
Hospital Drops Baby Friendly Program After Doctors Baby Was Harmed
Letter to Doctors and Parents About the Dangers of Insufficient Exclusive Breastfeeding
Two Physicians Describe How Their Baby-Friendly Hospital Put Their Newborn in Danger
I Supplemented My Baby Until My Milk Came In And We Are Still Breastfeeding At 3 Months
Fed is Best Statement to the USDA Regarding the Harms of the Baby-Friendly Hospital Initiative
Nurses Quit Because Of Horrific Experiences Working In Baby-Friendly Hospitals
Nurses Are Speaking Out About The Dangers Of The Baby-Friendly Health Initiative
“Is Baby-Friendly Safe?”: BFHI Safety Issues Discussed at National Neonatology Conference
CONTACT US/VOLUNTEER
THANK YOU FOR YOUR INTEREST IN THE FED IS BEST FOUNDATION!
Our mission statement is:
The Fed Is Best Foundation works to identify critical gaps in the current breastfeeding protocols, guidelines, and education programs and provides families and health professionals with the most up-to-date scientific research, education, and resources to practice safe infant feeding, with breast milk, formula or a combination of both.
Above all, we strive to eliminate infant feeding shaming and eliminate preventable hospitalizations for insufficient feeding complications while prioritizing perinatal mental health.
HOW YOU CAN SUPPORT FED IS BEST
There are many ways you can support the mission of the Fed is Best Foundation. Please consider contributing in the following ways:
- Join us in any of the Fed is Best volunteer and advocacy, groups. Click here to join our health care professionals group. We have: FIBF Advocacy Group, Research Group, Volunteer Group, Editing Group, Social Media Group, Legal Group, Marketing Group, Perinatal Mental Health Advocacy Group, Private Infant Feeding Support Group, Global Advocacy Group, and Fundraising Group. Please send an email to Jody@fedisbest.org if you are interested in joining any of our volunteer groups.
- If you need infant feeding support, we have a private support group– Join us here.
- If you or your baby were harmed from complications of insufficient breastfeeding please send a message to contact@fedisbest.org
- Make a donation to the Fed is Best Foundation. We are using funds from donations to cover the cost of our website, our social media ads, our printing and mailing costs to reach health providers and hospitals. We do not accept donations from breast- or formula-feeding companies and 100% of your donations go toward these operational costs. All the work of the Foundation is achieved via the pro bono and volunteer work of its supporters.
- Sign our petition! Help us reach our policymakers, and drive change at a global level. Help us stand up for the lives of millions of infants who deserve a fighting chance. Sign the Fed is Best Petition at Change.org today, and share it with others.
- Share the stories and the message of the Fed is Best Foundation through word-of-mouth, by posting on your social media page and by sending our FREE infant feeding educational resources to expectant moms that you know. Share the Fed is Best campaign letter with everyone you know.
- Write a letter to your health providers and hospitals about the Fed is Best Foundation. Write to them about feeding complications your child may have experienced.
- Print out our letter to obstetric providers and mail them to your local obstetricians, midwives, family practitioners who provide obstetric care and hospitals.
- Write your local elected officials about what is happening to newborn babies in hospitals and ask for the legal protection of newborn babies from underfeeding and of mother’s rights to honest informed consent on the risks of insufficient feeding of breastfed babies.
- Send us your stories. Share with us your successes, your struggles and everything in between. Every story saves another child from experiencing the same and teaches another mom how to safely feed her baby. Every voice contributes to change.
- Send us messages of support. We work every single day to make infant feeding safe and supportive of every mother and child. Your messages of support keep us all going.
- Shop at Amazon Smile and Amazon donates to Fed Is Best Foundation.
Or simply send us a message to find out how you can help make a difference with new ideas!
For any urgent messages or questions about infant feeding, please do not leave a message on this page as it will not get to us immediately. Instead, please email christie@fedisbest.org.
Thank you and we look forward to hearing from you!

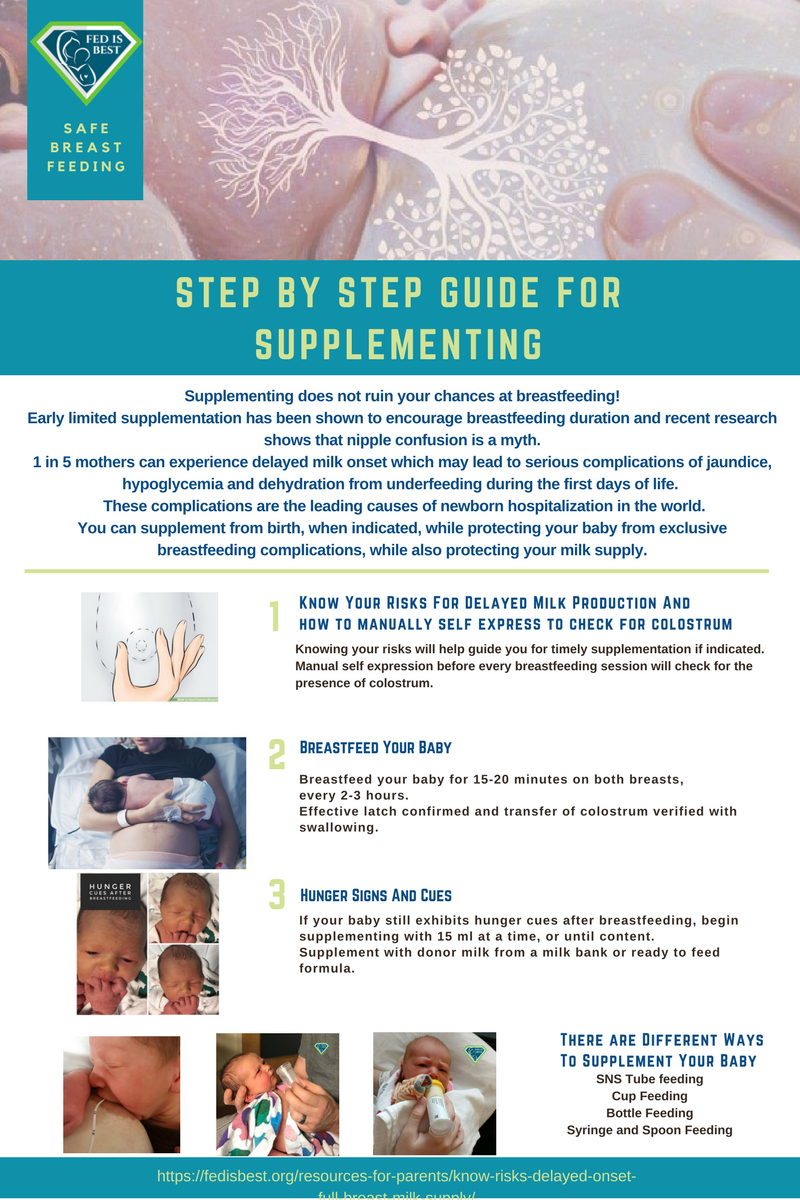
Parents tell us they were not taught how to supplement their babies safely, if necessary to prevent exclusive breastfeeding complications.
For more information on how to protect your baby from feeding complications due to early exclusive breastfeeding, please read and download the Fed is Best Feeding Plan, a way to communicate your feeding choices to your health care providers.
In addition, please read and download the Fed is Best Weighing Protocol to prevent newborn dehydration and failure to thrive.
Lastly, for more detailed information, please watch our educational videos on Preventing Feeding Complications.
Our full list of parent resources can be found on our Resource Page.
If you wish to help parents learn how to protect their newborns from accidental starvation, please share this story and sign our petition to demand that the CDC, the AAP, the U.S. Surgeon General and the WHO/UNICEF Baby-Friendly Hospital Initiative warn parents about the dangers of newborn and infant starvation from insufficient exclusive breastfeeding. Go to http://fedisbest.org/sign-our-petition/.
Please consider making a donation to the Fed is Best Foundation to support its mission of providing safe infant feeding education and support and raise awareness on the harms of insufficient infant feeding.
We believe all babies deserve to be protected from hunger and thirst every single day of their life and we believe that education on Safe Infant Feeding should be free. If you would like to make a donation to support the Fed is Best Foundation’s mission to teach every parent Safe Infant Feeding, please consider making a one-time or recurring donation to our organization.
Donate to Fed is BestThank you so much from the Founders of the Fed is Best Foundation!



Sorry for your loss.
Sound like your son passed away from SIDS.
Weight loss 9.7% should not cause hypovolemic shock and hypernatremia.
I think that metabolic disturbance happened after his last breathing stopped too long from unrecognized apnea (SIDS)
Hello Sai, 9.7% weight loss was the last weigh in at 8 am in the morning. He was losing 5% a day. So by the time he was found unresponsive at 2 am the next day, he was likely 13-14%. He did die of hypovolemic shock because he had 18 more hours of starvation after the last weigh in. My own son was found unresponsive at 15%.
It was NOT SIDS. If you read any of these stories, including mine, you would know it was from starvation. We never got milk and the breastfeeding nazzis did not support bottle feeding. It’s so sad and heartbreaking that babies lives are being lost or nearly lost because new moms are being told not to give a bottle.
I am so so sorry for your loss! Your story left me in shock, and sadness, I think the doctors should have done a better job to prevent this from happening!
I read your story on MSN today and felt compelled to write to you. Thank you so much for speaking out and warning others about this issue. Almost 6 years ago I gave birth for the first time. I also have PCOS and no one ever warned me about the potential lack of milk production or the dangers associated with it. Within 24 hours my daughter lost almost 10% of her birth weight, developed a fever from dehydration and had to be removed from my room for monitoring where they gave her supplemental formula. My daughter continued to scream constantly after being returned to me where I continued to try to breastfeed. At one point I put my pinky in her mouth to soothe her (pacifiers were not given out at the hospital) and realized her mouth was dry. I called the pediatrician we had hand-selected and was told it was impossible for her to be dehydrated so soon. Still, no one told me breast feeding might not be working for me. On day 3, several hours before I was going to be discharged, a lactation nurse took one look at my chest, asked a few questions and easily concluded that this would not work and loaded me up with formula. I feel incredibly guilty sharing this with you because I did not have the same outcome, but please know that your story will undoubtedly save lives. Your courage is humbling and I am heartbroken by your loss.
My heart is broken in sympathy for your terrible loss, but you and your little angel will save lives with your courage in sharing your story. I couldn’t breastfeed because of inverted nipples (one was okay, the other wasn’t), fortunately the lactation nurse didn’t push the issue, told me to keep trying with the good breast to see if I could get some colostrum into my son but that there was no problem with supplementing with formula or just using formula. I see now that I was very lucky in this regard. (It was 2004)
Reading all these stories of all these bullied mothers is heartbreaking. Why are the breastfeeding and medical professionals doing this? Is it worth causing so much pain to vulnerable mothers and babies? Isn’t that the opposite of what they should be accomplishing? It’s incomprehensible.
This just makes me so sad, My oldest is (8) he too named Landon had issues breast feeding the hospital I was in for him had no issues getting him set up on formula, My second son Liam (4) was born in another state is a pro breast hospital where I told them I had issues feeding my first son, I WANT TO BOTTLE FEED, that the nurse pushed and pushed breast for the first day, I was hysterical in tears, that when the pediatrician came in to check on Liam and see me upset she requested formula right away, my husband and mother even said something to the nurses, once we got bottles for Liam it was like we were the shunned the black sheep. It should never happen to any mother in the hospital and is truly amazing that the hospitals still do this and continue to push.
Thank you for starting this campaign! I’m a pediatrician who has been battling this ridiculous, self-righteous movement that has put the concept of exclusive breastfeeding ahead of the baby’s health, well-being, and indeed, the baby’s very life! I’ve had other pediatricians and nurses and department chairs of pediatrics at “baby friendly” hospitals act as if I had ordered cyanide when I ordered a supplementary bottle after breastfeeding for babies whose mom’s milk had not yet come in, or immediate formula for infants of diabetic mothers, who would very likely develop severe hypoglycemia if not fed. The latest fad is lactation specialists who are all diagnosing non-existent “posterior tongue tie” and sending every single infant who falls into their clutches for dangerous invasive laser surgery under the tongue to treat a problem that was never there. I’ve seen babies who haven’t regained their birth weight by TWO MONTHS OLD, due to the mother’s terror of using any of the evil formula. I’ve seen babies whose mothers hoarded pumped milk to stretch it out, saying that if they gave it to their starving infant, they wouldn’t have any left for later, and of course they wouldn’t give formula, God forbid! I’ve seen mothers of infants who looked worse than the pictures of infants from famine-ridden areas of the world, proudly proclaiming that bottle fed babies are disgustingly FAT, and thank God their exclusively breastfed, starved, profoundly underweight infant wasn’t FAT!
A breastfed baby who is getting all he can eat of breast milk actually gains weight FASTER and is HEAVIER than a formula fed infant – IF he’s actually getting enough milk, which at least 25% of the time, is NOT the case! Yet lactation specialists and the huge “breastfeeding support” industry point to breastfed infant growth charts to support their false notion that breastfed infants are naturally thinner than bottle fed infants – which of course is the case when a significant proportion of those breastfed infants aren’t getting enough to eat!
The greatest sin in the world is a hungry infant not being fed, especially when food is available. I am SO sorry for your completely unnecessary loss! I am sorry for all the starving infants, all victims of the self righteous exclusive breastfeeding movement, whose response to the significant percentage of unfed or underfed infants due to exclusive breastfeeding is, “If it’s not working, YOU must be doing something wrong!”
When you have medical professionals not only validating, but encouraging mothers to literally starve their infants, even to the point of death, it’s time for the pendulum to swing back the other way. Thank you for your campaign! Spread the word!
I am so sorry this happened to you and your husband, and I commend you for being brave enough to speak out about this unnecessary tragedy. So much shame is heaped upon new mothers these days. I got a lot of flack for supplementing breast milk with formula. Fortunately, my father is a retired obstetrician who acted as the voice of reason and support. However, I have watched friends suffer and punish themselves in the face of a constant refrain of “breast feed only” or “attachment parenting only”. There is no single “right” way to parent, and new moms should be told to do whatever works best for their baby – but also that they shouldn’t neglect their own needs or punish themselves. I’m glad that you have two beautiful daughters to love, and I hope you know that your little boy did not die in vain. Your courage in sharing your story will save lives.
This almost happened to my son 5 months ago. He’d lost 9% by 24 hrs and I asked if I should supplement, but they said “No, he’s not past 10% yet and he’s got a great latch. We’ll keep an eye on him”… but they didn’t weigh him again before we were discharged. 6 hrs later, he was no longer latching, screaming, and hot to the touch. I brought him back to the hospital and he had lost 15% of his weight and the fever was from dehydration. He was in the NICU for 48 hrs of round-the-clock supplementing, my milk came in and I continued to supplement for another week or so until he completely refused the bottles after breastfeeding. It turned out okay only because I realized he was too hot, but babies often feel hot and I wouldn’t fault any parent who didn’t catch it …AND during that time in the NICU, I got another visit from the lactation consultant who told me again his latch was great, and then suggested I not give him all of the formula the NICU nurses had set out for me!!!! She actually said, ‘I don’t think you need to give him all of that. You don’t want to overfeed him.’ We were in the NICU because he was STARVING!!! I could have punched her.
What a tragic story. I am grateful that I cam across Landon’s story and this site because it actually validated an experience that I had often questioned. Both of my babies were supplemented and I felt like a bad mother. I have heard countless people tell me that it wasn’t necessary. Militant responses that colostrum was all they needed and supplementation was a myth and damaging. I can’t tell you how thankful I am that my first child was born in a hospital in Brazil that while being designated “baby-friendly” did not hesitate to supplement when they saw it was necessary. I was adamant that I would exclusively breastfeed and very suspicious and unhappy about the intervention. My daughter latched and suckled and tore me up and I bled and nothing was coming out (not a drop). She cried non-stop. The nurse on the third day finally said we have to supplement her. And she did and I was miserable and felt like a failure. But my child was calm and we all got a little sleep.I ended up supplementing several other times over those really hard first weeks, but went went on to successfully, exclusively breastfeed till she weaned naturally. My second child was born in a “baby friendly” hospital in the United States. Santa Rosa Memorial Hospital in Santa Rosa, California. I was a wreck after 20 hours in labor and an emergency c-section. I was dehydrated from having gone more than12 hours with nothing but ice chips. I vomited and shook uncontrollably for an hour in a reaction to the anesthetic. For 30 hours my son cried almost non-stop, and I couldn’t hand express a drop of colostrum. The lactation consultant kept stopping by and correcting my position, showing me I was doing it “wrong” and saying not to worry. On day two my mom instinct said he was starving, and remembering my first child, I asked for supplementation. I needed it, he needed it. We were both miserable. But I had to ask three times and it had to be signed off on by the pediatrician before it was finally approved (I nearly sent my husband out to smuggle some in). It took more than an hour to get it. And I was treated with distain. Chastised by the lactation consultant, and lectured on the benefits of breastfeeding by the nurse. But I remembered my experience with my first child and I knew it didn’t have to be all or nothing. I even pointed out that I couldn’t get a drop out (they said his mouth was stronger than my ability to hand express). I prevailed and he supplemented a couple of times in the hospital and at home until my milk finally came in about five days later. (And boy did it come in — I over produced and ended up donating.) Again, my son and I went on to be successful and exclusively breast fed until he stopped on his own at about 18 months. Breast is best, but the reason must also prevail. Now that I have read Landon’s story I feel even more grateful for that first nurse with my first child. If I hadn’t been through it once, I might have made the same call as Jillian – especially with all the push back I got the second time. Heartbreaking and preventable tragedy.
I’m so glad i saw this post in the Washington post today. My kids babies were fine but I couldn’t produce that much milk either. Some but not much so I had to both breastfeed and give them supplement. Also in order to manually get milk out I had to use the pump machine’s from the hospital. ( I was working there at the time) as the store ones didn’t work for me. My oldest is 26 yrs and my youngest one 13 yrs. All this time I couldn’t explain to anyone what was happening. I was ashamed and all these years felt guilty. I tried to tell my step mom but she couldn’t give me any answer. Now after reading this article I feel relieved that’s its not my fault. Now there is a closure. Thank you for educating us.
I feel so so sorry for your loss, Jillian. My heart aches so much while I read this. My son was starved by me after he was born. At the time, as a first time mom, I was so brainwashed by the western doc, the lactation consultant and everybody around me that colostrum will come and just wait. But I guess they had never guessed it took me 10 days! We didn’t feed him water (I was told water is bad too) or any formula for days until I found his color seemed to be more yellow (I am a Chinese) than he should. We took him to the doc and he sent us to ICU right away (his jaundice is at the dangerously high level). We were so lucky he lived. Now I think of it, if it weren’t because of jaundice, we might have still kept on starving him. Oh, my gosh! Being brainwashed is so dangerous! Fed is Best! I hope no babies or parents will have to ever go through this!
Thank you for sharing your story. My heart aches for you and your loss. I too had a similar experience however in desperation among her wails at 3am I finally reached for a bottle. My daughter is now 12 and although I’m grateful she is healthy and well… to this day I still feel guilt and shame over not being able to provide her what she needed.
Moms need to not judge other moms and Heath care professionals need to be more open minded and supportive.
Thank you so much for sharing your story! I could feel your pain and yes I shed some tears because I can relate! When I had my first I was determined that I was going to breastfeed but when I wasn’t making enough (even when the nurses swore I was) and she wasn’t latching (she was tongue tied and I had issues as well) I decided I was going to breastfeed and use formula as a supplement. This went on for 3 months until the last day when I only made 1 ounce in *the WHOLE day* it was a terrible experience, I was stressed out and felt like a failure at the time. After reading this story i am glad that I followed my gut and went with the formula supplement and now that I’m pregnant with my second I will remember your and Landen’s story and keep it close to my heart, thank you again!
Thank you for sharing your heartbreaking story. Fly high little Landon ? X
I am so sorry for your loss. Reading your story brought the memory of my experience flooding back. I am currently sitting next to my 24 year old son, so I know just how lucky I am, and acutely aware that I too could have experienced such a tragedy. I cannot say for sure how I got so lucky, maybe a few bottles of ‘sugar water’ at the hospital, this was 1992 they did that then, made all the difference. I too heard from each and every nurse that entered my hospital room, “he’ll get the hang of it”, “it takes time” and “they don’t need a lot at this stage”, etc. They all meant well, but the reality was that I don’t believe any of them saw me more than once, with shift changes and a weekend ( Sunday into monday ) birth. I had no problem producing milk, but he never learned to latch on. His weight was down from his 7.9 birth weight (which of course is typical, and they are quick to tell you), when we left the hospital. I know there were times when my milk just dripped into his mouth, he would awake every 2 hours and fall back to sleep exhausted, but as I know now, not satisfied. When I spoke to the Lelache league representative that I had taken a breast feeding class with I was again told “he’ll get it, it takes time” and “don’t give him a bottle”. At 1 week of age he awoke one morning and his breathing was shallow and quick. We went directly to the doctors and he was dehydrated, and diagnosed as “failure to thrive”. Seeing those words were devastating for me. I felt like a failure, how could I have not known, or seen. He was down to 5.9 lbs. The clothes he came home from the hospital in now hung on him. Needless to say he was on a bottle from that day on. I consider myself very lucky. I wish I had pursued the issue with the hospital at the time. I hate the thought that other families have gone through this too. First time mothering is difficult, and lack of sleep puts you at a disadvantage. It is a sad state of affairs and hospital staff need to be trained in recognizing whether a baby is getting adequate sustenance whether it be breast or bottle. Thank you for sharing your story and helping people realize that they are not alone. I was truly amazed at the number of posts from women with similar stories. I wish you all the best, continued courage and healing.
Wow. Dozens of stories or women, doctors and midwifes allowing babies to starve, sometimes to death, due to ignorance and pride.
This is one of the most horrifying post and comments I have ever read.
I am so glad you shared your story. I nearly lost my first grandson because my daughter’s midwife was adamant that she not supplement with a bottle even though her son was not latching on well and by the second day was becoming lethargic. I had breastfed all my babies, but I’m not so fanatical as to ignore what was happening unlike my daughter’s midwife. I was finally able to convince my daughter to supplement by bringing a friend who is a nurse-midwife to see her and give a second opinion. Her son began perking up immediately after his first bottle. She was eventually able to nurse him successfully as well as her other three children, but had I not been there I don’t know what might have happened. I am so sorry for your loss, but I hope that sharing your story will save lives.