Dear Colleague and Parent:
My name is Christie del Castillo-Hegyi and I am an emergency physician, former NIH scientist, with a background in newborn brain injury research at Brown University, and mother to a 6-year-old child who is neurologically disabled. I am writing to you because my child fell victim to newborn jaundice, hypoglycemia and severe dehydration due to insufficient milk intake from exclusive breastfeeding in the first days of life. As an expectant mom, I read all the guidelines on breastfeeding my first-born child. Unfortunately, following the guidelines and our pediatrician’s advice resulted in my child going 4 days with absolutely no milk intake requiring ICU care. He was subsequently diagnosed with multiple neurodevelopmental disabilities. Being a physician and scientist, I sought out peer-reviewed journals to explain why this happened. I found that there is ample evidence showing the links between neonatal jaundice, dehydration, hypoglycemia, and developmental disabilities. I wish to explain to you how I believe this could apply to my son and the many children whose care you are entrusted with.
I was an attending physician in the hospital where my son was born at Downtown Presbyterian Hospital in Albuquerque, New Mexico. My son was born 8 pounds and 11 ounces after a healthy pregnancy and normal uneventful vaginal delivery. He was placed directly on my chest and was nursed immediately. He was nursed on demand for 20-30 minutes every 3 hours. Each day of our stay in the hospital, he was seen by the pediatrician as well as the lactation consultant who noted that he had a perfect latch. He produced the expected number of wet and dirty diapers. He was noted to be jaundiced by the second day of life and had a transcutaneous bilirubin of 8.9. We were discharged at 48 hours at 5% weight loss with next-day follow-up. We were told by the lactation consultant before discharge that he would be hungry and we were instructed to just keep putting him on the breast. Upon getting home, he became fussy and I nursed him longer and longer into the night. He cried even after nursing and latched back on immediately. He did not sleep. By the next morning, he stopped crying and was quiet. We saw our pediatrician at around 68 hours of life (end of day 3). Despite producing the expected number of wet and dirty diapers, he had lost 1 pound 5 ounces, about 15% of his birth weight. At the time, we were not aware of and were not told the percentage lost, and having been up all night long trying to feed a hungry baby, we were too exhausted to figure out that this was an incredible amount of weight loss. He was jaundiced but no bilirubin was checked. Our pediatrician told us that we had the option of either feeding formula or waiting for my milk to come in at day 4 or 5 of life. Wanting badly to succeed in breastfeeding him, we went another day unsuccessfully breastfeeding and went to a lactation consultant the next day who weighed his feeding and discovered that he was getting absolutely no milk. When I pumped and manually expressed, I realized I produced nothing. I imagined the four days of torture he experienced and how 2 days of near-continuous breastfeeding encouraged by breastfeeding manuals was a sign of this. We fed him formula after that visit and he finally fell asleep. Three hours later, we found him unresponsive. We squeezed a few milliliters of formula milk into his mouth, which made him more alert, but then he seized. We rushed him to the emergency room. He had a barely normal glucose (50 mg/dL), a severe form of dehydration called hypernatremia (157 mEq/L), and severe jaundice (bilirubin 24 mg/dL). We were reassured that he would be fine, but having done newborn brain injury research, knowing how little time it takes for brain cells to die due to hypoglycemia and severe dehydration, I did not believe it, although I hoped it.

Born healthy, full-term weighing 8 pounds 11 ounces getting skin-to-skin and immediate breastfeeding after birth

The third day of life after the pediatrician visit. He was no longer crying and he was jaundiced and dehydrated with 15% weight loss. We were reassured that we could keep exclusively breastfeeding.

Hypernatremic dehydration and encephalopathy from brain injury. Blank staring is a hallmark of newborn brain injury.
Watch the Doctors Show Interview
At 3 years and 8 months, our son was diagnosed with severe language impairment, autism, ADHD, sensory processing disorder, low IQ, fine and gross motor delays. He was later diagnosed with a seizure disorder associated with injury to the language area of the brain. Since my child’s diagnosis, I have been researching the scientific literature on breastfeeding insufficiency, newborn starvation, brain injury, and developmental disabilities for over three years. In addition, I have collected similar breastfeeding stories of tens of thousands of women through social media.
In the September 2015 issue of Hospital Pediatrics, an article was published describing 11 exclusively breastfed newborn babies who developed profound hypoglycemia between the second and fifth days of life from insufficient breast milk intake. The child described in the body of the article was a healthy full-term baby who presented just like my son. He was seen on the third day of life at his pediatrician’s office. Despite that, he was found on the fourth day of life lethargic and unable to feed. He had lost 10% of his birth weight and had a low glucose of 20 mg/dL (normal > 47 mg/dL). This child was given IV glucose after which he developed a seizure. They obtained a brain MRI which showed extensive areas of injury to almost the entire brain. In addition to this child, 10 other healthy term newborns were identified to have developed hypoglycemia from insufficient breastfeeding as well. They were found lethargic, seizing, hypothermic and/or not breathing. 5 out of the 6 MRIs obtained in these babies showed widespread injury to a third to almost the entire brain in varying patterns. They subsequently developed long-term neurological disabilities including seizure disorders, motor weakness, visual impairment and feeding difficulties requiring speech therapy.
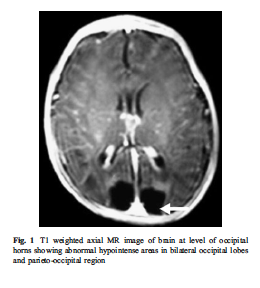
The brain MRI of an exclusively breastfed baby who developed lethargy and hypoglycemia (20 mg/dL) by day 3 of life from insufficient breast milk intake. The dark areas in the posterior part of the brain are the areas of missing brain tissue that resulted one month after the episode of hypoglycemia.
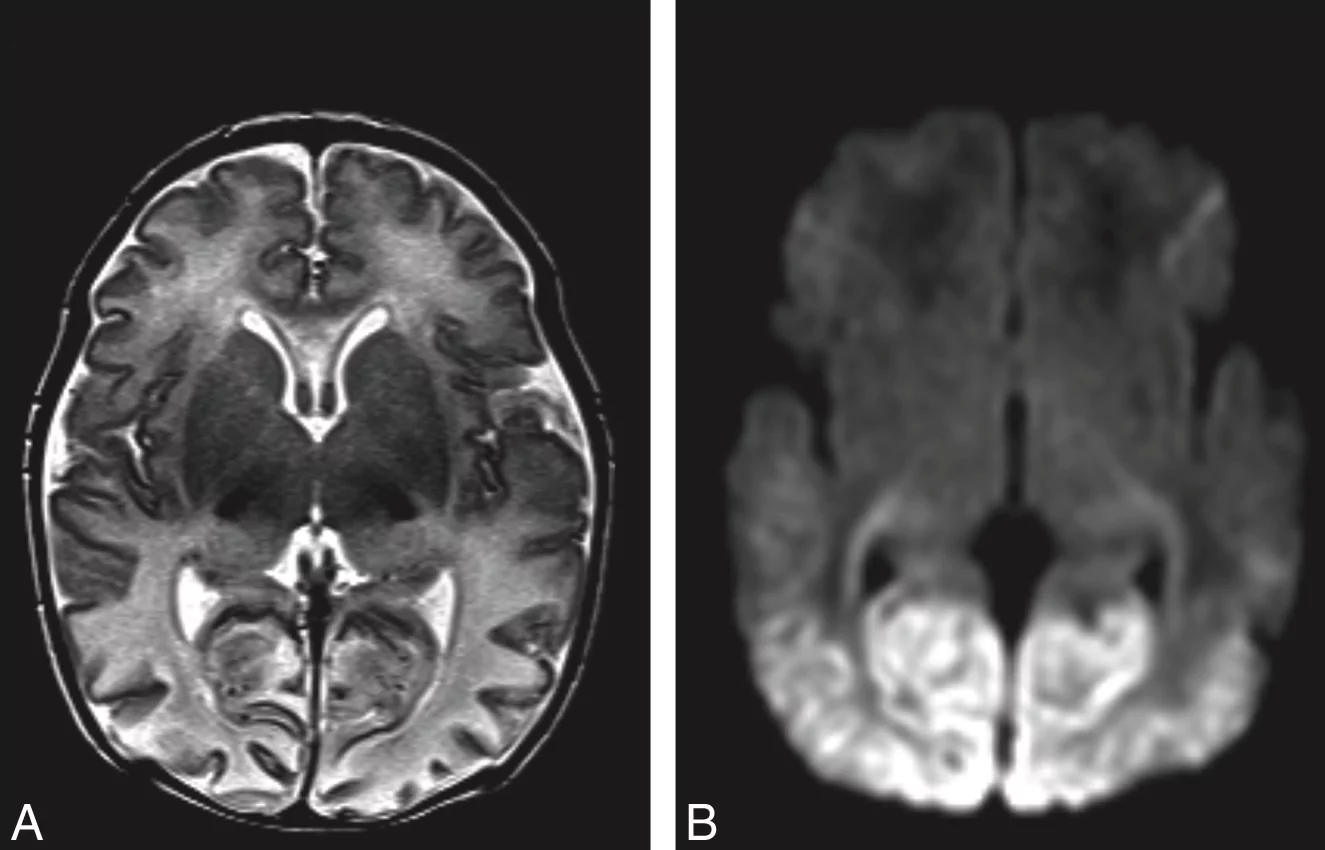
Brain MRI of acute hypoglycemic brain injury. The light appearance in the posterior part of the brain is swelling and injury caused by caloric deprivation to brain cells due to hypoglycemia.
The answer to the epidemic of developmental disabilities we are seeing may be found in this vulnerable period. The risk factors for neurological disabilities in children all have to do with brain injury caused by excessive jaundice, loss of oxygen, circulation, and glucose delivery to the brain. These include pre-eclampsia, intrauterine growth retardation, and prematurity, which are caused by poor function of the placenta and decreased circulation to the baby. Hypoglycemia, umbilical cord prolapse, nuchal cord (cord wrapped around the neck), fetal distress, low Apgar scores, respiratory distress, and other labor complications, events that all cause perinatal brain injury also cause long-term neurological disabilities. Although there are many causes of newborn brain injury that we have no control over, we have control over whether or not a child is fed enough for all their brain cells to survive. I believe we may be inducing hypoglycemic brain injury to many newborns by asking mothers who may not be producing sufficient milk for their newborn’s physiologic need to exclusively breastfeed. We are potentially putting ourselves at odds with the protective natural instinct to respond to a baby’s cry by telling mothers that their colostrum is enough (which for many it may not be) and by making them fear failure by giving their child supplementation when they need it.
My child’s story is not rare. In a study of 280 mother-baby dyads, 22% of motivated mothers intending to exclusively breastfeed who received close lactation support experienced delayed onset of copious milk production, or lactogenesis II, which put her child at 7-fold increased risk of excessive weight loss greater than 10%. This means more than 1 in 5 newborns are at risk of excessive weight loss and the associated complications if exclusively breastfed from birth. In another study, it has been found that 10% of well-monitored exclusively breastfed babies undergoing the Baby-Friendly Hospital Initiative protocol develop hypoglycemia of less than 40 mg/dL within the first 48 hours. This incidence was even higher in babies born to first-time mothers as 23% developed hypoglycemia. This level of hypoglycemia has been shown in other studies to result in brain injury on MRI and long-term declines in cognitive function. One study showed that a glucose of less than 46 mg/dL within the first 24 hours of life was associated with a 3.7-fold increased risk of brain injury on MRI and a 4.8-fold increased odds of lower motor, cognitive and language scores at 1 year of age. This cognitive impairment persists as evidenced by another study of 1395 newborns showing that newborns who develop transient hypoglycemia of less than 40 mg/dL had a 50% reduction in passing their fourth-grade proficiency test in literacy and math. Even glucose less than 45 mg/dL resulted in a 38% reduction in passing the literacy test. The current standard of care tolerates a glucose between 25 and 45 mg/dL when there is evidence that those levels of hypoglycemia result in long-term lower academic achievement and developmental disability.
I hope you feel the same sense of urgency that I do. Since we received our diagnosis, I have come to personally know 43 mothers whose children experience starvation-related complications from exclusive breastfeeding, including pediatricians, other doctors, nurses and lactation consultants. All of them have children with long-term neurodevelopmental impairments. While the literature cites poor education in breastfeeding as the cause of these starvation-related complications, in my research of breastfeeding mothers, it is the most educated in breastfeeding that are at the highest risk. The least educated will respond to a baby’s cry by offering a bottle. The mothers that are most educated in breastfeeding are the ones who have been taught that offering just one bottle will ruin her breastfeeding and potentially harm her child. I have learned that this is a distortion of reality created by breastfeeding education to pressure mothers to exclusively breastfeed that can put her child’s life at risk.
I am writing to let you know I believe the current newborn exclusive breastfeeding guidelines of the Baby-Friendly Hospital Initiative are dangerous. My son suffered an incredible amount of weight loss by the third day, which is often when mothers produce milk. How many newborns are experiencing this same fate? To date, there are no rigorously done studies on the safety of newborn weight loss and exclusive breastfeeding before lactogenesis II on the newborn brain. In fact, a study has shown that exclusive breastfeeding at discharge is associated with an 11-fold higher risk of rehospitalization for underfeeding and dehydration, which few parents are informed of.
I would like to advocate for a patient safety initiative to increase monitoring and supplementation to prevent adverse neurologic conditions in all exclusively breastfed newborns as described by the following:
1) Mothers should be instructed on how to manually express to confirm the presence of milk, which is available through this link. Any baby whose mother has little to no colostrum should be offered supplementation immediately.
2) Twice daily weighing for exclusively breastfed newborns in the hospital and at home as it has been shown that the least-fed newborns can lose the maximum recommended weight loss of 7% within the first 24 hours. This practice should be continued at home until breastfeeding meets the child’s full metabolic requirement as signaled by the onset of daily weight gain. The 7% weight loss threshold should be provided to the mother to help signal the need for supplementation in the hospital and at home.
3) Universal daily transcutaneous bilirubin checks and glucose monitoring while in the hospital for exclusively breastfed newborns before the onset of daily weight gain as the scientific literature has now identified them as a high-risk population for hypoglycemia. The physical exam is insufficient to rule out hypoglycemia and pathological hyperbilirubinemia. Any inconsolable child should also have a glucose check as this is an often-missed sign of hypoglycemia. Supplementation with breast milk or formula as well as IV glucose should be given immediately at a glucose level less than 47 mg/dL as this is the only prospectively validated glucose threshold that if corrected immediately prevents the development of developmental delay. Supplementation should also be offered for bilirubin levels exceeding 15 mg/dL or any level considered high risk on the bilirubin nomogram. Not only does supplementation for underfed newborns protect a child’s brain and stabilize glucose but it also doubles the rates of exclusive breastfeeding at 3 months.
4) Pre- and post-breastfeeding weights after lactogenesis II to measure the amount of milk transferred to the baby. The caloric requirement of a newborn baby is 100-120 kcal/kg/day and a mother’s production should be around 2.7 oz/lb/day or 6 oz/kg/day (roughly 2 ounces per feed every 3 hours) to sustain a newborn and prevent feeding complications. Some babies with medical conditions may need more than the above volumes.
5) Next day after discharge follow-up with pediatricians and lactation consultants with universal bilirubin and glucose checks in the office. Children who are crying inconsolably at home especially before lactogenesis II should be supplemented after nursing UNTIL they reach their health care provider in order to prevent the development of hypoglycemia, dehydration and negative neurological consequences.
6) I advocate for mothers to be informed of the possibility that her child can become dehydrated, jaundiced, and hypoglycemic from insufficient breast milk intake and that these conditions can cause developmental and neurological disabilities. Signs of this are a child that is not sleeping or crying repeatedly after breastfeeding as well as nursing near-continuously. Lethargy, poor feeding, seizures, hypothermia (low body temperature), and bradycardia (slow heart rate) are late signs that suggest the presence of profound brain injury from near-complete glucose deprivation to the brain. Lethargic hypoglycemic babies deserve a brain MRI to provide vital information to parents so that they can closely monitor their development and obtain early intervention as needed.
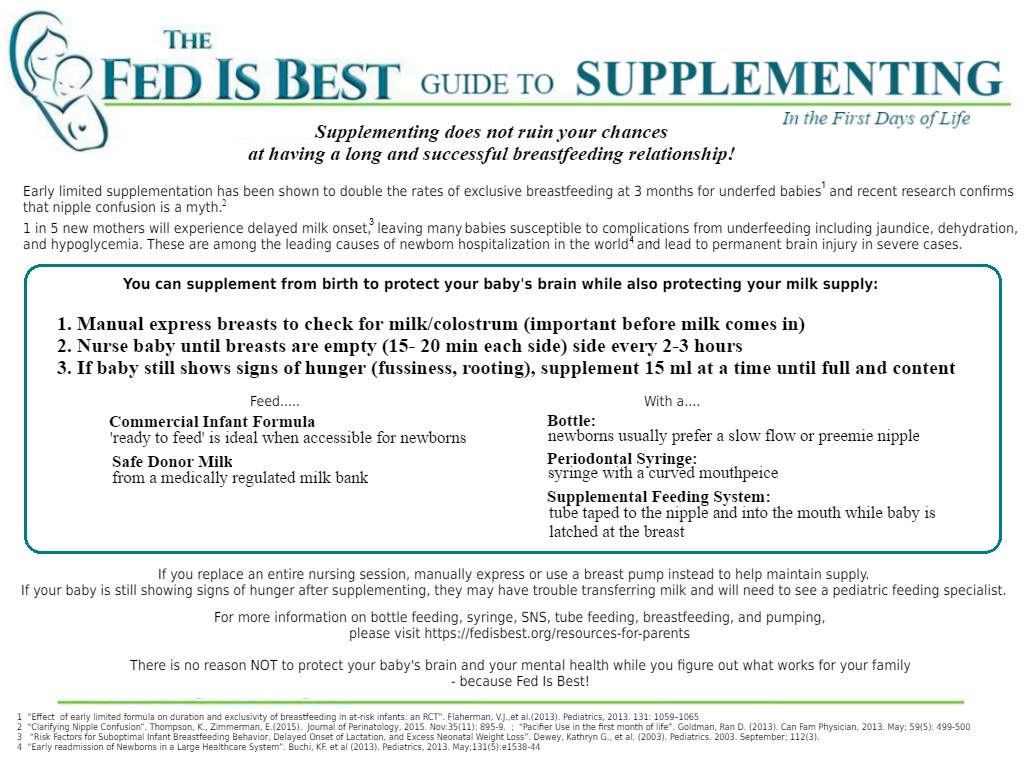
7) Every mother should be educated on supplementation after nursing in order to continue the stimulation needed to promote milk production in case the need for supplementation arises, particularly before discharge if lactogenesis II has not occurred. If a child is hypoglycemic, greater than 7% below the birth weight, hyperbilirubinemia, hypernatremic or crying inconsolably out of hunger, supplementation can be offered 15 MLS at a time as the newborn stomach has been in fact measured to be 20 mL in size at birth, much larger than commonly taught to mothers and health professionals. Supplementation should be offered until a child’s laboratory markers are corrected and the child is no longer in distress. A child’s brain will not wait for food. Once the child is adequately fed, the breastfeeding may then be evaluated to identify the cause of underfeeding. Supplemented breastfeeding is a valid choice as NO BENEFIT of exclusive breastfeeding justifies the risk of life-long disability caused by hypoglycemic brain injury. Any mother sent home before full milk production without a supplementation plan is being sent home to potentially starve and disable her child if her milk does not arrive on time.
Mothers are taught by breastfeeding manuals that they will uniformly be able to produce enough milk for their baby’s needs and will feed them near-continuously for weeks without question if their doctors and lactation consultants tell them not to give formula. But as you have witnessed as a matter of routine, breastfeeding jaundice is very common and mothers do not uniformly produce enough milk for their babies’ needs. The learned wisdom of grandparents who know instinctively the sound of a hungry baby is being supplanted by breastfeeding manuals that cannot teach that sound to the new parent. If you observe non-Western cultures all around the world, babies are given pre-lacteal feeds or milk through wet nurses when mother’s milk is not enough in the first days of life and beyond because instinctively, we as a species protected our newborns by responding to their hungry cry. Thousands of years of evolution have wired mothers to respond to this cry and we are interfering with a biologically protective instinct by telling mothers that their child is getting enough when it is apparent to them that they are not. Babies get admitted to the ICU lethargic, jaundiced and dehydrated every day because their mothers did not know it was possible to have insufficient milk. The most recent publication on hospitalizations for newborn jaundice at a hospital system with high exclusive breastfeeding rates showed that out of 104,468 babies born in a 3 year period, 12.4% of newborns developed excessive jaundice and 5.7% needed hospitalization for phototherapy, the majority of these cases completely preventable with early supplementation. That means millions of babies have been hospitalized since the 1991 publication of the Baby-Friendly Hospital Initiative which codified this protocol. The Baby-Friendly Hospital Initiative and the WHO breastfeeding protocol protects the breastfeeding more than it protects the baby and countless babies have endured days, weeks, and even months of hunger in order to meet its goals.
The time for magical thinking has ended. Breastfeeding education is based on many premises not consistent with reality. Individual health professionals and even mothers have been blamed for accidental infant starvation when in fact, it is the system of breastfeeding education that fails to adequately educate and counsel health professionals and parents on the serious risks of insufficient feeding from exclusive breastfeeding. No time in the history of this planet have we allowed babies to cry out for milk for as long as we tolerate for the purpose of breastfeeding. The first law of nature is and has always been that Fed is Best. Many parents are led to harm their own babies because of what they have been taught about breastfeeding. As you can see, if such a severe case of jaundice and dehydration can occur to two physicians taking home their first-born son, it can happen to anyone.
To all doctors and parents, my message is simple. Feed your baby. Provide your baby its physiologic needs every minute, including the days before milk production. The only person who knows what a newborn needs is that newborn. The accidental starvation of a newborn child is a tragedy by any definition. We are allowing newborns to receive less than their nutritional requirements and telling parents that they are doing what is best for their children. We must be certain an infant is actually getting fed by every available mean. I hope you join me in informing your colleagues, friends, and family of the data and make changes to your practice. Please feel free to share this letter with whomever you wish.
Respectfully,
Christie del Castillo-Hegyi, MD
[email protected]
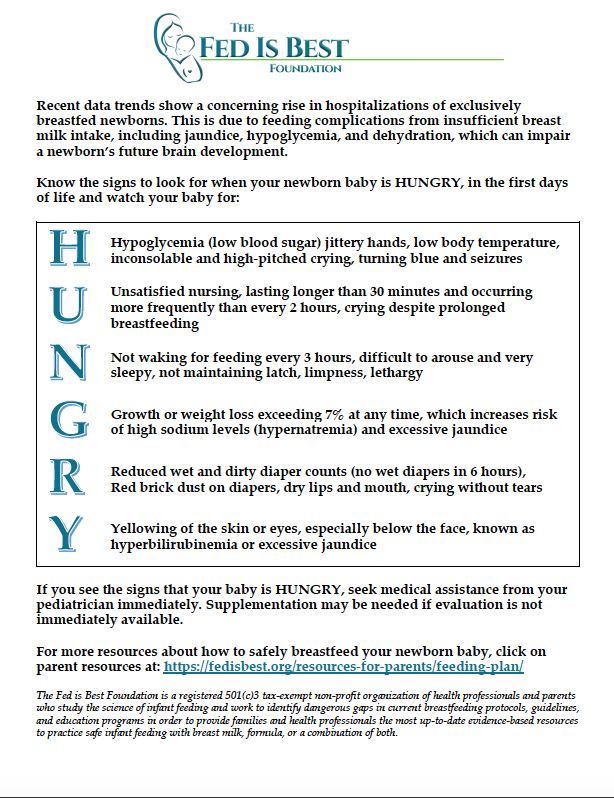
Unfortunately, serious complications occur routinely among newborns who undergo the Baby-Friendly exclusive breastfeeding protocol, namely excessive jaundice, excessive weight loss, dehydration, hypernatremia and hypoglycemia. We would like to help your family protect your baby’s future.
Read the Stories of Thousands of Families, Nurses and Physicians Who Signed the Fed is Best Petition
If I Had Given Him Just One Bottle, He Would Still Be Alive.
Hospital Drops Baby Friendly Program After Doctors Baby Was Harmed
Two Physicians Describe How Their Baby-Friendly Hospital Put Their Newborn in Danger
Jillian Johnson: My Message To Parents During World Breastfeeding Week-Just One Bottle
NICU Nurse Discloses Newborn Admission Rates From Breastfeeding Complications in BFHI Unit
Nurses Are Speaking Out About The Dangers Of The Baby-Friendly Health Initiative
Neonatal Nurse Practitioner Speaks Out About The Dangerous Practices Of The BFHI
Information for Hospitals: Ensuring Safety for Breastfed Newborns
Fed is Best Statement to the USDA Regarding the Harms of the Baby-Friendly Hospital Initiative
Dangers of Insufficient Exclusive Breastfeeding Grand Rounds Presentation
National Women’s Health Advocate Describes How A Baby-Friendly Hospital Starved Her Baby
Nurses Quit Because Of Horrific Experiences Working In Baby-Friendly Hospitals
How To Prepare For Supplementing When Breastfeeding Your Baby In The Hospital
To learn more about the Fed is Best Foundation, please go to our About page.
Disclaimer: This document does not replace in-person physician evaluation and treatment. This document is meant to inform parents of the most recent data regarding infant feeding and to increase their knowledge on how to protect their newborns from hyperbilirubinemia, dehydration, hypernatremia, hypoglycemia and extended or repeat hospitalizations due to complications from underfeeding. Earlier supplementation may be needed for babies who are premature or have medical conditions. It is recommended that a parent seeks evaluation by a pediatrician for any concerns regarding the health and safety of her baby if they arise.


Hi Chrisite,
I've been meaning to share with you for sometime since you started posting your research on jaundice and newborns that Chris and I experienced a similar situation with Joshua when he was born. I too was wondering two days after giving birth when my breast milk was going to come in and feeling helpless with my child crying in my arms for food. Joshua was getting tiny doses of my colostrum but of course it's not enough for a hungry infant. I noticed Joshua was looking a little yellow and felt it wasn't right. On our scheduled visit to see our lactation nurse on the fourth day since Joshua's birth she decided formula was going to be needed as a supplement until my breast milk arrived.
I was apprehensive, I too was dedicated to breast milk 100% without the interference of formula. I was a first time mom at forty and chose to give birth naturally. Surely mother nature wasn't going to let me down with my milk, I was thinking. But, my child's well being was at stake and did not want him to look unhealthy anymore. And, once he had formula, Joshua and I rested more peacefully. Once I was able to nurse him with breast milk it was a seamless transition to stop using formula.
After reading your articles, I can't believe how close to danger Chris and I were with Joshua. I can only say we were lucky and blessed that he came out fine once he was given formula. There should be standards set in educating new parents about the risk of neonatal jaundice. Had I known, I would have made a different decision early on regardless of my holistic beliefs and choices.
I applaud you dear cousin and I'm proud of what you're doing. Everything is not just black and white in this world. As parents we must consider and be open to all options and be educated thoroughly with our choices when it comes to our children from prenatal to postnatal. To put an infant's life at risk over simple assumptions and educated guesses of what a mother's body will do eventually to feed her child is an anguishing thought which I can't believe has been going on for so long. What you're doing is important work and I support you wholeheartedly. I will do what I can to spread the word to anyone that will lesson until things finally change. Good job Dr. del-Castillo Hegyi!
This could’ve been my daughter thank god the doctor rechecked her bilirubin and MADE me give her formula. So sorry this happened.
I have cared for moms and babies for more than 34 years. After more than 20,000 babies, I have learned to respond quickly and supplement sooner vs later. Many nurses don’t tell moms that they should force their own fluid intake. A huge number of moms become severely dehydrated themselves from the birthing process. One novel idea is to establish milk production prior to delivery and freeze the acquired colostrum to feed your newborn as a supplement if needed. Some moms are using electric pumps to establish milk production prior to delivery starting at 37.5 weeks gestation. Moms of today appear to have less colostrum production than in years past. This may be due to toxins in our environment, hormones in our meat or perhaps due to the over use of pitocin and pain killers. Moms who have had unmediated deliveries, we call them stop and drops and who refrain from taking Motrin, Norcos, Tylenol with codeine appear to have a greater abundance of colostrum. Over the years, I noticed that moms would start out with plentiful colostrum but then it appeared to dwindle as the mom received more post partum pain meds. Thermacare hot packs might be a better option for pain control. I also encourage my mom’s to drink water simultaneously as they nurse. This practice often triggers bigger, bolder letdowns of colostrum and breast milk. I also educate parents that babies don’t cry without a good reason. My book is entitled: Pampering Parents; Empowering Parents One Baby At A Time by Victoria Bidlack, BSN, RN by LitFire Publishing 2016.
Mommy, how come you did not noticed that you do not have milk?..i am sorry for the baby..may God bless him for early recovery…
I am also a mom with 1 yr old baby. i did not listened to my doctor the first time she insisted/instructed me to feed my baby since i wasnt also able to produced milk. i insisted them to feed formula just to feed the baby while i was waiting for my milk to come out.
.
Thanks for sharing. This has hit close to home for me. Trying to breast feed a 9lb 10oz baby for 4 days before trying to pump and realising there was hardly any milk. Dylan lost over 10%of his weight unsurprisingly. And diagnosed recently with autistic spectrum disorder. Let’s hope for more research and promotion of feeding by any means necessary
Did
I believed is up to every individual on breast feeding situation. I am a Live Clean Practitioner. For years scientists have thought that chemical pollution is only in the air, water, land and food. Now they have discovered that industrial pollution is in our bodies. Our chemical exposure, in fact begins in the womb- hundreds of industries chemicals, pollutants and pesticides are pumped back and forth from mother to baby through umbilical cord blood, affecting babies during vital stages of development. In other words before we are even born, synthetic chemicals and heavy metal of all kinds begin building up in our bodies.
Hard to believe ? Here is the proof.
In USA
EWG, based in Washington, DC lab studies found an average of 200 industrial chemicals and pollutants in blood from 10 babies born in August and September 2004 in US hospitals. A new science has measure toxins in people, the human body burden – tested each sample of umbilical cord blood of 413 industrial and consumer product chemicals.
Tests, done on the babies’ umbilical cord blood after the cord was cut, detected a total of 287 chemicals in the blood. The pollutants include consumer products ingredients, ban industrial chemicals and pesticides and waste byproducts. According to the report, of 287 chemicals detected in umbilical cord, 180 are known to cause cancer in human or animals, 217 are toxic to the brain and nervous system, and 208 causing birth defects or abnormal development in animal tests.
The babies in the study were exposed to poison in their blood before they even take their first breath!
According to the EWG, ” the danger of pre- or post-natal exposure to this complex mixture of carcinogen, development toxins and neurotoxins have never been studied”
However the chemical exposure in the womb or during infancy can be dramatically more harmful than exposure in later life, the reports warn.
In the Netherlands
A recent study by Greenpeace Netherlands and WWF-UK found that babies in the womb are being contaminated with hazardous non-stick chemicals, flame retardants, perfumes and other gender -bending chemicals.
In the study , tests on blood taken from the umbilical cords of nearly 30 new horns babies and from more than 40 new mothers were analysed for the presence of 8 group of chemicals ranging from artificial musk used in cosmetics and cleaning products to flame retardants and chemicals used to make plastics and non-stick and water proof coatings.
The results every single samples of mother or baby blood tested positive for an array of chemicals, many of which are suspected to cause or linked to health problems ranging from birth defects and genetically abnormalities to certain type of cancer. All umbilical cords contained a minimum of 5 of 35 chemicals tested for , some contained as many as 14. Two of the mothers tested had 17 of the 35 chemicals in their blood. Most of the chemical are found in products that we use everyday, cleaning fluids and sprays, tin can lining, perfumes and cosmetics and even baby bottles. Others include banned pesticides like DDT.
For full details of findings were highlighted by Greenpeace Netherlands in a September 2005 report call “A Present for Life”.
In the report, Greenpeace warns that babies are being exposed to these chemicals at the most vulnerable point in their development, and calls for urgent action to be taken to control the production and sale of those chemicals that may damaged the health of both babies and adults.
The report also voices concern over the possible effects of chemicals on children’s brain development and intelligence .
.
My biggest concern about my hospital stay once my baby was born is that the nurses were not allowed to discuss formula feeding with us. (I knew someone that worked on floor and we discussed this later). They instantly put my baby on the breast and even though my baby never latched appropriately, it was assumed everything would be fine once I got home. My baby gained a little weight in the first couple of weeks but by week 7, had only gained 1 lb over birth weight. I am a nurse and I too was scared into believing that formula or bottles would hurt my chances at breast feeding. She is now thriving on formula and gratefully never suffered the consequences of her failure to thrive. Yet everyday, I think about what could have happened. Thank you for this article. There needs to be a kinder approach to feeding choices for new mothers. Hospitals need to talk about formula!!! I dont think any amount of support would have made my breast feeding successful. Im glad I tried but wish I knew to stop much sooner.
Thank you so much for your support and for sharing your story. Every mother needs to know what really happens and that it is not what they say in the books.
Thank you so much for posting this. People need to know. Now I understand why the doctors were so intent on tracking my first twin's glucose and giving him formula on day 1.
I'm so sorry this happened to your child!
I started to respond to your post and lost it, so I hope I don't post twice. Now I'm on a computer instead of my phone, where I can more easily write.
I agree with you that a possible link between jaundice and autism should be investigated. And I agree that we should be sure that babies are feeding adequately before they are discharged from the hospital. Unfortunately, it sounds like your facility/ providers missed some opportunities to catch your baby's problems. It also sounds like they weren't following established guidelines for feeding, discharge, follow up, etc. I have some feedback as an a LDRP RN-BSN, IBCLC on some of your comments, as follows.
"Exclusively breastfed babies are the only patients in the hospital for which we have no information about the quality and quantity of the food they receive."
In my hospital, we follow exclusively breastfed babies more than anyone. All babies feeds are are directly observed at least q12h by staff who have all had at least 20 hours of training specifically on lactation and feeding. Patients generally all get a lactation consult to assess feeding, get individualized feeding education, and have questions answered. Couplets are assessed more often than that to make sure baby is feeding with adequate frequency. Voids and stools are tracked at least q12h; babies who aren't getting enough milk generally do not have adequate output. All of our parents are taught "How to Know Baby is Getting Enough" repeatedly. Our babies are weighed at least q12h (most places probably do q24). Average healthy babies lose around 5-6% of birth weight. One tool that can be used to track normalcy of newborn weight loss is NEWT at http://www.newbornweight.org.
At risk infants have blood sugars tracked for hypoglycemia per AAP guidelines, and all infants have bilirubin levels checked prior to discharge, also in line with AAP guidelines (Coombs +, visibly jaundiced, etc, have labs drawn earlier).
I have never seen a baby in our unit, or readmitted to our peds unit, with a bili of 26, because we practice evidence based feeding guidelines and the above screening guidelines. I don't even think I've seen one over 20 that was born on our unit. (I have seen some in the 20's readmitted from other hospitals where they had poor or no feeding education).
"It has been estimated that as many as 1 in 20 mothers have true milk insufficiency due to breast hypoplasia, post-partum hemorrhage and other factors."
I would like your resource for this, I've don't think I've ever seen this number in 15 years of studying infant feeding , and certainly we don't have this number on our unit. With nonoptimal feeding practices, this/ non evidence-based would be higher of course.
"I also advocate for next day after discharge follow-up with pediatricians with universal bilirubin checks for exclusively breastfed babies, especially before lactogenesis."
Um, we pretty much do this. Universal bilirubin screening is already the AAP recomendation.
Here are some of the AAP guidelines for discharge of healthy, term newborns (the whole paper is linked):
"For newborns discharged less than 48 hours after delivery, an appointment should be made for the infant to be examined by a licensed health care professional, preferably within 48 hours of discharge based on risk factors but no later than 72 hours in most cases.If this cannot be ensured, discharge should be deferred until a mechanism for follow-up evaluation is identified." and "breastfeeding or bottle feeding (the breastfeeding mother and infant should be assessed by trained staff regarding breastfeeding position, latch-on, and adequacy of swallowing); ● the importance and benefits of breastfeeding for both mother and infant; ● appropriate urination and defecation
frequency for the infant;" http://pediatrics.aappublications.org/content/125/2/405.full.pdf
Thank you!
"and most importantly, breasts that are not producing milk when pumped or a child not gaining weight after each feeding."
Any practitioner who knows much about breastfeeding, knows that hardly any mother can pump much in the first couple of days. Colostrum is thick and sticky and usually doesn't work well with a pump like transitional and mature breastmilk does. Some mothers can do it, but I find that mothers almost always do better in the first couple of (colostrum) days with high quality hand expression. Emphasis on "high quality", because poor hand expression often won't work well, either. Simply squeezing the breast or nipple a few times and then assuming that there's nothing there is not the same thing. It can take good instruction, good technique, and a little time for it to work. Very often I observe mothers who don't continue expression long enough or with good technique, for it to start working.
A normal, term, healthy baby generally gets more than pumps or expression. Some moms just don't respond well to pumps. Therefore, pumping offers very little help in determining how much milk a mother actually has. I find that it is one of the most damaging things for a new mom to do (unless she has a risk factor, non latching baby, separated from baby, etc. and needs to express/pump to stimulate supply, of course). I discourage it because they get a pump, get very little and then believe that they have no milk, get very disappointed, and want to quit and it's rarely, if ever, the case if other more reliable parameters such as good feeding assessment, swallowing, good latch, adequate frequency of feeds, good output, and appropriate weights are there.
"I advocate for mothers to be informed of the possibility that their child can become dehydrated, underfed and jaundiced from insufficient breast milk intake."
What place doesn't inform mothers of this??? Again, we are repeatedly teaching how to breastfeed an how to know baby is getting enough during a couplet's stay. And about jaundice specifically, per AAP guidelines.
"Mothers are going home believing that they will uniformly be able to produce enough colostrum for their babies needs and will feed them day and night for weeks if necessary without question if their doctors and lactation consultants are telling them they are getting enough and that they should not give formula."
A practitioner is negligent if they are not assessing feeding, output, and weights properly.No one should be telling their patients that feeding is sufficient if it isn't. Obviously agreed. #1 priority is ALWAYS "feed the baby".
"The current recommendations can be summed up by the words of a lactation consultation who advised a friend's daughter with the following: "Your child will never learn to breastfeed properly if you give her a bottle." This mother went on to feed her daughter day and night for two weeks until a pediatrician intervened when she was found to be underweight. Exhausted and discouraged, this mother stopped breastfeeding altogether. "
NO, current recommendations encompass MUCH MORE than "don't give a bottle"- and anyone who is just saying that without assessing according to ALL THE OTHER GUIDELINES out there, is an idiot.
Although, it is a true recommendation for most babies under 3 or 4 weeks to not use a bottle, before breastfeeding is established. We know this, and when our babies do NEED supplementation, because sometimes they certainly do, we do it with breastmilk, and with alternative methods (usually with SNS type setup at the breast for us, but sometimes finger feeding, cup, spoon, etc.) whenever possible, and formula of course when needed.
"I also advocate for more liberal use of supplementation before lactogenesis and that we scrutinize the science behind the current guidelines of supplementation at a threshold of 7-10% weight loss."
Non-medically indicated supplementation is the single highest determinate of mothers not meeting their breastfeeding goals, which is very damaging to public health. There are so many reasons why this is a bad idea (unless needed as evidenced by excessive weight loss, signs of poor transfer of milk, insufficient output, hypernatremia, etc.). Using formula when it isn't truly needed also changes the gut flora for weeks, and sensitizes babies to cows milk protien, setting them up for allergy. It undermines a woman's confidence.
Again, I'm not against supplementing when needed, but it does not appear that your facility and providers were adhering to established guidelines at all.
Our guidelines and practices (which is what is recommended by AAP, ABM, CDC, etc.) have proven to work quite well – again, we don't HAVE babies with high % weight loss and jaundice like your baby experience because we don't let it get to that point. But I believe that what you are suggesting is way too far in the opposite direction, and would likewise be damaging.
"The daily caloric requirement of a newborn is publicized as 110 kcal/kg/day. Colostrum has been studied as having 60 kcal/100 mL. To meet a one-day-old child's requirement, he must receive 2.8 oz/lb/day of colostrum. A 7 lb child would need 19.6 oz per day or 2.5 oz per feed every 3 hours. Very few women produce this."
Can I see this reference also? 110calories a day may be for the newborn period, but not the first couple of days. Holy cow (no pun intended). That's after they've built up to bigger feedings. Babies fed that much almost all puke it up, because it's too much in the beginning.
Average intake in the first 24h for HEALTHY (not underfed) infants is around 2-10mL per feed. An ounce of (mature) breastmilk is about 22 cal, formula about 20cal. In order for a 3kg baby to get enough according to this, they would have to eat around 16.5 ounces in 24 hours!! Obviously, newborns in the first few days don't eat this much, LOL!!! That would be 8 feeds at over 2 ounces each! These days, we call that a risk factor for obesity later in life. We teach our bottlefeeding moms not to overfeed like that in the first few days.
How would the human race have ever survived if a brand new newborn needed that huge amount of feeding that no woman has… they don't have it because it isn't needed 🙂
Average intake at 24-48h of age is about 5-15mL, 48-72h is 15-30mL, 72-96h is 30-60mL- again, this is based on HEALTHY breastfed infants.
http://www.bfmed.org/Media/Files/Protocols/Protocol%203%20English%20Supplementation.pdf
"We accept a weight loss of 7-10% in the first few days of life based on a 1984 study measuring weight and milk production data of 9 women and have assumed that this is normal, physiologic and advantageous. For every creature on earth, weight loss occurs when the intake of calories and fluid does not meet the minimum metabolic requirement of that organism."
Of course. But newborns
Normal newborn weight loss isn't that hard to figure out… it's pretty easy to see the average weight loss when you work in a newborn unit and see which babies lose what every day. Average healthy, normally fed babies that thrive on my unit lose about 5-6%. They usually peak with their loss on day 3 and regain birth weight by 10-14 days. This is easy to see when you do it every day.
They are going to lose some weight at first because they live in water in the womb and are going to lose some of that water weight, and in addition, at least a couple of studies have found that babies of mothers who get very much IV fluid in labor also are going to be expected to lose even more than the normal amount. A
After this normal adjustment period, loss would be abonormal of course. Again, these days, infant weight gain in the first couple of days is actually considered a risk factor for obestity later on because it is NOT normal.
"1) Daily pre- and post-breastfeeding weights for exclusively breastfeeding mothers. "
Just not needed if other evidence-based guidelines are used. We sometimes do it if there are concerns but really if there is that much concern, we are going to fix the problem and supplement if needed.
After a couple of days, when more milk should be there, we regularly do this at outpatient follow up visits, when it can be more valuable. But when you are talking about 2-10mLs, it's kind of dicey. Other paramenters are more reliable at that stage, take less work, and produce more confidence in moms (again, they are learning "8 or more in 24", appropriate output needed, normal loss amount, etc. – I sometimes show moms http://www.newbornweight.org so they can track it if they want, I think NEWT was based on like 160,000 babies to determine normal weight losses and make the tool).
"2) Thorough counseling on the possibility of underfeeding and jaundice and giving mothers permission to supplement if it appears that their child is hungry and not doing well with next-day follow-up with a pediatrician if such event arises. Such mothers can be advised to pump if necessary."
No mother needs permission to supplement, that is her choice. But if it isn't medically needed, we are not going to recommend that.
Again, any facility that is using normal established guidelines will be doing these things already. We always supplement babies who are underfeeding and they either aren't discharged if feeding poorly, or have next day follow up. I don't know what competent place isn't doing this already???
"3) Uniform daily bilirubin and glucose checks for exclusively breastfed infants before lactogenesis, regardless of physical exam findings."
Again, already established guidelines have been found to be successful in preventing hypoglycemia and hyperbilirubinemia or treating when needed. Truly, it almost always works if all guidelines and evidence-based feeding practices are happening, including immediate and uninterrupted skin to skin at birth (obviously for healthy mothers/babies- just assume that qualifier is on everything I write), which established better feeding from the get-go.
"4) Detailed instructions on the above-described protocol of breastfeeding before bottles until a mother's milk comes in."
Evidence tells us that supplements are not usually needed, and when they are, expressed breastmilk given via alternative methods is the way to go. Again, all this is pretty well established now. Any facilities not using these guidelines need to get with the program, and are setting themselves up for problems. I WOULD expect many more feeding problems from places that are not using established guidelines for breastfeeding, hypoglycemia, and jaundice. If you are looking at facilities that use poor, non evidence-based practices, then you ARE going to see a higher than normal rate of feeding/ weight problems for sure, so if that's the case then your view is going to reflect that. If you haven't observed facilities/ practitioners using evidence-based practice, then I would highly recommend it (AAP, CDC, ILCA, ABM, Baby-Friendly, etc.).
"Daily weighing is insufficient when brain injury occurs within minutes of sustained hypoglycemia."
Evidence has shown that normal, healthy low risk babies that ARE feeding well according to the above paramenters aren't hypoglycemic.
Again, I'm suspecting that the theme here is facilities who don't follow their guidelines, have more poor feeding, and more hypoglycemia as a result. You really aren't going to see that with well-performing facilities.
I'm sorry that you had such a bad experience. It can be very different. You would probably enjoy reading articles in the Journal of Human Lactation, which are naturally always touching on these topics. I hope that as breastfeeding continues to become the norm, reliable information and practices will permeate for the betterment of moms and babies.
I think we need to remember that correlation doesn't equal causation? You advocate for more liberal supplementation and yet if your theory is correct, pre formula wouldn't society have been at HUGE risk of autism? Yet the epidemic is recent so what has changed?
What about the studies that link formula and it's microbiome changing properties with autism? Or epigenetics from 2 or 3 gens of formula feeding (a scientific unknown)? There is so much that hasn't been explored – what about the implications of tongue tie in spectrum conditions? That can also cause inability to transfer colostrum effectively, a time when a baby needs to be highly skilled before volumes increase? It can interfere with the vagus nerve, digestion and is itself linked with genetic mutations like MTHFR which may prevent adequate methylation in the body and increase risks of autism. There are also some studies suggesting certain genetic mutations may pose increased risk with vaccinations etc, did your son have those?
That said I don't think there is any excuse for a dehydrated baby, and the vast majority at 10% are showing signs, in my practice I consider up to 7% typical.
I think in the case of a 15% loss for a paediatrician to give the option of waiting another 24-48 hours is very worrying and renal failure could become a very real concern. A baby with that loss would be lethargic, unable to feed well and has to be rehydrated slowly to prevent seizures! Time and again in practice I see health professionals missing starving babies, the signs are always there from the start, they're just not recognisied until crisis point.
AA
.
Here is article written by an IBCLC saying the rate of failed and delayed lactogenesis are 5 and 15%. Both conditions can lead to pathological jaundice and weight loss if supplementation does not occur.
http://www.medscape.com/viewarticle/565620_4
From the same source:
"Weight loss in excess of 7% may be an indication of inadequate milk transfer or low milk production.34 Although weight loss in the range of 8–10% may be within normal limits, if all else is going well…"
As an IBCLC in a hospital, about 2/10 patients either approach or exceed 10% weight loss by Day 3-4 AND are almost always showing other signs of inadequate intake. It is really scary to discharge them, especially considering that some pediatricians are so "breastfeeding-friendly" that they think it's fine to let an infant go hungry for a few more days waiting for the milk fairy to arrive. This situation is an egregious violation of infants' human rights, and I cannot believe people are so butthurt over Christie's opinions.
Christie, can you provide the full citation? That link doesn't take me to the article.
Lourdes, my pediatrician was irresponsible but I don't blame breastfeeding for newborns returning to the hospital lethargic from breastfeeding. I blame the lactation communities active withholding of information on the incidence of delayed and failed lactation to breastfeeding mothers to keep them from taking matters in their own hands when their children are crying out for milk. There are many mothers on my facebook page whose children were harmed by their lies. You may not have had the same experience but mothers are misled about the risks of exclusively breastfeeding when there is insufficient milk and their children pay for it.
I am curious to hear about your breastfeeding experience that includes how often did baby feed the first 24 hours and how often did you hand express in the first 24 hours. Then after the first 24 hours how how did baby come to breast and did you continue to hand express? How sore were your nipple? How long were they sore? During the nights how often did baby feed? Did he sleep in the same room? What singnaled you to feed baby, such as early feeding cues vs late feeding cues? When latched, describe the suck. How wet were the diapers during the time of dehydration diagnosis? What colour was the urine and stool?
There is so much missing from your article that is extremely important to this important discussion.
My child fed 30 minutes every 3 hours, which I set an alarm for because he did not pipe up for feedings more often than that. Then when he became more hungry, he fed near-continuously. No one asked me to hand express to see how much colostrum I had, of which I had none. My nipples were not sore and the LC said his latch was perfect. Having breastfed him for 20 months, his latch WAS perfect and the suck was strong. Those first nights, he fed near continuously through the night and we roomed-in the entire time. You cannot easily tell how “WET” a wet diaper is with modern day diapers. In fact, no mother or health professional can do that without a scale, which is why diaper counts do not protect newborns from developing excessive weight loss/starvation, which has been shown by breastfeeding research to not correlate with adequate intake. The urine eventually became red. The stool was meconium. We do not diagnose breastfeeding problems until the baby is literally starving. That is what this Foundation is setting out to do by educating mothers to check their milk supply, to listen to their baby’s inconsolable crying and by meeting those signs of starvation with supplemental milk.
My daughter also starved in her first two weeks of life… her urine became orange with some crystal substance. It is the most painful thing to realize that your newborn baby is starving. After 2 weeks of unrest (and intervention from my wise mother), we gave her a bottle of formula and did combination feeding. She then thrived and got to recover by the 4th month. We were lucky that she somehow dodged the more serious complications. She is now 6 years old with an insatiable thirst for milk. Thank you for establishing your foundation. It is so important what you are doing. I fully support you and have experienced first hand the same pain. By the way, the link to your donation page does not work. Hope you can fix that. Hope you would continue this advocacy. It is truly important and life-saving.
Thank you! I just fixed the link! Thank you for considering a donation to our foundation!
Do you really think that those that specialize in lactation education would maliciously withhold information? I am a postpartum RN and a breastfeeding educator. What I have seen are a group of women that want what is best for our babies, if that be exclusive breastfeeding or supplementing. I have to agree with one of the other posts, that there can be extenuating circumstances that keep the baby from transferring milk, (i.e. severe posterior tongue tie).
No, they are not doing it maliciously, but they are withholding information on the risks of newborn starvation to increase exclusive breastfeeding rates. It turns out that is a patient rights violation and can cause irreversible brain injury to a newborn who does not get fed enough. No mother wants her child to experience the torture of starvation and yet they are being taught untrue things like breasts will always provide enough. Only when their babies experience the complications are they told about the risk of brain injury from those complications.
Starvation in newborns is described in this document guiding all lactation consultants from the American Breastfeeding Medicine protocol 22 on newborn jaundice. Why is it that the average breastfeeding momw who reads a breastfeeding manual and takes breastfeeding classes is not aware that newborns starve when it is clearly described in this document available to the public on the internet? STARVATION happens in 10-18% of newborns according to the national organization that guides IBCLC's!
http://www.bfmed.org/Media/Files/Protocols/Protocol%2022%20Jaundice.pdf
Starvation jaundice of the newborn
It is important to recognize that not all breastfed infants will
receive optimal milk intake during the first few days of life; as
many as 10–18% of exclusively breastfed U.S. newborns lose
more than 10% of birth weight.12–14 Absence of caloric intake
in normal adults, even for as brief a period as 24 hours and
with good hydration, results in a small increase in unconjugated
hyperbilirubinemia of about 1–2mg=dL (17–34 mmol=L)
above the adult normal total serum bilirubin concentration of
1.5mg=dL (26 mmol=L).15–17 In newborns, reduced caloric intake
below the optimal intake for age, even without absolute
starvation, results in greater increases in serum unconjugated
bilirubin concentrations because of the normal developmental
limitations in bilirubin metabolism and transport that are
present in the newborn infant.18–20
Two studies21,22 widely quoted in the breastfeeding literature
report that when breastfeeding is optimally managed
there are no differences in serum bilirubin concentrations
in breastfed and formula-fed infants during the first 5 days
of life; however, the majority of reports indicate increased
serum bilirubin concentrations and greater weight loss in
breastfed infants.23,24 Starvation jaundice of the newborn is
more often seen during the first week of life when breastfeeding
is being initiated, but it can occur later in the newborn
period (first 28 days of life) and even into infancy. The
mechanism of starvation jaundice has been shown to be an
increase in intestinal absorption of unconjugated bilirubin.
After the first 5 days of life, starvation further enhances the
normally increased intestinal bilirubin absorption of the
breastfed infant, possibly resulting in toxic bilirubin concentrations.
Interaction of starvation jaundice
and breastmilk jaundice
Poor breastfeeding with inadequate caloric intake during the
first days of life increases intestinal bilirubin absorption because
of relative starvation.17–19 Poor intake also delays emptying
of meconium, a reservoir of considerable unconjugated
bilirubin, and enhances transfer of bilirubin from meconium
into the infant’s circulation.25 This enlarges the circulating bilirubin
pool in the infant, as reflected in higher than normal
serum unconjugated bilirubin concentrations.7 With the appearance
of mature breastmilk at the end of the first week of
life, the factor that enhances intestinal bilirubin absorption will
return greater amounts of bilirubin than normal back into the
infant’s circulation. This results in abnormally increased serum
unconjugated bilirubin concentrations in the second and third
weeks of life, and beyond, which potentially may be toxic.
Attention to optimizing breastfeeding management may mitigate
against the development of late exaggerated serum bilirubin
concentrations in normal infants.17,18
BREASTFEEDING MEDICINE
Volume 5, Number 2, 2010
ª Mary Ann Liebert, Inc.
DOI: 10.1089=bfm.2010.9994
87
I’m not a doctor, just a mom who experienced the pain of seeing my newborn starve. I’m just wondering… it took your baby just a few hours to starve but it took mine 2 weeks. I may have had a little breastmilk coming out of me, but my daughter was also not jaundiced at anytime during her hospital stay. I wonder, does jaundice exacerbate the starvation/dehydration?
It’s the other way around. The less milk a child gets, the worse the jaundice gets. That is why exclusively breastfed newborns are the highest risk of getting severe jaundice.
Starvation in newborns is described in this document guiding all lactation consultants from the American Breastfeeding Medicine protocol 22 on newborn jaundice. Why is it that the average breastfeeding momw who reads a breastfeeding manual and takes breastfeeding classes is not aware that newborns starve when it is clearly described in this document available to the public on the internet? STARVATION happens in 10-18% of newborns according to the national organization that guides IBCLC's!
http://www.bfmed.org/Media/Files/Protocols/Protocol%2022%20Jaundice.pdf
Starvation jaundice of the newborn
It is important to recognize that not all breastfed infants will
receive optimal milk intake during the first few days of life; as
many as 10–18% of exclusively breastfed U.S. newborns lose
more than 10% of birth weight.12–14 Absence of caloric intake
in normal adults, even for as brief a period as 24 hours and
with good hydration, results in a small increase in unconjugated
hyperbilirubinemia of about 1–2mg=dL (17–34 mmol=L)
above the adult normal total serum bilirubin concentration of
1.5mg=dL (26 mmol=L).15–17 In newborns, reduced caloric intake
below the optimal intake for age, even without absolute
starvation, results in greater increases in serum unconjugated
bilirubin concentrations because of the normal developmental
limitations in bilirubin metabolism and transport that are
present in the newborn infant.18–20
Two studies21,22 widely quoted in the breastfeeding literature
report that when breastfeeding is optimally managed
there are no differences in serum bilirubin concentrations
in breastfed and formula-fed infants during the first 5 days
of life; however, the majority of reports indicate increased
serum bilirubin concentrations and greater weight loss in
breastfed infants.23,24 Starvation jaundice of the newborn is
more often seen during the first week of life when breastfeeding
is being initiated, but it can occur later in the newborn
period (first 28 days of life) and even into infancy. The
mechanism of starvation jaundice has been shown to be an
increase in intestinal absorption of unconjugated bilirubin.
After the first 5 days of life, starvation further enhances the
normally increased intestinal bilirubin absorption of the
breastfed infant, possibly resulting in toxic bilirubin concentrations.
Interaction of starvation jaundice
and breastmilk jaundice
Poor breastfeeding with inadequate caloric intake during the
first days of life increases intestinal bilirubin absorption because
of relative starvation.17–19 Poor intake also delays emptying
of meconium, a reservoir of considerable unconjugated
bilirubin, and enhances transfer of bilirubin from meconium
into the infant’s circulation.25 This enlarges the circulating bilirubin
pool in the infant, as reflected in higher than normal
serum unconjugated bilirubin concentrations.7 With the appearance
of mature breastmilk at the end of the first week of
life, the factor that enhances intestinal bilirubin absorption will
return greater amounts of bilirubin than normal back into the
infant’s circulation. This results in abnormally increased serum
unconjugated bilirubin concentrations in the second and third
weeks of life, and beyond, which potentially may be toxic.
Attention to optimizing breastfeeding management may mitigate
against the development of late exaggerated serum bilirubin
concentrations in normal infants.17,18
BREASTFEEDING MEDICINE
Volume 5, Number 2, 2010
ª Mary Ann Liebert, Inc.
DOI: 10.1089=bfm.2010.9994
87
Hello, sorry it took me so long to respond. I really applaud your hospitals higher level of care. I actually took your q12hr practice and added it to my recommendations to the Joint Commission. Weighing is so little effort and yet it is so VITAL for every newborn who is exclusively breastfed. Mothers should in fact be informed of how vital this figure is and should be given the 7% and 10% weight loss threshold calculated at birth so that they may be aware of the threshold when to be concerned and should be advised to weigh their child when they go home if it happens before lactogenesis II and establishment of full feeding. Home baby scales have gotten less expensive and pretty decent at at least detecting the absolute weight of the newborn so that if that newborn goes below the threshold and is in distress as demonstrated by inconsolability, unlatching because little to no milk is present or the baby is not sleeping, a mother can supplement her child at home in the middle of the night and potentially save her child from the harm of pathological weight loss and jaundice.
Glucose levels are undermonitored in my opinion in exclusively breastfed babies because the predominant assumption among laction consultants and physicians is that there MUST be milk present. Therefore babies who are not babies of diabetic mothers or otherwise large for gestational age get NO glucose monitoring, when insufficient feeding absolutely eventually leads to hypoglycemia once the newborn's stores have been exhausted and the milk has not come in to supply their metabolic needs. My newborn developed hypoglycemia by the 4th day (possibly by the 3rd in my clinical estimation) because he was getting nothing.
As for the source of 1 in 20 women having failed lactation and additionally 1 in 7 women having delayed lactation, it comes form this article written by an IBCLC. I have seen that number quoted in other articles on failed lactation as well.
http://www.medscape.com/viewarticle/565620_4
As for next day after discharge follow-up, the guidelines actually say follow up has to be within 48 hours. My child went from 5% quietly losing weight to agitated and at 15% in one day. 48 hours is just too long. I believe at the minimum 24 hours follow up should be universal for exclusively breastfed babies whose mother's milk has not come in. In my estimation, the true time frame a child has to burn through stores is only 2 days if they get nearly nothing from mom. But also, real life does not follow the guidelines. I know moms whose follow-up appointment was 6 days out and this child developed starvation jaundice and is neurologically devasted. Mom was also producing little to no milk the entire time.
Looking at latch and swallow alone is insufficient. At the minimum, a mother's and newborn's milk transfer should be tested before discharge because a patient has the right to know. A professional does not have the right to withhold this information from her and to decide for her what is adequate for her child especially if that information can make her aware that her colostrum may soon not be enough (or that it is not present at all). Latch and swallow does not compare to an actual test weight, which is how we discovered my child was getting nothing. I could have prevented this tragedy with this information had I known it.
Wet and dirty diapers are also incredibly inaccurate for determining true intake because a child can meet all the diaper count requirements from the fluid and stool they are born with. Again, my child got nothing and was able to meet the diaper requirements for at least 3 days, hence the 15% weight loss. Also, the weight of a wet diaper is not defined so 3 wet diapers in one child can be interpreted as 6 wet diapers in another. We are talking about something as critical as preventing starvation in newborn and we are using about the most unproven and inaccurate means to measure it. The most accurate way to detect intake is test weighing, which a mother can do at home as home baby scales are accurate to 2 g (or 2 mL). Even if the baby is moving, a 1/2 ounce can be distingushed from 2 oz by the 3rd day. The guidelines are not enough because if they were, no newborn would ever be admitted for starvation jaundice.
I adjusted this recommendation on pumping based on the feedback of multiple LC's. I actually now recommend manual expression. But some mothers may actually have plenty of milk or even mature milk but their children are not good at getting it so I advocate for moms to try both means so that they may syringe- or spoon-feed their child if necessary. We cannot assume a child is better than a pump or even manual expression because some are not. Making that assumption for something as critical as feeding in the first days is what leads to breastfeeding tragedies like mine. It is our responsibility to make sure they are getting it by any means necessary. I posted a video on manual expression on my Facebook page for this purpose. Unfortunately, mothers are underinformed of the frequency of failed and delayed lactogenesis because of the push to reduce supplementation and promote absolute exclusive breastfeeding. But this exact pressure is what puts newborn lives at risk from pathological jaundice and weight loss. Starvation is far more dangerous than any incremental risk of a few days of limited supplementation and the fact is, some mothers do not produce enough and some newborns do not tolerate waiting for milk before the develop the signs of starvation.
Pretty much not a single mother I have spoken with who received teaching from a breastfeeding manual or lactation consultant were ever told that sometimes colostrum is not enough. Not a single one. You can see people posting on this blog and my facebook page who literally think I am making up the fact that newborns get admitted for not getting enough milk from mom when you as an IBCLC probably see it almost every day. They are told how to count wet diapers and to follow up but they are not told WHY. If this is standard practice, it is not happening in real life because NONE of the moms report on my page that they were told their child could get into trouble from insufficient intake through breastfeeding. It is a frank violation of patient's rights to not be told the risks of exclusive breastfeeding before lactogenesis, which include starvation jaundice, pathological weight loss, hypoglycemia, hypernatremia and brain injury. Every health care provider is required to inform a patient of the risks of any intervention regardless of how rare it is (and this complication is not rare) and any harm that results from the incomplete informing a provider is liable for. Lactation consultants are in dangerous territory because they do not tell mothers that it is possible to not get enough from colostrum alone in order to "reassure" her. Withholding negative information to reassure is coercion and leading her to risks she did not sign up for.
Most importantly, a child can get into trouble at home, in the middle of the night when there may be little access to a provider to give "permission" to feed. Thousands of years have wired mothers to respond to a hungry baby's cry and grandparents are being discounted because mothers are being taught to fear formula when it can save their baby's brain and life. A mother has the capacity to detect pathological weight loss on her own at home and we are putting her child's health at risk by taking away her right to feed her own child who is not getting enough milk. I can count of my hand the number of people I know with milk allergy. Quite frankly, who cares when the other side of that equation is brain-threatening dehydration and hypoglycemia.
I find the diaper count hard to believe due to my son having ‘brick dust’ as described to me as dehydration in less than 24 hours of his birth.
Yes, diaper counts have been shown to have no correlation with sufficient milk intake. Some babies who lose excessive weight of over 10% are able to produce up to 6-8 wet and dirty diapers even on the 4th day.
The current accepted guidelines on normal newborn intake in the first days of life are derived from the observation of what they get from mom who typically produces little in the first days of life. I believe that some children may be born with just enough fluid and fuel stores to get through 2 days of minimal intake and get by. But what my calculations indicate is that they are truly just getting by. They are receiving less than their metabolic requirement and that is why they lose weight. Newborns may in fact lose the 5% which is what my child did quietly. but once they are no longer quiet, I believe they are indicating distress. What is described in the the breastfeeding manuals as 'cluster feeding' or nearly continuous feeding for hours is what I describe as hunger, starvation and distress. That is what my physician- and mother-eyes saw. There is no scientific study that has demonstrated the safety to the newborn brain and long-term cognitive outcomes for newborns who experience 10% of weight loss over 10 days. Not a single study in all of the scientific literature. We started this practice after the 1992 WHO-guidelines were published calling for absolute exclusive breastfeeding from birth through 6 months of age without safety data on newborns. How many babies have fallen through the cracks like my baby since then? Many. It happens every day because a mother is reassured that colostrum is always enough until it isn't. With that, at the minimum, I advocate to daily weighing to be done at home after discharge and for checking for presence of milk through manual expression and pumping. I advocate that a mother have the permission to feed her child like she has had the right to do for millenia and for her to be given the knowledge that sometimes, there is not enough milk and perhaps even no milk.
Looking at latch is insufficient to know a child is getting milk. My child's latch was perfect and he was receiving nothing. A child who gets little to no breastmilk for days even with a good latch due to inadequate milk production will become hypoglycemic. That is a law of physiology. Therefore, a child who goes home after 48 hours and mother's milk has not come in should be checked for hypoglycemia because in fact, he could become hypoglycemic in that time frame if he has run out of his fuel stores. Furthermore, it is vital information to prevent brain injury and practically costs nothing to check. No book or LC provides a mother who wants only the best for her child permission to decide on her own to supplement a newborn if they are crying continuously or feeding without satisfaction when she goes home. In fact, the message she receives is that she could harm her child with formula when the alternative when she is considering it is starvation jaundice and dehydration. There are stories of moms being bullied, insulted and told they aren't good mothers for even considering supplementation when it appears to her that her child is not satisfied. What about the rights of the newborn who's cry is their only means of communicating that the milk they are getting is not enough? As you can see, a term newborn who receives absolutely nothing may have within normal vital signs, bilirubin and weight loss within the 48 hours they are typically kept in the hospital. But after that first 48 hours is where they get into trouble. As for the claims that newborns who get too much in the first days of life is quite not believable. Billions of people walk this earth have been supplemented to 2 oz on the first day of life before the 1992 guidelines and they do not have obesity because of a few ounces of formula. That claim by the lactation community may have been derived statistically but there is no credible mechanism through which that happens that is not confounded by feeding habits obtained from parents and genetics. Normal, healthy low risk babies who are feeding well can be screened with weighing and not be impacted to save the few who develop pathological weight loss. If the guidelines for preventing starvation in newborns were sufficient, admissions for this horrible, preventable disease would stop today. You know as well as I do that is not the case. Sacrificing a few newborns to promote rigid and absolute exclusvie breastfeeding before lactogenesis is unacceptable.
Agree 100%! As an ER nurse practitioner, I've also seen dehydrated and underweight babies that were too weak to even breastfeed properly. Moms are so afraid to supplement as they think that it will "ruin their supply" even though baby needs some calories for energy in order to effectively empty the breast! Very good article: "Feed the baby: when supplementing saves breastfeeding"
http://wendywisner.com/2014/09/02/feed-the-baby-when-supplementing-saves-breastfeeding/
Thank you so much for your support!
Thannk you for sharing your story as im sure it can help many
This is not fear mongering at all; these are facts.
Telling women that just one bottle will harm their babies by putting them at risk for diabetes, cancers, asthma, allergies, obesity, and low IQ without much in the way of evidence IS fear-mongering.
Scare tactics like these(at least I think) is one of the reasons so many babies go hungry and so many new mothers are stressed out.
I agree. Telling new moms things like “You should not give your baby a bottle because she will have nipple confusion”, “You should not pump within the first two months because it will disrupt your milk production”, “You should keep trying, your body will produce milk if you do not give up”.. like what my friend from La Leche League kept telling me IS fear-mongering.
Oh and I was also told, “Your baby has a very tiny stomach—the size of a marble. She will not starve while you wait for your milk to kick in” and “Under no circumstance should you give your baby water because she doesn’t need it” and the most absurb one was, “Did you know that in extreme cases, males have been found to lactate to feed and save a child”.
My birthing hospital is one of the top hospitals in my country. They advocated pure breastfeeding with complete breastfeeding room and lactation coach…new moms needed to get doctor’s permission to give newborn baby formula.
This almost caused my baby her life.
You may find this article interesting. Especially the final bullet point on page 2.
http://www.naba-breastfeeding.org/images/Just%20One%20Bottle.pdf
It should considers mum and baby as a unit and is much more than treating symptoms. breast pump
Hi, I am from Kerala, a state in South India. Both my kids developed jaundice after birth, but the pediatrician and my gynaec identified tbe problem immediately, they encouraged me to supplement with formula until I had enough milk supply. The best part is that they assured me that supplementing fora few days after birth would not have an adverse impact on breastfeeding. My second child , had to be supplemented with formula and expressed milk for the first ten days. I dont understand how the healthcare professionals in an advanced country can allow an infant to starve! Why didnt you ,a physician, follow your own instincts, when your infant was restless even after being fed!
"He was nursed on demand for 20-30 minutes every 3 hours."
There's your problem. Every hour, at least, for the first few days.
The fact that your infant was eating only once every three hours should have alerted you to a problem. You claim to have read all the guidelines on breastfeeding your child, but you somehow missed the very important detail that though bottle-fed infants eat only once every 3-4 hours, a breastfed infant eats once every 1.5 to 2 hours. If your breastfeeding child was breastfeeding only once every three hours, it is not at all a wonder that he was starving. I am sorry no one ever informed you of this very important detail of breastfeeding.
14-6-16
Thank you so much for sharing your personal story and insights out of it! I empathize with what you went and still go through. Of cource, nobody knows what was the real cause of your baby’s autism, anyway you brought to the surface a really serious issue that nearly all of us who work with breasfeeding mothers have experienced, at least once. In my practice, i have seen enough underfed breastfeeding babies, some of the cases serious. I also feel there a vagueness in guidelines concerning safe feeding of babies, or, to put it otherwise, a vagueness in interpreting and applying existing guidelines. I find your propositions concerning monitoring of neonates' feeding very interesting and a good base for debate and revision or for more accurate formulation of guidelines.
I personally stick to the following priorities concerning that topic, in the sequence that follows: 1. FEED THE BABY, 2. feed the baby with mother's milk or donor milk, 3. breastfeed. It has saved me from quite some dangerous situations of seriously underfed weakened babies, in spite of the fact this has dissatisfied some mothers passionate for breastfeeding. At the end of the day, at least for me, above all guidelines, i let intuition guide me when encountering a situation that feels awkward to me despite being “ok” according to guidelines. Let us be reminded that guidelines follow facts, studies and observation, are made to be revised, and -last but not least- are made by humans.
We have to keep in mind that, “breast is best”, and support breastfeeding in a SAFE frame – which is the best means of promoting it. That can be done when we -as health professionals- keep a clear mind –free of emotional approaches to the subject, and put “FEED THE BABY” as the cornerstone to our practice.
Thank you again for sharing, and for the opportunity you gave us of exchanging views on such an important subject. The very best to you and your family!
I had a similar situation to yours. One difference was that I received zero post-delivery lactation support and a pediatrician who discharged my son with an 11% weight loss and who still jaundice. I was told this was fine and to maybe start supplementing with formula and was sent home with 8 oz of formula. I live in the Washington DC area where we are thought to be educated and have excellent hospitals. I went to all the baby education classes. I knew my son was not well but all the experts said he was ok. Within 12 hours he was being transported (without me) to a children's hospital and subjected to multiple test to rule out bacterial infections. That hospital provided me with the support I should have gotten but it was too late for my milk production. 15 months later and I still feel like it was my fault and I should have known better. Thank you for sharing, time will tell if my son will have an negative effects but today he is in the 97th percentile in weight and height!
While I appreciate your information, blogs like these do tend to cause fear in moms and discourage breastfeeding. There is no link between autism, jaundice, and breastfeeding. My son had severe jaundice and was rushed to the NICU because the hospital was negligent and sent us home with a level of 9. He had 4 of the 5 signs of severe jaundice. (I found this out later, after getting better care at the NICU) He was nursing and eating. All I hear these days is, "I can't make enough milk." "I am not producing." Only 2% of all women can't produce enough milk. 98% of women CAN. They just don't want to put in the work and time in those first few months. I had to feed both my little ones every 1.5 hours to establish a good milk supply. Once every 3 hours is not enough and your body won't boost your supply. If supplies are truly low, there are many ways to effectively boost it. Breastfeeding is hard and takes a lot of work in the first month. Too many women give up after a week or two. Please, don't create unnecessary fear in women. This is why people don't breastfeed.
I realize that this is probably your experience, but your comments make me sad. I did not produce enough milk with my baby but didn’t know it until I took her to the doctor and found out she was mildly dehydrated. I then went to my OB and he put me on Reglan which sometimes helps with milk supply. It didn’t help. I also hired a lactation consultant that came to my house daily for weeks. From day 1 I fed my baby on demand which ended up being every hour and a half. I know your comments obviously don’t pertain to me and I’m sure there are lazy mom’s out there that don’t put out the effort. I just get bummed out when women are made out to be bad mom’s when they use formula. Can we just agree that feeding our babies should be #1 even over breastfeeding? I think breastfeeding is best as long as there’s milk and it’s healthy but that isn’t always the case unfortunately.
We absolutely agree. Feeding out babies should be number 1, 2 and 3. No mother should be shamed and no baby should ever go hungry.
You know, making a statement like “they just don’t want to put in the work and time” is equivalent to people who make the claim that abortions shouldn’t be readily available because then women will use them as a form of birth control. Both are absurd, and insulting to women. I know NO ONE, that is ZERO women who intended to breastfeed their babies who simply gave up because it was too hard. Most women, including myself, keep trying past the point of realizing nothing’s actually going to make it happen, and then carry a sense of personal failure about it ever after.
Where does your statistic that “only 2% of all women can’t produce enough milk” come from? Because that is the kind of bullshit that only contributes to this stupid, stubborn insistence on breastfeeding at all costs, and makes women like myself who tried EVERYTHING feel like they have ZERO support from not only their fellow moms, but the lactation consultants, midwives and everyone else who chimes in with their unhelpful two cents.
What I do know is that neonatal jaundice and dehydration can cause cerebral palsy if left untreated, but not a single medical professional I came across ever mentioned that. If that’s the risk that lactivists want to take, let them do it with their own children. Not mine.
What I’d like to see is all of these sanctimonious breastfeeders to stop judging moms who simply—and it doesn’t actually matter what the reasons are, because it’s none of your judgemental, bitchy business—make the choice to formula feed. How about we stop making the issue of feeding our babies into some kind of stupid “I’m a better mom than you” contest? How about we push for better formula, for better access to breastfeeding help, for better options for women, no matter the choices required?
I highly recommend you read “Lactivism” by Courtney Jung, if you need the other, reasoned, science-based side of the issue.
My milk didn't come in with my oldest son, and he got very dehydrated and his bilirubin was spiking. We took him home, but then took him back to the hospital for 5 days. Truly, it was touch and go. It took an hour for them to find a vein so they could rehyrdrate him. He's fine now, 13 years old.
I wish I had known what you're sharing here. I shared the same thing with people I knew who were expecting around the same time as me because I didn't want what happened to my baby (I literally nearly killed him with my ignorance) to happen to others. It didn't feel like fear mongering then.
I still breastfed both my kids. I was afraid because of what I'd experienced, but it didn't put me off breastfeeding. My second one took formula in the hospital, though it probably wasn't necessary. I certainly wasn't going to let the same thing happen twice.
I guess allowing people to know more than just one side and what to look for while breath feeding the first few days of life is "fear mongering". We get it..you like breast feeding and nothing but breast feeding and it couldn't possibly have any negative side effects.. Luckily your much smarter than this pediatric dr and scientist is. Funny how not once did she say NOT to breast feed..or say it was bad..just that some mothers don't produce enough milk or any milk the first week of life and to watch carefully for signs that come along with it in your baby..another lactation nazi who can't understand anything than what they want to understand. Any word to the contrary equals "fear mongering". Uhg. This is why I seriously hate so many people. Life,education,relationships and even breast feeding are not all one sided. You clearly haven't had any problems breast feeding like I myself did or countless other mothers. Fortunately even at the young age of 18 when I had my first child I new something was wrong with him crying like he was,When I called my doctor they told me he would be fine and could go days off "brown fat" alone and just keep going.. Needless to say he was bottle fed from then on as were my other two children later on. I'm all for breast feeding but not all of us are equipt to do so. It's a shame that when some one offers extra knowledge and resources how easily you can tear it apart and call it nothing more than a mass hysteria ploy by using the words.."fear mongering ". I'm sure you're a real peach to talk to in real life. You seem so u derstandable and open minded.
Thank you for saying this. I’m with you
YES!!! Not to mention was the baby evaluated (properly) for lip and tongue ties? Most doctors are NOT informed about these and they are often misdiagnosed or undiagnosed. Especially hidden posterior tongue ties that are not visible until properly checked for with a specific tool. This would explain a lot because ties prevent babies from effectively transferring milk. And everyone knows that the amount of milk you can pump is NOT an indication of your milk supply. There are soooo many things wrong with this article and completely fear mongering in many of it's wording. Ugh.
Thank you so much for sharing this article. More new mothers need to be reassured that they are not "bad moms" if they find their baby needs supplementation until they can produce enough milk on their own. When I had my son, I had read multiple books on breastfeeding, and thought I was very well prepared. However, as you have observed, everything I read discouraged any type of supplementation in the early days of breastfeeding. When my 9 lb son was born, he was healthy and had a voracious appetite. The lactation specialist said his latch was good. However, although I nursed him frequently, he cried constantly and kept dropping the latch. The specialist thought perhaps his stomach was upset, so they had his tummy pumped and found nothing unusual. I kept trying to feed him, and he kept crying in frustration. Meanwhile, he was becoming increasingly jaundiced (to the point that we were prescribed a bili blanket the day after we left the hospital). Finally, as we were packing up to leave, the nurse hesitantly suggested supplementing with formula using a syringe while he nursed. Suddenly he was nursing with vigor and much more content. I wish she had said something earlier. He lost 11% of his body weight in the first 48 hours, although they didn't seem to monitor that in the hospital. The only reason we found out is that we went to the doctor to have his bilirubin checked the day after we checked out of the hospital. The doctor suggested that we continue to supplement until he regained weight and was no longer jaundiced. While I felt disappointed that breastfeeding had not gone according to plan, and frustrated that nothing I had read had prepared me for this type of situation, I was particularly horrified by the idea that my child had essentially been starving during his first day & night of life. While breastfeeding is of course the best way to go, women should be aware that if they have to supplement during the early days, it will not "ruin" their child's breastfeeding future, particularly if they do it with a syringe while simultaneously nursing. (I know others who did this, along with pumping, and were able to get their supply up within a few days.) Additionally, women who have more serious long-term problems with their milk supply meeting the baby's needs should not feel like failures or be judged by others because they are not "exclusively" breastfeeding. My son has consistently been in the 98th percentile for all size categories, and I was never able to get my breastmilk supply up to what he needed, in spite of speaking with a lactation specialist and doing a LOT of pumping, which was discouraging for me (I did feel like a failure), but I gave him as much as I could, and he thrived with the formula supplementation (I switched to a bottle for formula rather than a syringe as he got a little older). I'm grateful to the nurse for showing me how to use the syringe so that I could simultaneously breastfeed and supplement. It helped me make the psychological leap from all the warnings and finger-shakings I had read about the "dangers" of supplementation to actually doing what was best for my baby under the circumstances. Every situation is unique, and breastmilk is the best food for baby (when it can be provided), but I didn't have enough to meet his needs and this was the best solution to our situation. I only wish I hadn't been so scared to try it based on inaccurate information that I had read (that he would have an allergic reaction, that he would reject the breast, that I would never be able to breastfeed, etc.), none of which turned out to be true in this case. I have a relative whose child did seem to be allergic to regular formula, so she purchased breastmilk or used special formula as an alternative. NOTHING I read warned me of the possible dangers of my baby not getting enough to eat in the early days, and I think more research and education should be provided for that.
"The learned wisdom of grandparents who know instinctively the sound of a hungry baby is being supplanted by breastfeeding manuals that cannot teach that sound to the new parent." This was most definitely not my experience. As a new mother I had immediate instincts to feed and love my baby when he cried. I was condemned by family, including many grandparents, saying that I was "spoiling" him by responding as soon as he cried and that I was going to turn him into a "hip baby". Being a mother, especially a first time mom, is hard. Everyone has strong opinions on how we should raise our kids, and a lot of the information being passed down to our generation is outdated. My mother insisted that the reason my baby wasn't sleeping all the way through the night was because we were not loading up a bottle with rice cereal and giving it to him before bed to fill up his stomach. This is just one example. I agree that in some facilities, the push for exclusive breastfeeding regardless of whether the mother is producing sufficient milk can cause harm to a newborn. But, on the other side of this spectrum are the facilities and practitioners who have very limited knowledge of breastfeeding and simply hand out cans of formula even when the mother intends to nurse the baby. Not receiving appropriate medical information causes new parents to turn to the internet and to family, who may be well meaning but lack current evidence based information. The "mommy wars" are not helping this issue either. Unfortunately, many new moms think they have to be in one camp or the other: either a "lactivist" or a formula feeder. It doesn't have to be that way!
Dear Dr. Castillo-Hegyi, Yours is a lonely voice, but please keep speaking out. By God's grace, I was able to listen to each of my four newborns cry, and instinctively know they were hungry. I supplemented despite the condemnation of my own husband, his family, my friends, and the powerful La Leche League, who seemed to feel that every woman is capable of producing sufficient milk. My children are grown now, and looking back as I read your article, I feel I narrowly dodged a bullet. Keep telling the truth. You deserve a Nobel Prize.
Hi Dr. Castillo-Hegyi, i would love to suggest you research on Tahneek, a practice which is by rubbing the palate of newborns with a date (fruit) that can prevent babies against brain damage, whether this practice could be another solution to formula feeding upon birth.
I have done some reading on common birth practices, and I was very interested to find this article. One thing it discusses is how pumping mothers in labor full of IV fluids can lead to breast edema and delayed milk production. I'm not saying this is every case, but it's worth reading. This is another danger of potentially over-medicalizing a normal process. http://evidencebasedbirth.com/are-iv-fluids-necessary-during-labor/
I’ve also read that a C-section with all the anaesthesia you are given has devastating effects on milk production, not to mention all the stress you suffer at the hospital, especially if you tried for hours (including the dreadful synthetic oxytocin you are given when the contractions are not good enough) to have a normal birth and couldn’t. 🙁
I got all of that. The nurses in charge when my baby wouldn’t latch didn’t bother… just gave me a bottle (no syringe, which might have saved my breastfeeding efforts). Arriving home, I bought a breastpump and thus began my adventure. I expressed milk, first with a pump, and later when I learned how to, with my hands, but I could never achieve exclusive mother milk feeding (at best, I could cover 50% of his milk requirements). I could never get my baby to latch, unfortunately. My boy learned in hospital that bottle was best, and never wanted the breast. 🙁
Now reading this, I have to say in spite of the guilt you are induced to feel, the insecurity of being a mother who tried to breastfeed and failed, I feel blessed to have a normal, very healthy 7-year-old.
OH my goodness, your first two paragraphs were so hard to read. I felt sick and started to cry as I was instantly transported back to the first week of my first child's life. It was hellish. My introduction to being a mother was a week of my baby screaming. I was so determined to do the right thing for my baby, to exclusively breastfeed, and to not hurt my supply by supplementing at all. After a week of torture, daily trips to the hospital to check his bilirubin count as it just went up and up, and both of us crying day and night, I borrowed a pump and saw that I was producing barely anything. So I said, "Screw it. Breast is best, but starvation is worst." I got out one of those sample bottles of formula from the hospital, and my baby, who hadn't latched and sucked for longer than 5 seconds at a time, CHUGGED an entire 2 ounces…and fell asleep contently! After that, I was able to buy my own pump, and I continued to pump and bottle feed my baby, while supplementing with a bottle of formula once or twice a day. My son is a healthy boy, but the trauma from this experience is something I would never wish upon any new mom. With my next two babies, I breastfed and supplemented from the get-go. They didn't get jaundiced, I felt relaxed and not worried, and there was much less bawling. I actually enjoyed the time with my newborns! It still makes me just sick that I was basically starving my child because of the extreme information I was taught in breast-feeding classes. Thank you for speaking out in a society which basically thinks you are a child-abuser if you don't exclusively breastfeed. There are so many mothers who struggle with milk supply and whose babies suffer because of it!
Thank you so much for your support.
Because the books make you fear formula and hide the possibility and the risks of starvation your child. I am glad you had a wise pediatrician. Millions of health professionals are being taught to avoid supplementation at all costs and not tell mothers a baby can be hospitalized and brain injured by starvation from exclusive breastfeeding.
He nursed continuously for 2 days straight.
1 in 10 baby is hospitalized by a Baby-Friendly hospital system. This is not just my baby. There is nothing I did that made my baby starve except listen to lactation consultants who lie about how often a mother does not have enough milk to keep her baby from starving.
I'm so sorry that happened to you. Mothers should all be taught about the realities of exclusive breastfeeding before they even go into the hospital. Babies should not suffer the consequences of mothers not being given all the information they need to know.
There are links to jaundice and autism. The most common cause of severe jaundice is now starvation jaundice from insufficient early breastfeeding and severe jaundice is associated with a 22-fold risk of autism. 22% of mothers have delayed-lactogenesis II from a study of motivated, lactation supported mothers which caused their babies to lose excessive weight. There is absolutely no published epidemiological study that supports that 2% can't produce milk. That is fiction from breastfeeding books who have a financial incentive for publishing that kind of mythology.
Thank you Christine for your support. Keep sharing with your friends and family. My son's story happens every single day.
I am so sorry Amy. It is criminal that this is hidden from mothers. It happens every single day. If you haven't signed the petition, please do so and leave a comment. Mother's need to know. https://www.change.org/p/center-for-disease-control-vivek-murthy-surgeon-general-american-academy-of-pediatrics-petition-to-warn-parents-regarding-brain-injury-caused-by-insufficient-breast-milk-intake
Thank you so much for that article based on science. My baby was found with hypoglycemia at birth. We stayed at the nursery for many days, breastfeeding and trying to get over this. After 5 days, we (parents) asked if giving supplement would help. Only then the nurses and doctor said yes. After that, I gave supplement while breastfeeding for weeks (pumping also each time). I finally succeed in breastfeeding and I still do after 18 months. For months, I had feel so bad thinking I hadn't done the right thing for my baby, reading stuff like no mother cannot breastfeed or that giving bottles will end my breastfeeding. Thank you for confirming I had done what was right for my baby. Go on speaking up loud!