Dear Colleague and Parent:
My name is Christie del Castillo-Hegyi and I am an emergency physician, former NIH scientist, with a background in newborn brain injury research at Brown University, and mother to a 6-year-old child who is neurologically disabled. I am writing to you because my child fell victim to newborn jaundice, hypoglycemia and severe dehydration due to insufficient milk intake from exclusive breastfeeding in the first days of life. As an expectant mom, I read all the guidelines on breastfeeding my first-born child. Unfortunately, following the guidelines and our pediatrician’s advice resulted in my child going 4 days with absolutely no milk intake requiring ICU care. He was subsequently diagnosed with multiple neurodevelopmental disabilities. Being a physician and scientist, I sought out peer-reviewed journals to explain why this happened. I found that there is ample evidence showing the links between neonatal jaundice, dehydration, hypoglycemia, and developmental disabilities. I wish to explain to you how I believe this could apply to my son and the many children whose care you are entrusted with.
I was an attending physician in the hospital where my son was born at Downtown Presbyterian Hospital in Albuquerque, New Mexico. My son was born 8 pounds and 11 ounces after a healthy pregnancy and normal uneventful vaginal delivery. He was placed directly on my chest and was nursed immediately. He was nursed on demand for 20-30 minutes every 3 hours. Each day of our stay in the hospital, he was seen by the pediatrician as well as the lactation consultant who noted that he had a perfect latch. He produced the expected number of wet and dirty diapers. He was noted to be jaundiced by the second day of life and had a transcutaneous bilirubin of 8.9. We were discharged at 48 hours at 5% weight loss with next-day follow-up. We were told by the lactation consultant before discharge that he would be hungry and we were instructed to just keep putting him on the breast. Upon getting home, he became fussy and I nursed him longer and longer into the night. He cried even after nursing and latched back on immediately. He did not sleep. By the next morning, he stopped crying and was quiet. We saw our pediatrician at around 68 hours of life (end of day 3). Despite producing the expected number of wet and dirty diapers, he had lost 1 pound 5 ounces, about 15% of his birth weight. At the time, we were not aware of and were not told the percentage lost, and having been up all night long trying to feed a hungry baby, we were too exhausted to figure out that this was an incredible amount of weight loss. He was jaundiced but no bilirubin was checked. Our pediatrician told us that we had the option of either feeding formula or waiting for my milk to come in at day 4 or 5 of life. Wanting badly to succeed in breastfeeding him, we went another day unsuccessfully breastfeeding and went to a lactation consultant the next day who weighed his feeding and discovered that he was getting absolutely no milk. When I pumped and manually expressed, I realized I produced nothing. I imagined the four days of torture he experienced and how 2 days of near-continuous breastfeeding encouraged by breastfeeding manuals was a sign of this. We fed him formula after that visit and he finally fell asleep. Three hours later, we found him unresponsive. We squeezed a few milliliters of formula milk into his mouth, which made him more alert, but then he seized. We rushed him to the emergency room. He had a barely normal glucose (50 mg/dL), a severe form of dehydration called hypernatremia (157 mEq/L), and severe jaundice (bilirubin 24 mg/dL). We were reassured that he would be fine, but having done newborn brain injury research, knowing how little time it takes for brain cells to die due to hypoglycemia and severe dehydration, I did not believe it, although I hoped it.

Born healthy, full-term weighing 8 pounds 11 ounces getting skin-to-skin and immediate breastfeeding after birth

The third day of life after the pediatrician visit. He was no longer crying and he was jaundiced and dehydrated with 15% weight loss. We were reassured that we could keep exclusively breastfeeding.

Hypernatremic dehydration and encephalopathy from brain injury. Blank staring is a hallmark of newborn brain injury.
Watch the Doctors Show Interview
At 3 years and 8 months, our son was diagnosed with severe language impairment, autism, ADHD, sensory processing disorder, low IQ, fine and gross motor delays. He was later diagnosed with a seizure disorder associated with injury to the language area of the brain. Since my child’s diagnosis, I have been researching the scientific literature on breastfeeding insufficiency, newborn starvation, brain injury, and developmental disabilities for over three years. In addition, I have collected similar breastfeeding stories of tens of thousands of women through social media.
In the September 2015 issue of Hospital Pediatrics, an article was published describing 11 exclusively breastfed newborn babies who developed profound hypoglycemia between the second and fifth days of life from insufficient breast milk intake. The child described in the body of the article was a healthy full-term baby who presented just like my son. He was seen on the third day of life at his pediatrician’s office. Despite that, he was found on the fourth day of life lethargic and unable to feed. He had lost 10% of his birth weight and had a low glucose of 20 mg/dL (normal > 47 mg/dL). This child was given IV glucose after which he developed a seizure. They obtained a brain MRI which showed extensive areas of injury to almost the entire brain. In addition to this child, 10 other healthy term newborns were identified to have developed hypoglycemia from insufficient breastfeeding as well. They were found lethargic, seizing, hypothermic and/or not breathing. 5 out of the 6 MRIs obtained in these babies showed widespread injury to a third to almost the entire brain in varying patterns. They subsequently developed long-term neurological disabilities including seizure disorders, motor weakness, visual impairment and feeding difficulties requiring speech therapy.
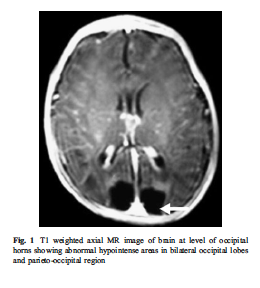
The brain MRI of an exclusively breastfed baby who developed lethargy and hypoglycemia (20 mg/dL) by day 3 of life from insufficient breast milk intake. The dark areas in the posterior part of the brain are the areas of missing brain tissue that resulted one month after the episode of hypoglycemia.
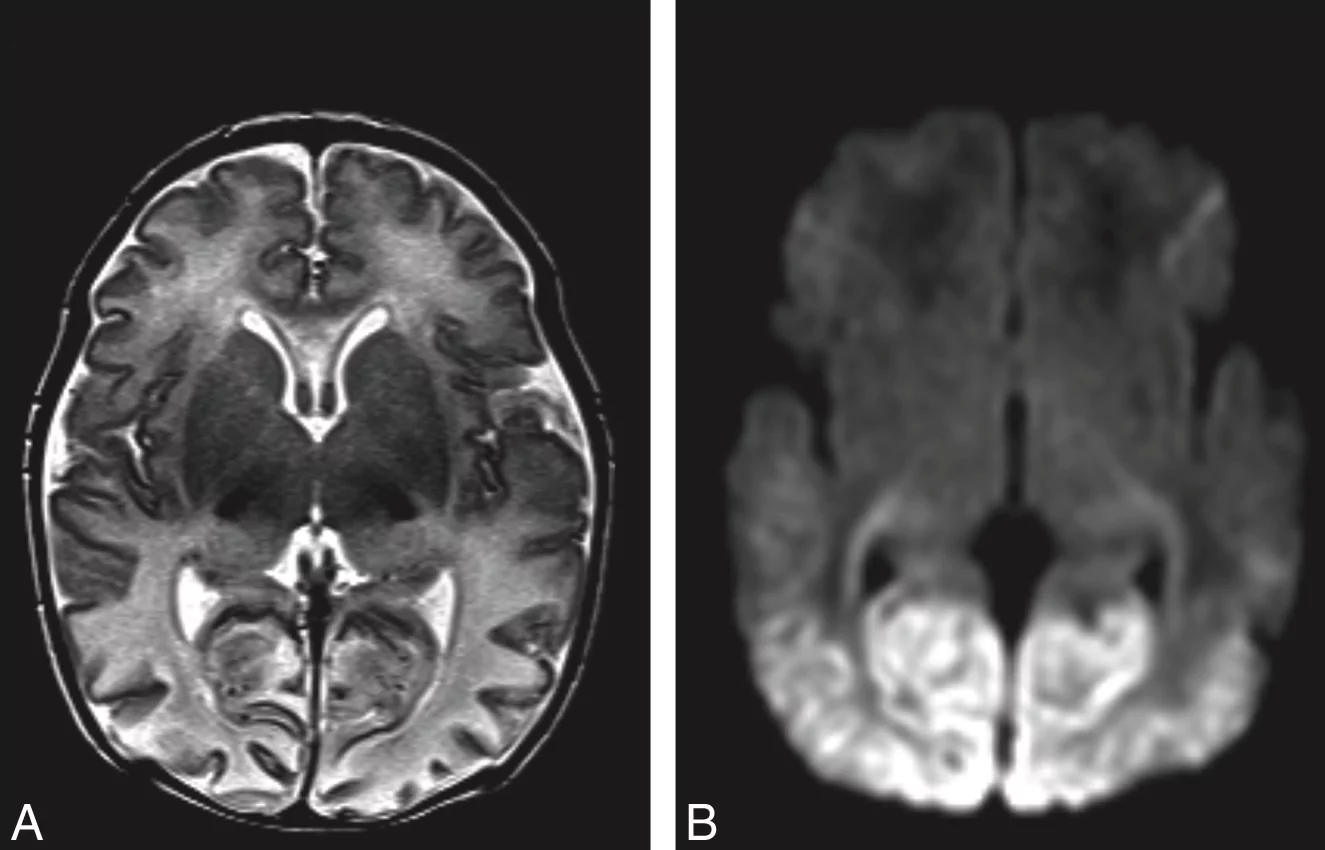
Brain MRI of acute hypoglycemic brain injury. The light appearance in the posterior part of the brain is swelling and injury caused by caloric deprivation to brain cells due to hypoglycemia.
The answer to the epidemic of developmental disabilities we are seeing may be found in this vulnerable period. The risk factors for neurological disabilities in children all have to do with brain injury caused by excessive jaundice, loss of oxygen, circulation, and glucose delivery to the brain. These include pre-eclampsia, intrauterine growth retardation, and prematurity, which are caused by poor function of the placenta and decreased circulation to the baby. Hypoglycemia, umbilical cord prolapse, nuchal cord (cord wrapped around the neck), fetal distress, low Apgar scores, respiratory distress, and other labor complications, events that all cause perinatal brain injury also cause long-term neurological disabilities. Although there are many causes of newborn brain injury that we have no control over, we have control over whether or not a child is fed enough for all their brain cells to survive. I believe we may be inducing hypoglycemic brain injury to many newborns by asking mothers who may not be producing sufficient milk for their newborn’s physiologic need to exclusively breastfeed. We are potentially putting ourselves at odds with the protective natural instinct to respond to a baby’s cry by telling mothers that their colostrum is enough (which for many it may not be) and by making them fear failure by giving their child supplementation when they need it.
My child’s story is not rare. In a study of 280 mother-baby dyads, 22% of motivated mothers intending to exclusively breastfeed who received close lactation support experienced delayed onset of copious milk production, or lactogenesis II, which put her child at 7-fold increased risk of excessive weight loss greater than 10%. This means more than 1 in 5 newborns are at risk of excessive weight loss and the associated complications if exclusively breastfed from birth. In another study, it has been found that 10% of well-monitored exclusively breastfed babies undergoing the Baby-Friendly Hospital Initiative protocol develop hypoglycemia of less than 40 mg/dL within the first 48 hours. This incidence was even higher in babies born to first-time mothers as 23% developed hypoglycemia. This level of hypoglycemia has been shown in other studies to result in brain injury on MRI and long-term declines in cognitive function. One study showed that a glucose of less than 46 mg/dL within the first 24 hours of life was associated with a 3.7-fold increased risk of brain injury on MRI and a 4.8-fold increased odds of lower motor, cognitive and language scores at 1 year of age. This cognitive impairment persists as evidenced by another study of 1395 newborns showing that newborns who develop transient hypoglycemia of less than 40 mg/dL had a 50% reduction in passing their fourth-grade proficiency test in literacy and math. Even glucose less than 45 mg/dL resulted in a 38% reduction in passing the literacy test. The current standard of care tolerates a glucose between 25 and 45 mg/dL when there is evidence that those levels of hypoglycemia result in long-term lower academic achievement and developmental disability.
I hope you feel the same sense of urgency that I do. Since we received our diagnosis, I have come to personally know 43 mothers whose children experience starvation-related complications from exclusive breastfeeding, including pediatricians, other doctors, nurses and lactation consultants. All of them have children with long-term neurodevelopmental impairments. While the literature cites poor education in breastfeeding as the cause of these starvation-related complications, in my research of breastfeeding mothers, it is the most educated in breastfeeding that are at the highest risk. The least educated will respond to a baby’s cry by offering a bottle. The mothers that are most educated in breastfeeding are the ones who have been taught that offering just one bottle will ruin her breastfeeding and potentially harm her child. I have learned that this is a distortion of reality created by breastfeeding education to pressure mothers to exclusively breastfeed that can put her child’s life at risk.
I am writing to let you know I believe the current newborn exclusive breastfeeding guidelines of the Baby-Friendly Hospital Initiative are dangerous. My son suffered an incredible amount of weight loss by the third day, which is often when mothers produce milk. How many newborns are experiencing this same fate? To date, there are no rigorously done studies on the safety of newborn weight loss and exclusive breastfeeding before lactogenesis II on the newborn brain. In fact, a study has shown that exclusive breastfeeding at discharge is associated with an 11-fold higher risk of rehospitalization for underfeeding and dehydration, which few parents are informed of.
I would like to advocate for a patient safety initiative to increase monitoring and supplementation to prevent adverse neurologic conditions in all exclusively breastfed newborns as described by the following:
1) Mothers should be instructed on how to manually express to confirm the presence of milk, which is available through this link. Any baby whose mother has little to no colostrum should be offered supplementation immediately.
2) Twice daily weighing for exclusively breastfed newborns in the hospital and at home as it has been shown that the least-fed newborns can lose the maximum recommended weight loss of 7% within the first 24 hours. This practice should be continued at home until breastfeeding meets the child’s full metabolic requirement as signaled by the onset of daily weight gain. The 7% weight loss threshold should be provided to the mother to help signal the need for supplementation in the hospital and at home.
3) Universal daily transcutaneous bilirubin checks and glucose monitoring while in the hospital for exclusively breastfed newborns before the onset of daily weight gain as the scientific literature has now identified them as a high-risk population for hypoglycemia. The physical exam is insufficient to rule out hypoglycemia and pathological hyperbilirubinemia. Any inconsolable child should also have a glucose check as this is an often-missed sign of hypoglycemia. Supplementation with breast milk or formula as well as IV glucose should be given immediately at a glucose level less than 47 mg/dL as this is the only prospectively validated glucose threshold that if corrected immediately prevents the development of developmental delay. Supplementation should also be offered for bilirubin levels exceeding 15 mg/dL or any level considered high risk on the bilirubin nomogram. Not only does supplementation for underfed newborns protect a child’s brain and stabilize glucose but it also doubles the rates of exclusive breastfeeding at 3 months.
4) Pre- and post-breastfeeding weights after lactogenesis II to measure the amount of milk transferred to the baby. The caloric requirement of a newborn baby is 100-120 kcal/kg/day and a mother’s production should be around 2.7 oz/lb/day or 6 oz/kg/day (roughly 2 ounces per feed every 3 hours) to sustain a newborn and prevent feeding complications. Some babies with medical conditions may need more than the above volumes.
5) Next day after discharge follow-up with pediatricians and lactation consultants with universal bilirubin and glucose checks in the office. Children who are crying inconsolably at home especially before lactogenesis II should be supplemented after nursing UNTIL they reach their health care provider in order to prevent the development of hypoglycemia, dehydration and negative neurological consequences.
6) I advocate for mothers to be informed of the possibility that her child can become dehydrated, jaundiced, and hypoglycemic from insufficient breast milk intake and that these conditions can cause developmental and neurological disabilities. Signs of this are a child that is not sleeping or crying repeatedly after breastfeeding as well as nursing near-continuously. Lethargy, poor feeding, seizures, hypothermia (low body temperature), and bradycardia (slow heart rate) are late signs that suggest the presence of profound brain injury from near-complete glucose deprivation to the brain. Lethargic hypoglycemic babies deserve a brain MRI to provide vital information to parents so that they can closely monitor their development and obtain early intervention as needed.
7) Every mother should be educated on supplementation after nursing in order to continue the stimulation needed to promote milk production in case the need for supplementation arises, particularly before discharge if lactogenesis II has not occurred. If a child is hypoglycemic, greater than 7% below the birth weight, hyperbilirubinemia, hypernatremic or crying inconsolably out of hunger, supplementation can be offered 15 MLS at a time as the newborn stomach has been in fact measured to be 20 mL in size at birth, much larger than commonly taught to mothers and health professionals. Supplementation should be offered until a child’s laboratory markers are corrected and the child is no longer in distress. A child’s brain will not wait for food. Once the child is adequately fed, the breastfeeding may then be evaluated to identify the cause of underfeeding. Supplemented breastfeeding is a valid choice as NO BENEFIT of exclusive breastfeeding justifies the risk of life-long disability caused by hypoglycemic brain injury. Any mother sent home before full milk production without a supplementation plan is being sent home to potentially starve and disable her child if her milk does not arrive on time.
Mothers are taught by breastfeeding manuals that they will uniformly be able to produce enough milk for their baby’s needs and will feed them near-continuously for weeks without question if their doctors and lactation consultants tell them not to give formula. But as you have witnessed as a matter of routine, breastfeeding jaundice is very common and mothers do not uniformly produce enough milk for their babies’ needs. The learned wisdom of grandparents who know instinctively the sound of a hungry baby is being supplanted by breastfeeding manuals that cannot teach that sound to the new parent. If you observe non-Western cultures all around the world, babies are given pre-lacteal feeds or milk through wet nurses when mother’s milk is not enough in the first days of life and beyond because instinctively, we as a species protected our newborns by responding to their hungry cry. Thousands of years of evolution have wired mothers to respond to this cry and we are interfering with a biologically protective instinct by telling mothers that their child is getting enough when it is apparent to them that they are not. Babies get admitted to the ICU lethargic, jaundiced and dehydrated every day because their mothers did not know it was possible to have insufficient milk. The most recent publication on hospitalizations for newborn jaundice at a hospital system with high exclusive breastfeeding rates showed that out of 104,468 babies born in a 3 year period, 12.4% of newborns developed excessive jaundice and 5.7% needed hospitalization for phototherapy, the majority of these cases completely preventable with early supplementation. That means millions of babies have been hospitalized since the 1991 publication of the Baby-Friendly Hospital Initiative which codified this protocol. The Baby-Friendly Hospital Initiative and the WHO breastfeeding protocol protects the breastfeeding more than it protects the baby and countless babies have endured days, weeks, and even months of hunger in order to meet its goals.
The time for magical thinking has ended. Breastfeeding education is based on many premises not consistent with reality. Individual health professionals and even mothers have been blamed for accidental infant starvation when in fact, it is the system of breastfeeding education that fails to adequately educate and counsel health professionals and parents on the serious risks of insufficient feeding from exclusive breastfeeding. No time in the history of this planet have we allowed babies to cry out for milk for as long as we tolerate for the purpose of breastfeeding. The first law of nature is and has always been that Fed is Best. Many parents are led to harm their own babies because of what they have been taught about breastfeeding. As you can see, if such a severe case of jaundice and dehydration can occur to two physicians taking home their first-born son, it can happen to anyone.
To all doctors and parents, my message is simple. Feed your baby. Provide your baby its physiologic needs every minute, including the days before milk production. The only person who knows what a newborn needs is that newborn. The accidental starvation of a newborn child is a tragedy by any definition. We are allowing newborns to receive less than their nutritional requirements and telling parents that they are doing what is best for their children. We must be certain an infant is actually getting fed by every available mean. I hope you join me in informing your colleagues, friends, and family of the data and make changes to your practice. Please feel free to share this letter with whomever you wish.
Respectfully,
Christie del Castillo-Hegyi, MD
[email protected]
Unfortunately, serious complications occur routinely among newborns who undergo the Baby-Friendly exclusive breastfeeding protocol, namely excessive jaundice, excessive weight loss, dehydration, hypernatremia and hypoglycemia. We would like to help your family protect your baby’s future.
Read the Stories of Thousands of Families, Nurses and Physicians Who Signed the Fed is Best Petition
If I Had Given Him Just One Bottle, He Would Still Be Alive.
Hospital Drops Baby Friendly Program After Doctors Baby Was Harmed
Two Physicians Describe How Their Baby-Friendly Hospital Put Their Newborn in Danger
Jillian Johnson: My Message To Parents During World Breastfeeding Week-Just One Bottle
NICU Nurse Discloses Newborn Admission Rates From Breastfeeding Complications in BFHI Unit
Nurses Are Speaking Out About The Dangers Of The Baby-Friendly Health Initiative
Neonatal Nurse Practitioner Speaks Out About The Dangerous Practices Of The BFHI
Information for Hospitals: Ensuring Safety for Breastfed Newborns
Fed is Best Statement to the USDA Regarding the Harms of the Baby-Friendly Hospital Initiative
Dangers of Insufficient Exclusive Breastfeeding Grand Rounds Presentation
National Women’s Health Advocate Describes How A Baby-Friendly Hospital Starved Her Baby
Nurses Quit Because Of Horrific Experiences Working In Baby-Friendly Hospitals
How To Prepare For Supplementing When Breastfeeding Your Baby In The Hospital
To learn more about the Fed is Best Foundation, please go to our About page.
Disclaimer: This document does not replace in-person physician evaluation and treatment. This document is meant to inform parents of the most recent data regarding infant feeding and to increase their knowledge on how to protect their newborns from hyperbilirubinemia, dehydration, hypernatremia, hypoglycemia and extended or repeat hospitalizations due to complications from underfeeding. Earlier supplementation may be needed for babies who are premature or have medical conditions. It is recommended that a parent seeks evaluation by a pediatrician for any concerns regarding the health and safety of her baby if they arise.


Dr. Christie, my daughter, after reading all in the above, I cannot stop crying with joy. I know for certain now, that you, my only daughter is doing God’s work. God chose you in this mission to prevent millions of babies today and many generations ahead from a lifetime of misery and sometimes death. At present, you have more than a million supporters. You have already made a difference in many lives. Anak (my child) keep the torch burning with love, for one day the Universe will say ” Thank you Little One for a job well done”. God Bless, my child!
… And let us bow our head in thanksgiving that God has inspired you with passion to use His gifts of caring for the health of others and given you the time to do it.
Praying for you always, Mom
a lot of time, i hear that breastfed babies are usually jaundice, and we accept it without explanation thinking that it shouldnt be the case since, breastmilk is the best for babies. but now i realized why breastfed babies are jaundiced because they might be suffering from hypoglemia, dehydration or starvation. scary. i was even told by a midwife that a baby can survive up to 3-4 days even without feeding. i am glad i never listened to these. much as i wanted to exclusively breastfeed, i knew very well that i wasnt producing enough milk, because i myself would lose weight terribly every after giving birth. like, i myself could not sustain my own body, much less feed another human being.
I just used my common sense and my mother instinct to give my newborn formula milk. I had no problem with breastfeeding my first 2 children, but with my last, he can’t get enough off of me. So you see I am not a new mother, and I panicked that I do not have enough milk because I used to have so much that I donate my own breastmilk while I was still at the hospital when I gave birth to my eldest.
The hospital was very strict. “Baby-friendly”-my-@$$! Sorry for the word but I mean it from the bottom of my soul.
They confiscated the formula my husband had bought because they are “BABY-FRIENDLY”.
Just so these narrow-minded people would know, I lived healthy. I ate healthy foods and stuff on my last pregnancy that I never had the opportunity to take on my 1st pregnancy.
I slept 8-10hrs a day, drank lots of water and juices, took my vitamins, loved the veggies and ofcourse the fruits. My only fault was I was crazy over rice that lead me to have pre and post-eclampsia.
The 1st day I gave birth to my youngest, I was confident that I can give milk. He sucked and fell asleep. I thought we were fine. After a few hours, the doctors and nurses came and had put on me 3 dextrose, 1 on my left and 2 on my right hand, and a catheter down below. I looked like a puppet on strings.
That night, he kept crying even while breastfeeding. Another mom said maybe he wasn’t getting enough and offered her breastmilk. I accepted since I am all tied up in bed and have no choice. He got quiet and had slept peacefully after feeding from her.
Next day, he won’t stop crying again. His fontanelle had sunk and any mother would know that the baby is very hungry. I kept giving him my breast but it seems like he can’t get enough. We tried for hours and I was almost crying because it wasn’t planned! It wasn’t going as it should! I don’t have enough milk! I COULD NOT bear to see my little boy go hungry because mommy cannot produce enough to make him thrive. Each wail sends thorns through my heart.
So, my husband and I had decided to get him formula milk as soon as possible.
I let my little one feed and I saw his comfort as he slept. I knew I was doing right not to get him hungry. I was bottlefed too when I was an infant and I don’t want to brag, but I can say that I made my momma proud with what I am today. That is why I am not afraid of using formula milk and do not believe in that BS that breastfeeding classes teaches us (yes, I still attended even though I already was a pro). They say it is poison. They say it causes the child to have animalistic character. They say it causes the child to be stupid. Well? They’re all BS.
3rd day and the nurses found out that I am hiding a bottle of formula milk. They confiscated it and shamed me in the ward filled with patients and visitors because they are “BABY-FRIENDLY”. Stating that I just DON’T KNOW how to breastfeed properly and that I am lazy and that the baby isn’t really hungry and I am just overfeeding my boy because babies don’t get hungry right away. I was like WTF???
Guess what? My baby cried himself to sleep because I was FORCED to breastfeed only. Looking at his little face, sunk and fontanelle is so deep, mouth weak, I cried with him til I fell asleep as well. It broke my heart to think that this is the baby I almost died for. My son. My hungry little boy. Mommy is making him hungry.
4th day. Our last day in the hospital. Boy did they get a piece of my mind. Nobody is going to make me starve my baby. They told me to continue exclusive breastfeeding at home so that the kid could get high IQ because formula milk cannot give it. I was like, hey, I used to compete in international math and science competitions representing this country, but I was bottlefed. Will that make my kid an Einstein then? After a series of debate and agonizing reasoning with stupid narrow-minded people who does not even have any idea on where I am coming from, we finally went home.
I fed him formula milk. He grew stronger than my eldest did during their 1st few months. He is a curious and smiley baby now. He likes discovering new things. And, yeah, he is more advanced than babies his age. I knew I made the right decision. The decision to make sure that my baby gets fed.
When I read this article, I was like, FINALLY!!! THANK YOU!! Though there are closed-minded people here that doesn’t agree that fed is best and insist on exclusive breastfeeding, just don’t mind them. They will never understand til they experience it. Hard-headed, narrow-minded and judgemental people are what’s wrong with the world today.
Wow, that’s insane. I can’t believe they actually confiscated the bottle! My hospital is pro-breast feeding but they at least recognize-yeah, baby needs to be fed. I would loose my mind on them, lol. When I was in nursing school I’m grateful that my teacher emphasized that no, formula is not the devil’s elixir! Your baby will be fine on formula if u have to! Lol. I don’t personally like all the crap in formula myself, I’ve recently been trying out goats milk and that’s been working great. I’m glad you had the sense to know and fight for your baby’s needs ?.
Please make sure your baby is getting all the vitamins they need. B12 and iron deficiency in EBF babies as well as babies who do not receive vitamin supplementation through their milk can cause developmental delays. Speak with your pediatrician.
I am very sorry for the problems you have had. Please understand that every IBCLC knows Rule #1 is Feed the Baby. Blaming the “Lactation Community” is not helpful. We devote our lives to helping mothers and babies succeed with breastfeeding. Recognizing problems, educating parents, and intervening are things we do every day. As previously stated, it sounds as if warning signs were missed when breastfeeding was not proceeding normally for you and your baby.
Lyn, I welcome all IBCLCs to come to terms with the harm that is done when facts about commonly occurring life- and brain-threatening complications from exclusive breastfeeding are hidden from mothers to promote exclusive breastfeeding. That is a form of patient endangerment that is unprecedented in medicine. It is unethical and threatens the life of a newborn child. When the IBCLC community chooses to promote breastfeeding ethically and safely, by informing mothers of the common possibility of insufficient milk and the common need for supplementation, then will I consider the LC community as valid and responsible members of the healthcare community. In the mean time, there are many more mothers than me that you and your colleagues need to apologize to. Christie del Castillo-Hegyi, M.D.
I too am and IBCLC of 30 years. Education of mothers, nurses and physicians about breastfeeding is an ongoing need. Education in lactation has evolved over the years for LC’s and the patients we care for. I use EBP to direct my care – one mother and baby at a time. Parenting classes may be helpful with the basics, but honestly each mother and baby should be provided with a complete evaluation and feeding assessment. A follow up by a lactation consultant post D/C can evaluate maternal and infant risk factors that may preclude exclusive breastfeeding so as to avoid poor outcomes. This unfortunately is not uniformly provided in the US. HCP’s and LC’s need to be able to use the word formula in conversation and practice if it is medically warranted and or is needed to achieve long term success with breastfeeding. Some physicians and nurses who do not make breastfeeding a priority in their professional practice may be giving grossly inaccurate information they may or may not have learned well years ago. Social media may also be giving completely erroneous information pro or against breastfeeding. Practice changes occurs with an ever changing body of research, in all fields of medicine and nursing. All pediatricians, lactation consultants and others disciplines supporting breastfeeding mothers and babies, need to keep up with the current research and individualize care for them. To do nothing less, is to put mothers and babies at risk such as what happened to you and your child. If that could occur as it should, perhaps we wouldn’t need to have our legislators looking quite so intently at public policy about breastfeeding
We agree that there should be more education on the science of breastfeeding including updating lactation consultants on the newest data regarding brain injury from starvation due to insufficient milk production. The first update should be that colostrum in fact has fewer calories than mature milk and that an average mother produces a tenth and a third of a 3 kg newborn’s daily caloric and fluid requirement on the first two days of life, respectively. Respect should be given to that fasting child in that a newborn who is crying inconsolably despite breastfeeding is in fact hungry and by definition starving. Newborn weight loss is in fact fasting and 10% of healthy, term EBF newborns are in fact hypoglycemic to a level that has been shown in the literature to cause brain injury and long-term cognitive declines. The historical data on native breastfeeding practices show that in fact that all breastfeeding countries, before the WHO guidelines, supplemented their newborns with pre lacteal feeds or milk from wet nurses to prevent dehydration, jaundice, hypoglycemia and death from starvation. We have taught LCs and health professionals that these pre lacteal feeds are unnecessary and dangerous when they protected babies from brain injury and death from starvation. I suggest you watch the videos on jaundice and the effects of underfeeding at https://fedisbest.org/resources-for-parents/preventing-complications/ to get this update on the current literature. Furthermore, we believe that mothers need evaluation for risk factors for underfeeding before their baby experiences complications. This can be done by looking at the checklist found on https://fedisbest.org/resources-for-parents/feeding-plan/
Very interesting. My experience of hospital was that to resort to a bottle was a sign of failure. Breastfeeding was upsetting as I simply could not tell how much my son was getting. I’d had a difficult birth & got little support regarding much tbh. In the end, I asked for formula too & my son was fed on both for 6 months, keeping him on the highest weight centiles. Got no support regarding breastfeeding other than a distinct air of disapproval! Tried expressing but without that support, it was disastrous. Formula was vital in keeping my own sanity as well as in feeding my boy. I’ll never know if he was fed well enough in those first few days. He has an Autism diagnosis by the way, sensory & fine motor skill problems. Fortunately he is intellectually sound. I’ll never know how much of this will be down to any poor decisions made in his delivery & first few days of life in hospital or whether it’s genetic disposition, but I wish I’d been aware of these points regarding feeding beforehand. Thank you for sharing.
Thank you very much for speaking out on this important topic. We went though something similar – and gave formula to our newborn son on day 2. I was under a huge societal pressure to not give formula so early, but i knew from my baby’s cries that breastmilk was not sufficient for him. We transitioned to fully breastfed a couple of days later. The guilt associated with the initial formula feed was enormous. And every breastfeeding resource says that we do not need to supplement with formula the first few days. That breastmilk is sufficient. Based on personal experience, I disagree. This might be true for some, but not all. Thanks again!
On a side note- It is very common in India to supplement with formula before mother’s milk comes in between days 3-5. They usually do it with a spoon so that there is no nipple confusion. It is more of a taboo in the US.
Dear Dr. Del Castillo-Hegyi. Thank you so much for this article. My daughter was fortunately able to receive enough breast milk in her first 6 months of life, but not so in her 2nd six months. For me it was pediatricians pushing me to ween her off night feedings and let her “cry it out to extinction.” I tried it, I failed, and it was horrible and completely against my maternal instinct. It turns out I wasn’t producing enough, so that’s why she was crying. She was diagnosed with failure to thrive by one year. They then told me I needed to feed her a high fat diet. Put butter in everything, basically. She is now seven, and fortunately she is ahead of most of her grade level in most subjects. Her emotional development is behind, however. She has intense phobias that take at least 6 months to a year to resolve, and are replaced by a new phobia every year. I wish I could have gone back and read this article so that I wouldn’t have felt bad if I wanted to at least give her a bottle before bed time. There’s sooo much pressure on new mothers to follow a certain path and not a lot of common sense in just listening to instinct… I’m curious if you have any research on what mothers did in early history without formula to supplement with. Did they share breast feeding with other lactating mothers or use goat or cow’s milk? Maybe using a “wet nurse” was common before formula came along.
Hi Katie, I am so sorry for what you and your daughter went through. I agree, mothers are being taught to ignore their instincts to feed their babies. As a special needs mom, I know how difficult emotional development problems are. Before formula, mothers supplemented with whatever they could, milk from wet nurses, animal milk, anything safe. I’m sure they fed their babies pureed and even chewed up food, which I just learned from another reader, they do in her country. Feeding is SURVIVAL. Mothers used their brains to come up with any way to feed. I hope we can reach as many mothers as we can to relearn that basic evolutionary wisdom.
Hello,
Your article and the information you provide are very informative and important. Thank you for advocating for increased awareness of the need for thorough comprehensive pt education and close monitoring and standardized ways of evaluating the quality of breastfeeding and the physiological signs that indicate the newborn is actually being fed enough.
Do you know of any studies regarding low Hgb post partum and milk production? A friend bled significantly from a cervical tear during delivery that wasn’t found initially and her Hgb dropped from 135 g/L to 85 g/L (Canadian measurements). Her Dr. chose not to transfuse her.
Thankfully, after several days of struggling with a very hungry baby with an alarming weight loss, she decided to supplement, despite professional advice to do otherwise.
Wondering if the low Hgb could have been a factor in the inability to produce enough milk.
Thank you,
Thank you for your comment Kate! Excessive blood loss and low hemoglobin is one of the most potent inhibitors of milk production. Your friend is lucky that she supplemented her baby despite professional advice. Mothers, listen to your instincts and your babies! Excessive blood loss inhibits milk production likely because a mother who gives up fluid volume and glucose through milk in such a depleted state could potentially compromise her own life by doing so, which, from an evolutionary standpoint, could compromise her baby’s and her own survival.
What I want to know is why is so much emphasis put on breast feeding? I do understand that “Breast is best”, however, why do mothers feel bad for not being able to breast feed? Why do nurses insist on breast feeding? If a child is hungry, why not emphasis on FEEDING THE CHILD PERIOD EITHER BREAST OR BOTTLE!!! As long as they are eating and are healthy, isn’t that enough? I did try for the first 2 days to BF and my son was not satisfied. I finally told the nurse to get formula and once fed, he was happy and fell asleep. It’s not about failing as a mother by not being able to breast feed, it’s making sure your child is nourished, growing and healthy. Why not promote healthy children regardless of how they are fed and just encourage nurses to be supportive of feeding a child. My 3 children (9, 11 and 15 yo) were all formula fed, all healthy and thriving – period!! I don’t feel bad and never have for not breast feeding my children from birth. I refused to be bullied into breast feeding by anyone.
I have no words… During pregnancy I read all the books was intent on following all the breastfeeding guidelines, no supplementation etc. Latch within 1 hour of birth. But then it turned into a C-section and here in Suriname you get to look at the baby which is whisked away to be checked etv while you are stitched up. So by the time I was up in my room baby was at least 45 mins old and I’m pretty sure we didnt latch within 1 hour. This basically only made me more determined to succeed and exclusively breastfeed.
However luckily (I see that now) the hospital is very baby friendly but they do supplement as the standard basically. I remember being so very angry that she was given formula prior to being offered the breast… Changed my tune quickly and quietly feeling like a failure to provide for my child on day 2-3 and asked the nurses to please dear God feed her as she was nursing and clearly not fed enough. So I guess I am trying to say I am so thankful the hospital was not such a Nazilike “babyfriendly’ place that they had no formula in the building.
On day 5 she was lethargic and jaundiced. So back we went.. that was a whol other story because the nurses visually examined her and determined labs were unnecessary. Luckily my Mom went with us (I was severly jaundiced at birth, and sent home because the hospital was understaffed. On day 4 a nurse aunt told my mother this was in no way normal and I was rushed to hospital narrowly escaping brain injury according to the peadiatrician) and we had labs done which were still within range. And my daughter started improving the next day. Never was I told why to supplement or when it was necessary nor did I read it in any pregnancy or breastfeeding book.
Oh and damage to our breastfeeding relationship? Now exclusively breastfeeding 5 1/2 months in and she went from the 15% at birth to 95% today for weight.
Please continue speaking out. You are doing a very important job!!
This was very interesting to me. I am a nurse and new mother and I didn’t know that you could accidentally starve a baby. My milk was very obvious to me, the let down of milk so fast it was almost painful but not all mothers experience that. I also believe that mothers have been taught too much not to trust their instincts and to just do as they’re told. I had gestational diabetes so my baby’s BG was tested as soon as she was born and was immediately given some formula, which I had no problem with. But in the clinic you could hear moms-to-be talking about how under no circumstances were they going to let thier baby have formula-completely ignorant of the dangers hypoglycaemia can hold to a new baby. I have copied the link to this article and sent it to the email of my midwife’s office so hopefully they will read it and know to warn mothers of the potential danger. Thank you for bringing this to my attention.
Hi. Respectively yours, this is not “fear mongering”. This is educating the public in order to make an individual construct an informed decision for the good and health of her baby. I am both a mother (of a 17 and 15 year olds) and a nurse. I love research.
I am so sorry Christie that you had such an awful time and that your son has been through duck an awful time also. I have one question though that I don’t understand. How can your baby have been producing wet and dirty nappies if he wasn’t getting any milk? If nothing goes in, then nothing comes out. Also, women have breastfed their babies since the beginning of time and we are still alive. If breastfeeding was such an issue or needed to be supplemented with formula we wouldn’t ever have survived in the first place. Your research is extremely flawed and you should not be posting such scaremongering letters. Best of luck to you and your son
Helen, the breastfeeding literature has found that dehydrated babies can still produce up to 6 and even 8 wet and dirty diapers on the 4th day of life, because the majority of those diapers are from the fluid and stool their are born with. Hence the weight loss because they are getting an average of only 56 mL of colostrum on the first day of life. That 56 mL provides 1.5 Calories/Hour of the 100 Calories/kg/day a newborn needs. Their kidneys have to urinate after 24-48 hours in order to prevent electrolyte abnormalities that can kill them. EBF newborns are only expected to urinate 1-2 wet diapers the first two days of life, which on any other day would be consistent with fluid deprivation and would be considered an emergency. Our education on newborn feeding is dangerous and lacking in science and respect of the newborn’s human right to be fed.
Did you receive Iv fluids during labour?
Did Bub have ties?
There is no scientific evidence that IV fluids during labor prevent and reduce milk production. In fact, the most common advice given to mothers is to drink more fluids and by extension, IV fluids should improve milk production. One of the most potent inhibitors of milk production is low blood pressure from postpartum hemorrhage. Because a hemorrhaging, hypotensive mothers can die if she gives up fluid volume and glucose by lactating. My son’s latch was perfect according to the LC and having breastfed him for 20 month, his latch WAS perfect, no pain or nipple trauma. There was simply no milk and the causes of delayed and failed lactogenesis II are primarily biological and genetic, which are out of the hands of mothers and lactation professionals.
She is educating people. How is that unacceptable?
I don’t see how starting a balanced discussion about breastfeeding is fear mongering.
We agree!
People from continental Africa,with supposedly unclean water do not experience the First World have, I wonder why. My mother nursed my nine siblings including myself. Fortunately, she was a British trained nurse.
She told me a child loses a few pound after birth. But with feeding on demand and good rest. The newborn regains this weigth.
I am a mother of 3 all breast fed. 5’14” by 2 months was 10lbs fed 8 months
6’2″ fed 8 months
5’11” fed 24 months
Of course in African culture, a child sleeps besides the mother until, maybe 6 months.
That love and warmth is more nurturing that nursery rooms etc.
In my opinion and from experience newborn new mother comfort that a room, this baby does not appreciate.
Not all babies in Africa exclusively breastfeed without complications. In fact, the highest rates of hyperbilirubinemia along with the hospitalizations, long-term disability and mortality occur among jaundiced and dehydrated African babies because of the exclusive breastfeeding guidelines. Prior to the WHO guidelines, breastfed babies were almost universally supplemented in the first days of life to keep them from starving and become dehydrated. That is an incorrect perception of exclusive breastfeeding in Africa. http://www.njcponline.com/article.asp?issn=1119-3077;year=2016;volume=19;issue=1;spage=1;epage=17;aulast=Olusanya
This happened with my baby too! But we were fortunate enough to have a great pediatrician. So when we went for our 2 day follow up and she had lost a pound and was not having food bowel movements he started having me supplement and gave her a bottle before she left the office! He also checked her bilirubin and hospitalized her for jaundice. Then consulted a lactation specialist who tried to express milk and realized I was producing very little! Although there was a very scary 24 hours that she didn’t urinate. I’m so glad they caught it in time. She is 18 months old now and seems to be normal. Pediatricians need to become more aware of this problem so that what happened to your child does not happy to others. With what we are taught about breastfeeding I felt like such a failure when I had to start supplementing and that is not the case.
Thank you for sharing Sarah! We believe that mothers should know ahead of time whether or not they have breast milk to feed. That is why we advise mothers to check their breasts before every breastfeeding session, especially in the first days of life because some mothers do not produce colostrum. It is unacceptable for newborns to go hungry for the purposes of exclusive breastfeeding. Pediatricians and LCs need to be more aware of these problems and view them as UNACCEPTABLE. We hope to change our understanding of newborn and infant feeding and reprioritize feeding over breastfeeding.
Thank you for writing this. I am a well educated and sensible woman but after all three of my children were born felt pressured to stick with breastfeeding when there was clearly insufficient milk. The third was a late in life baby and my husband and I joked that this time around we wouldn’t fall for it. As my two older girls were failure to thrive. Thank goodness the pediatrician insisted on supplements immediately. But even with number three my husband walked in and I had the baby latched on. He was shocked, but I was tired and hormonal and felt pressured. I said I’ll just do it here and switch when we get home. There is definitely a stigma to not breastfeeding or supplementing.
Thank you so much Janet for commenting! We have heard from many mothers like you about the tremendous pressure to breastfeed exclusively, even when there is insufficient milk to do so. We believe that newborn starvation and failure to thrive are unacceptable consequences of the campaign to promote exclusive breastfeeding. The campaign does not use science nor does it respond the reports of negative consequences to newborns and infants to change practices that have been proven to be harmful. Please keep sharing your story and share the campaign letter with others so they can understand the importance of prioritizing feeding over breastfeeding.
Dear christie im muslim n wud suggest u to do research on one of Sunnah of Prophet Muhammad SAW which he suggests for new borns.He use to give chewed date to new borns(u can read it in a book” Bukhari shareef”.)I think it prevents them from hyperglycemia.u r scientist n I gav u just a clue,rest u can find. my faith is on Him wdout any scientific theory.thanks for sharing ur life saving findings.love
Every breastfeeding culture has evolved to provide some source of calories to their newborns before the onset of copious milk production to keep their newborns from starving, becoming jaundiced, dehydrated and hypoglycemic. I believe the human instinct to feed is far more scientific than the current standard of not feeding enough in order to exclusively breastfeed. Thank you for your comment!
I don’t know if I personally I was more concerned about my daughter’s bilirubin being a nurse, but I do know it was high at discharge after her first day. We went home that night, my milk had not come in, and did not come in until day 3 of being home. I had to have a pediatrician reassurance me I didn’t just need to stay and get her phototherapy, instead of just coming back after her lab work in 24 hrs.
Our pediatrican had us recheck her bilirubin the next day, and it was down trending. She thankfully also had no weight loss on our recheck monday following the weekend (labs were done on saturday). Which I attribute to supplementing.
I supplemented with formula and glucose water..and breastfeed some to help with my milk to come in, but the importance of the bilirubin coming down with feedings outweighed my breastfeeding concern (though I cried about it and that she would have nipple confusion, she didn’t). We also took a few naps in front of the window to get even some winter sun.
I guess the lesson from my experience is that it is explained to parents the importance that the bilirubin go down, get it rechecked early and that it is okay to supplement, your baby will figure it out, as will your body.
We agree! Being fed and reducing your newborn’s bilirubin is far more important than exclusive breastfeeding. A mother is not a failure by providing supplementation. She is protecting her child’s brain and life with supplementation while improving her long-term breastfeeding success.
Wow!!!!!! I’m literally balling here. I was starving my child for several months without realizing it. The pediatrician kept reassuring me time after time that my son was just going to be very tall and lean. The lactation consultant reassured me that he was getting enough milk. I was able to successfully exclusively breast-feed my firstborn so I felt confident in my body being able to produce enough milk.
My son was tongue-tied at birth and all the doctors lactation consultant and nurses kept telling me that he wasn’t. I followed my gut instinct and took him in to see and ENT specialist Who informed me that in fact he was tongue-tied. I figured that his feeding would improve after that but little did I realize that it didn’t. It never occurred to me to check to see if my body was producing enough. Thankfully he did not get dehydrated or have any of the other symptoms which some people seem to have experienced. It seems as though my body was producing about 1 to 2 ounces which at the beginning might be enough but as he got bigger it did not. He would constantly cry and my doctors assured me that he was just going to be a fussy sleeper. I tried everything. My son is now five years old and the guilt still weighs heavily on my heart.
He was developmentally delayed and needed lots of therapy. He will always have low muscle tone. This is the first time that I’m hearing of other people going through something like this. For once I feel like I’m not alone. Honestly feel like there should be a support group for us mothers who have gone through something like this
I am so sorry for what you had to go through. Thank you so much for writing this article.
I am so sorry that you and your son experienced this. My heart goes out to you. I hope with enough education, we learn how to prioritize feeding over breastfeeding. Breastfeeding at all cost is not best. Fed is best because the brain does not wait for food.
If your baby was tongue tied, it probably prevented you from fully feeding him (leaving dessert in the breast) and that resulted in low milk supply over a period of time. Babies should meet their benchmarks for weight. HCP do the baby disservice by “following them” but not referring to an IBCLC when this occurs. Regaining birthweight by 2 weeks and doubling birthweight by 5 months and tripling at a year is the long held standard. That said, for LGA babies. not quite but they should be following their own growth curve. I have seen babies be allowed to go up to one month to regain their birthweight and that is just too long. There are interventions that keep this from happening and it may or may not require formula.
For all we know about how breastfeeding works, this can be avoided, really!
Ultimately, it is the baby that knows best whether they need more milk. No IBCLC, pediatrician or breastfeeding guidelines can protect a baby from starvation better than listening to a baby’s hungry cries, watching their weight gain and using your maternal instincts. That is how we knew how to supplement for millenia and that instinct is what protected babies. We fed with our brains, not just our breasts. If there were no alternatives and a mother did not produce enough milk, her baby died. You offer a very simplistic view of breast milk production which does not account for a mother’s innate limitations to produce milk. Much of what is taught to IBCLCs about what causes delayed or failed lactogenesis II is biased by the belief that all mothers need is an IBCLC to produce milk. Biology is the main determinant of milk production, next is breast milk management. Babies starve even when an IBCLC is involved (often times because they are encouraging mothers to just breastfeeding).
My son cried constantly and I begged the nursery nurses to let me bottle supplement. They flat out told me
“No. Keep breast feeding.” He became very jaundice and had to stay in the hospital an additional 3 days and then was sent home on billi lights. He has fine motor issues, he cannot tie his shoes, he cannot ride a bike, and suffers from an emotional disorder that nobody can really explain. He has had an EGG that shows an abnormality in his left temporal lobe. I have ALWAYS thought that all of his issues are related to being starved from birth. I was an insecure, scared, first time mom and felt powerless. I refer to the nursery nurses as the “breast feeding Nazi’s”.
What was his bilirubin level and was he hypernatremic?
“In addition, the Academy of Breastfeeding Medicine jaundice protocol clearly states that 10-18% of exclusively breastfed baby develop starvation jaundice from insufficient milk intake, a fact disclosed by no breastfeeding manual.” — This is appalling. How about informing new moms to watch out for this instead of telling them that if they’re breastfeeding all the time everything will be alright? Because that’s the takeaway you get from all the information thrown at you when you decide to breastfeed: as long as you’re feeding all the time, you’ll be alright. Just keep feeding.
Also I despise, absolutely despise, the moralistic tone moms get when they say breastfeeding is difficult, share their breastfeeding problems, etc. “You just didn’t work hard enough” is incredibly condescending and dismissive of moms who have, in fact, worked incredibly hard. In my case, my son would breastfeed for up to two hours at a time, fighting to stay latched for maybe thirty minutes of that time by the way. I clearly remember one time when three or four nurses, for 45 minutes, tried to help with latching (thank goodness for nipple shields, that did the trick). And then after feeding, about an hour later, the process would start all over again. That went on for a week after his birth, in the hospital and then at home, until his 7th day when his pediatrician recommended supplementing because he had lost 1 lb post discharge. Go ahead, tell me I didn’t work hard enough. (NB: Eventually breastfeeding got easier. After 8 LONG WEEKS. We supplemented the whole time.)
The underlying assumption seems to be that formula is so awful that anything and everything should be tried in order to avoid it. Why else would everybody and their mother push breastfeeding so hard and make it clear that even one bottle, one pacifier, can ruin everything? And yes, maybe that’s not the official position but informally, that’s the gist of the message: Exclusive breastfeeding or you’re a FAILURE. That level of absolutism shows how dogmatic the thinking can be behind all of this.
Dear Leaj, Thank you so much for sharing your story. What is taught to mothers is dangerous and reckless. There is literally nothing in medicine that is as much a violation of patient rights as the Baby-Friendly Hospital Initiative. Sadly, everyone is taught the same things and we are pressured to agree with the prevailing dogma when what we see with our own eyes, as mothers and even healthcare providers run contrary to what they want you to believe. There ARE limits to breastfeeding, and that is when a child is harmed by it. Accidental starvation is not just a child skipping a meal or two. They are often skipping many meals for days until they cannot stay awake. It is NOT RIGHT and the idea that there are people who are still defending this system is appalling, as you say it. As of the most recent statements by the ABM called, “Of goldilocks and hypernatremia,” they did not support warning mothers about the dangers of newborn brain injury from insufficient breastfeeding because breastfeeding is apparently more important than the safety of a few thousand newborns. At one point, they used newborn deaths caused by Nestle as a battle cry and now they wish to hide their own mistakes from the general public, even if it means disabling a few thousand babies. Keep sharing Leaj and thank you for your support! Christie del Castillo-Hegyi, M.D.
I think it’s great useful article. Thanks So Much
Thank you for writing this. I struggled with breastfeeding my son, who was born at 37w1d because of my pre-eclampsia. He was small because of undiagnosed IUGR. We supplemented in the hospital, but stopped once my milk came in because that was encouraged by the nurses and lactation consultants. He was actually discharged from the hospital before I was. It was really rough caring for a newborn while I was still hospitalized. We discovered when he was 10 days old that he was tongue tied. My husband and I just thought it was a figure of speech and were quite surprised it is a real thing. The pediatrician who saw him ordered us to feed him formula and if he didn’t gain weight over the weekend, he was going to be admitted. Well, he was admitted the next day anyway for a fever getting late onset group B strep. He was discharged 3 days later. The day after he came home again, he visited the ENT who called me a saint for even attempting to breast feed. One short surgery later, my son could move his tongue like he never could before. I didn’t know he wasn’t getting enough milk from me before. I was a new mom and it seemed like he latched fine and the consultants said he was fine. He never really nursed from me effectively, so he got formula and breast milk that I pumped. The hardest thing to have ever read was failure to thrive. He’s over 1 now and healthy, thriving, and smart. I tell all moms to be now to not feel bad about supplementing because sometimes you have to.
Just wanted to chime in that supplementing for me saved our nursing relationship & my son never went hungry. I was so upset when I realized I needed to supplement, & basically accepted that nursing may not happen for us. My son was on almost all formula for about 6 weeks (I was hand pumping as little as 2oz/day because of terrible nursing tears). When he was 2 months old I reattempted nursing, with success, & we transitioned slowly to mother’s milk. My baby never went hungry, the bottle did not ruin his latch but did provide relief. He’s 19 months old & still nursing. I regret the many tears I shed over using formula, based on propoganda that served an agenda but neither myself nor my child. Formula can help.
Thanks for sharing. So glad that The US Preventive Task Force have also been looking into this. And JAMA has just published an article with your same conclusions.
http://www.medicaldaily.com/breastfeeding-facts-and-myths-2016-us-task-force-updates-advice-402370
Lack of proven efficacy for exclusive breastfeeding during
the newborn period to improve breastfeeding duration is
important, because exclusivity during the newborn period
may not be free of potential harm. For example, the onset of
copious breast milk production varies.13 For women who
have scant colostrum and no copious milk production for 4 to
7 days, exclusive breastfeeding in the first few days after
birth is associated with increased risk of hyperbilirubinemia,
dehydration, and readmission.14-16 Although these conditions
are generally mild and often resolve rapidly, their frequency
is high; 1% to 2% of all US newborns require readmission
in the first week after birth, and the risk is approximately
doubled for those exclusively breastfed.15,17 If counseling to
avoid food and drink other than breast milk is not an effective
method to support breastfeeding, the frequent low morbidity
and rare high morbidity outcomes could potentially be
avoided without reducing breastfeeding duration.
THANK YOU! We are posting a blog about this very article tomorrow! Stay tuned!
But if there was no supply. How did the baby had enough wet and dirty nappies
According to research on wet and dirty diaper counts, a newborn who develops dehydration of >10% can still produce up to 6 wet and dirty diapers even on the fourth day. Which means they are producing diapers from the fluid and meconium they are born with. That is why they lose so much weight. They have to eliminate to maintain their bodily functions even if they are receiving nothing.
I too fed on demand and still couldn’t produce enough. I pumped, I took tinctures, I massaged, I drank tea…still didn’t make enough. Fed is best.
So sorry this happened.Thanks for sharing
Thank you for the work you’re doing. My son, about to turn one, ended up in the NICU on day 5 after his temp slumped to 96 degrees. He was hypoglycemic and immediately put on IV sugars. I was producing some milk, but just not enough to sustain him. The good news was that the hospital lactation consultants told me to supplement, the bad news was my pediatrician told me to wait, even though he wasn’t producing wet or dirty diapers. Her words were exactly as you stated: colostrum is fine, your milk will come in, just wait. She even told me he wasn’t wet because the diapers were so absorbent! Needless to say she’s not our pediatrician any longer. The medical community just needs to remember that every case/child/mom is different and “fed is best.” I wish you the best in your work.
Fearmongering?? I call this new information I had no idea about! I breast feed my children who are grown and now have children of their own who have been breastfeed and we all were lead to believe all they need is the breast. Thank you Christie for sharing your story it opened my eyes!
Thank you so much for advocating for this cause. My daughter is four months old and as new parents we knew nothing. Neither of us were ever really around babies during our adult life. We wanted to do what was best for our daughter and had planned on exclusively breast feeding. She was born at 36 weeks and was able to latch wonderfully, but her blood sugar was low so they supplemented her before we even left the delivery room. We continued to supplement her at the hospital. We met with a wonderful lactation consultant who was very passionate about breastfeeding but not pushy.
When we went home I tried to exclusively breast feed, but she seemed to need to eat constantly and I was afraid she wasn’t getting enough so I still supplemented a couple times a day. The first week of her life we were at the pediatrician three times within a week and half monitoring her weight. She had lost about a pound, so we started breast feeding, pumping and supplementing on schedule.
I appreciated our pediatrician, Dr. John Markovitch, for not making me feel ashamed of this. There is a stigma with new Moms that if you are not exclusively breast feeding you are not doing what is right for your child. I completely disagree. It is your responsibility as parents to make sure your child is healthy and thriving. Do NOT be ashamed of using formula. The pain of something happening to your child would be much worse than the pain of feeling disappointed because you aren’t able to exclusively breast feed. Also, I have heard people say that if you are pumping and your baby is eating breast milk out of a bottle, you cannot consider them 100% breast fed. Please don’t listen to those people. I am a Mom with a career and I was back to work within seven weeks. Exclusive baby to breast feeding simply is possible for the majority of us who aren’t able to stay home. There is no shame in that.
New parents just don’t know. They don’t know how a baby should behave. We were up some very late nights, made a few frantic phone calls asking if this or that was normal. If I’ve learned anything, babies do a lot of “weird” things all of which are “totally normal.”
I never had much of a supply to begin with, and after my unexpected gallbladder surgery eight weeks post partum, my supply dwindled to nothing. My daughter is now exclusively on formula. I have felt some guilt over this, but she is growing, healthy, happy, and advanced for her age. She is strong and not over or under weight. Your baby will be okay and so will you, as long as you are making the best choice for your baby.
Fed is best.
I am constantly astounded how quickly we forget history. History is full with annotations and remarks about wet nurses. This is not a modern phenomenon. Their existence has been noted well before the advent of commercial formula milks. Why have we or rather the medical profession forgotten the presence of these women? It is in the literature of the past. The sheer fact that formula has come about is because of a medical need for supplementary feeding for infants of women who have inadequate supply of milk and not out of “laziness” that we so often hear.
I am the third generation of women who could not breastfeed solely. Unlike my mother and grandmother who were nursed with straight cows milk, I was fed on the early types of formula in the 60’s. So too, I had to feed my first born with formula, however this time it was traumatic. The insistence of the nipple drove me to PND. Until I was bat crazy, then and only then I demanded formula, and started comp feeding (breast and bottle).
I am still quite angry about it. And now I have now just read two tragic stories of infants dying of starvation, I think its a crime to insist breastfeeding when the tissue is not producing enough milk. This goes to show that the health practitioners do not know enough history nor do they know enough of biology. The careless notion that every woman can breastfeed is simply wrong, dangerous, and lethal as we have seen here.
So please remember HISTORY, there were wet nurses simply for the purposes of nursing other women’s babies when their supply was inadequate. There fore FEED YOUR babies and forget the NIPPLE NAZIS.
PS. My second born was comp fed, breast and bottle from day one of birth to 6 months. She’s fine and thriving, plays two musical instruments and is cheeky as hell. So far no allergies, and she’s 14. My first born is 17, 6 foot 3′, no allergies.
I’m a pediatric sub-specialist, but I remember during my pediatrics residency some of the lactation consultants in the nursery and NICU would make new moms cry. One lactation consultant screamed at me in front of a family because I told them that their jaundiced and underweight baby would need to be supplemented with formula. (Other lactation consultants were wonderful, treated families like they were their own, and taught me a ton.) I would see the moms in follow-up in the clinic and some whose milk had not come in or who were having difficulty breastfeeding were so distraught. They couldn’t enjoy their new babies.
While breastfeeding is awesome and important, a mom’s sanity and a baby’s well-being are more important. I am totally pro-breastfeeding, but I know that supplementing with formula is not a failure, nor is feeding your baby formula full-time. And we need to make sure parents understand that. Formula does not equal failure.
Getting through the first few weeks is about survival. The laundry and dishes are going to pile up, you’re probably not going to be able to shower every day. And maybe breastfeeding isn’t going as smoothly as you hoped. It’s okay. And I think new moms need to be told that it’s okay and that giving their babies a bottle of formula every now and then (or for every meal) doesn’t mean they love their newborns any less.
Who’s funding you—Enfamil?
We are funded by our own salaries and the private donations of mothers whose children have been harmed by the exclusive breastfeeding guidelines. I am a physician, scientist and mother whose child was nearly killed by the exclusive breastfeeding guidelines. We are warning mothers of the dangers of accidentally starving their babies because the consequences are severe and irreversible.
I had 5 healthy babies back in the ’60’s & bottle fed them all from the start with normal weight gain & no health issues! I can’t see why breast feeding is so recommended & enforced over bottle feeding. The hospitals are there to help people & make sure their lives are not in danger! If the baby’s parents do not request that bottle feeding be started before it’s too late, then the parents are responsible for the child’s death! I would have immediately switched my baby to bottle feeding, seeing that the results were so detrimental & life threatening! If you want a healthy, happy baby, a word from the mother is all it takes!!!
My sons & daughter are all in their ’50’s now, with their sons, daughters & grand kids, all living healthy, happy lives in their own homes………
I wish I would have known about this page a little over a year ago. Prior to the birth of my daughter last January my husband and I signed up for birth classes, toured the hospital, and were hyped up to exclusively breast feed. The hospital, of course, pushed breast feeding hardcore. When my daughter was born they cleaned her up and laid her on my chest where she marathon fed for almost 6 hours. It seemed that no sooner would we lay her down that she would fuss for another feeding. The lactation consultant assured me that everything was fine and that some babies are marathon feeders. We get discharged 48 hours after birth. After a few days at home I’m completely frazzled from having nearly no sleep. I attempt to pump so that maybe my husband could feed our daughter so I could sleep. I barely got a dribble out. Exhausted I laid down and slept like the dead for over 2 hours. I was nearly frantic when my husband woke me telling me that he fed our daughter some formula from a small sample we were sent during my pregnancy. He then told me that I was off the menu. Our daughter was sleeping contently with a full tummy and he couldn’t take watching my mental health deteriorate from lack of sleep and success in feeding our baby. I cried, pleaded, and argued with him that we needed to breastfeed. He held his ground and ordered me back to bed and he would go buy more formula the next day. I felt like the biggest failure and the worst mother in the world. But after a couple days I felt better about it. I was more rested. Our daughter was sleeping better and was far more content. I was actually able to bond with her better feeding her formula from a bottle than struggling at the breast where we were both unhappy. She’s going on 14 months now and is the happiest, healthiest lil girl I’ve ever known. I’m still resentful of the brainwashing I received from the hospital, and after reading the stories here I’m glad my husband stepped in when he did.
I have the greatest respect for any woman who is able to breastfeed, but at the same time woman who can’t breastfeed for one reason or another need to stop being vilified and made to feel guilty for doing the best that they can.
I hope new mothers realize that feeding on demand applies to older babies who are well established in breastfeeding. Newborns need to be breastfeeding every hour and a half whether they are acting hungry or not. Wake them up if they are sleeping. Not only will this help make sure baby is fed, but it will establish milk supply coming in too. I have breastfed 6 children. I wish information mothers were receiving about how to breasfeed was more consistently accurate. It seems like it should happen so naturally but women need to know how to properly nurse so that their babies are ok. Newborns can sleep a lot and tired moms sometimes are happy to let them sleep, but you cant! Also, new moms need to know when formula really is needed and not be made to feel bad about it.
Not all mothers have enough milk to keep their babies from starving. Those babies need to be supplemented when they are clearly telling you they are starving by their non-stop crying and nursing. Mothers should feel bad for giving something that will save their child’s brain and life. The WHO Baby-Friendly protocol is criminally negligent for allowing babies to starve until their hospitalized by lying to mothers about the risks of the exclusive breastfeeding guidelines.
I am so glad you are educating parents about the dangers of not supplementing if needed. I am sorry that you experienced this with your own child. My story has a happy ending – a healthy 22-year-old son about to graduate college. However, prior to his birth, I had read the books and was convinced I should not feed him a bottle as this would cause “nipple confusion” and greatly ruin his changes of successfully breast feeding. At the time of his birth, I was an active pediatric nurse working in a medical center and his father was a physician completing his surgical residency. It was also the time of the “24-hour drive-through delivery” when the mother / baby were only permitted 24 hours in the hospital after a normal vaginal delivery. Breast feeding wasn’t going well. I wasn’t “getting it” but I was determined not to “ruin” his chances of successfully breast feeding by giving him the bottle! He became jaundiced and still, I didn’t want to give him a bottle. He cried and cried. His father, thank God, insisted we feed him. He told me he’d be admitted to the hospital for phototherapy if we didn’t give him a bottle. I was a tired, emotional, mess and finally gave in and we fed him. I cried as he drank from the bottle, thinking I was “ruining” everything where breastfeeding was concerned. Now it is 22 years later after reading your story and similar ones, I feel my son would surely have suffered the same fate had his dad not “scared” me with the possibility of him needing phototherapy in the hospital. I just remember being “brain washed” by the books, lactation consultant, etc., to NEVER give him a bottle, especially in the first days of life, as this would cause nipple confusion and ruin his chances of successfully breast feeding. It makes me so sad that we are made to think we are a failure if we supplement and as a result, tragedies occur. Thank you for educating new parents about this. I hope the mind-set changes. Fed is Best.
Thank you to the very detailed points by Mitchmom. In the US the facilities of our entire birth network and medical system is not as vigilant as yours, mitchmom- but they should be and following AAP guidelines to promote safe exclusive breastfeeding. On the other hand, these same systems are not as negligent as what you experienced Christie. What I don’t like to see come out of this is fighting and angry statements misconstrued and mothers fearful that their own bodies will fail them. We don’t need to create fear. We need to create empowerment for moms to educate themselves and make informed decisions that are right for them.
Yes, we need to empower mothers to recognize the signs of a starving on their own with the same information a physician or nurse would want to know for their own child. We want them to learn how to supplement without permission to save their child from brain injury and death because the AAP and the BFHI guidelines weren’t actually studied for safety and the have been shown to fail babies at a very high rate.