by Jillian Johnson with commentary from Dr. Christie del Castillo-Hegyi
Landon would be five today if he were still alive. It’s a very hard birthday–five. It’s a milestone birthday. Most kiddos would be starting kindergarten at this age. But not my little guy. I wanted to share for a long time about what happened to Landon, but I always feared what others would say and how I’d be judged. But I want people to know how much deeper the pain gets.
I share his story in hopes that no other family ever experiences the loss that we have.
Jarrod and I wanted what was best for Landon, as every parent does for their child. We took all of the classes. Bought and read all of the books. We were ready! Or so we thought….every class and book was geared toward breastfeeding and how it’s so important if you want a healthy child. Landon was born in a “Baby-Friendly” hospital. (What this means is everything is geared toward breastfeeding. Unless you’d had a breast augmentation or cancer or some serious medical reason as to why you couldn’t breastfeed, your baby would not be given formula unless the pediatrician wrote a prescription.)

Sleeping comfortably a few hours after birth
Landon was born full-term weighing 3360 g or 7 lbs. 7 oz, born by urgent cesarean due to fetal intolerance to labor after the water had broken. [Previous publication of this blog said he had an emergency c-section. He was delivered by low transverse incision over 12-14 minutes, which is considered an urgent, not a STAT section.] Apgars were 8 and 9 and he was stabilized. He was transferred 2.5 hours later to the Mother-Baby Unit and returned to his mother. He exclusively breastfed with excellent latch for 15 – 40 minutes every 1-2 hours.

Landon, is 12 hours old.
Landon was on my breast —ALL OF THE TIME. The lactation consultants would come in and see that “he had a great latch and was doing fine,” but there was one who mentioned Imay have a problem producing milk. The reason she gave was that I was diagnosed with PCOS (polycystic ovarian syndrome), and it was just harder for women with hormone imbalances to produce milk. She recommended some herbs to take when I got out of the hospital.
While in the hospital, his mother’s risk factors for failed and delayed lactogenesis II (copious milk production) were identified by the IBCLC-lactation consultant. They were borderline diabetes, PCOS, issues with infertility, small, widely spaced breasts with minimal growth during pregnancy, being a first-time mom, and emergency c-section. Despite that, she was encouraged to exclusively breastfeed. She was closely monitored by a nurse, lactation consultant, and physician support. Her baby’s latch was rated as excellent.
By the first 24 hours, he had nursed a total of 9.3 hours, had zero wet diapers and four dirty diapers. By 27 hours, he had lost 4.76%. His nursing sessions became longer and longer until he was on the breast continuously by the second day of life. On the second day, he produced 3 wet diapers and 6 dirty diapers and nursed for almost 14 hours total. By53 hours of life, he had lost 9.72%.
At this time, the scientific literature on wet and dirty diaper production has shown that the number of diapers produced have no correlation with adequacy of milk intake in the first 4 days of life. The only study on diaper counts has shown that even newborns who lose excessive weight can produce up to 6 wet and dirty diapers a day. In addition, at this time, the Baby-Friendly Hospital Initiative has produced no data on the safety of newborn fasting and weight loss caused by exclusive colostrum feeding and what degree of weight loss protects a child from brain-threatening complications like hyperbilirubinemia, hypernatremic dehydration, and hypoglycemia. So far, the scientific literature shows that babies who lose greater than 7% of their birth weight are at the highest risk of developing excessive jaundice and hypernatremia to levels that can cause long-term developmental disability. It has also been found that 10% of healthy, term, exclusively breastfed babies undergoing the Baby-Friendly protocol experience hypoglycemia to levels that are associated with 50% declines in the ability to pass the literacy and math proficiency test at 10 years of age, even if aggressively corrected.
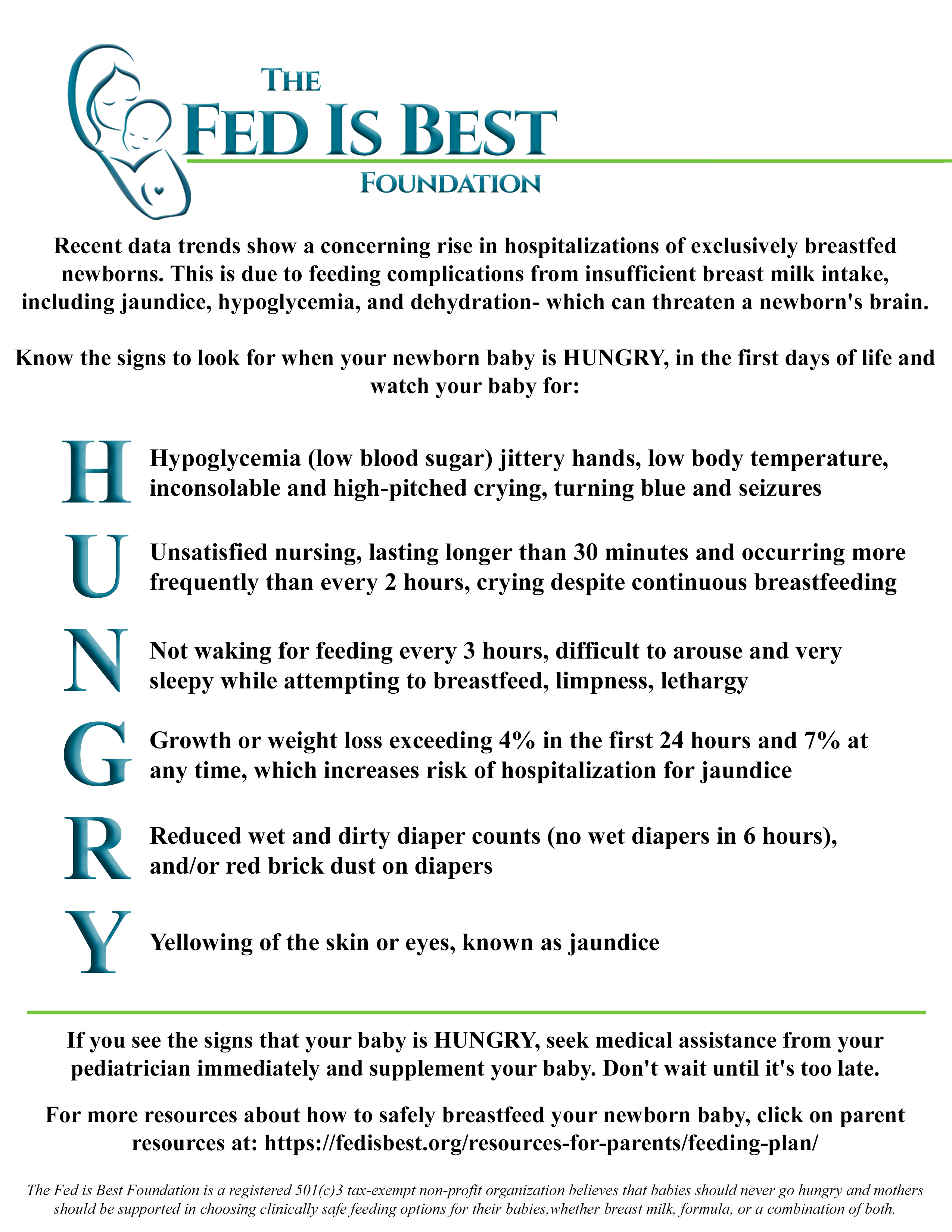
Constant, unsatisfied nursing and inconsolable crying are two of the signs of newborn starvation that lead to brain-threatening complications. If a child is receiving a fraction of their caloric requirement through early exclusive breastfeeding, they can experience severe hunger and thirst, which is why they will cry inconsolably and breastfeed continuously when it is the only source of calories and fluid they are offered. If a mother’s colostrum does not meet the child’s caloric requirement, they will breastfeed for hours a day in an attempt to relieve their hunger. A child who is “cluster-feeding” may actually burn more calories breastfeeding than they receive in return, which can result in fasting conditions and accelerated weight loss. The constant nursing and crying often found in newborns by the second day of life have been called“The Second Night Syndrome” in the breastfeeding industry. This is also whenmothers receive the most pressure to avoid supplementation in order to increase rates of exclusive breastfeeding at discharge. Babies who reach critically low levels of reserve fuel and fluids before their mother’s milk comes in can be found lethargic with compromised vital signs after hours of constant nursing and fussing, at which time they are often diagnosed with hypoglycemia, excessive weight loss, and/or hyperbilirubinemia, all markers of starvation.
Did you know that newborns aren’t supposed to cry all of the time? They’re supposed to eat and sleep and dirty their diapers. I had no idea he was inconsolable because he was literally starving. And when a baby is only on the breast, how do we gauge how much they’re actually getting out? Sure, there should be wet and soiled diapers and weight checks, right? And where is the limit as to weight loss and a minimum for the diapers changed?

Being discharged with visible weight loss.
Landon was discharged at 64 hours (2.5 days) of life having lost 9.7% of his birth weight continuously and exclusively breastfeeding with a mother whose milk had not come in. These are routine and unremarkable findings in newborn babies discharged home to exclusively breastfeed. At this time, there are no studies using standardized developmental testing or serum markers of starvation that show that allowing babies to lose up to 10% of their birth weight protects them from brain- and life-threatening complications, despite wide-spread perception that it is normal for exclusively breastfed babies to lose. Therefore, Landon’s mother was given no instruction to supplement. He was discharged with next-day follow-up.
So we took him home….not knowing that after less than 12 hours home with us, he would have gone into cardiac arrest caused by dehydration from unintended starvation because I was the mother who had no colostrum for my baby. The best advice I was given by one of his NICU doctors while he was on life support is that the breast is best, but follow with the bottle if they are still hungry.
This way you know your baby has eaten enough….if only I could go back in time.
Landon continued to breastfeed at home continuously and was found unresponsive, pulseless, and blue after eventually falling asleep from cluster feeding. His parents called 911. Per EMS, he was asystolic (no heart rate), and he received CPR en route to the local ER. By the time they arrived at the ER, he was found to have pulseless electrical activity (heart rate with no blood pressure). There, he was intubated and received several rounds of epinephrine. He was hypothermic with a temperature of 93.1 F. After 30 minutes of CPR, no cardiac activity was found on ultrasound. With parental consent, CPR was stopped, and he was left on the ventilator while continuing to receive IV saline. Twenty minutes later, with IV fluids, he regained his pulse. He was transferred to a Level III NICU to get the head cooling protocol for babies that experience a brain injury. He was diagnosed with hypernatremic dehydration and cardiac arrest from hypovolemic shock.

Landon is in the NICU on full life support.
I still have many, many days of guilt and questions – what if I had just given him a bottle? And anger because how would I have known? I trusted my healthcare professionals to protect my baby from harm. I remember when Stella, my daughter was born, and she was always quiet. I kept asking the nurses what was wrong with her. They said nothing. She’s doing what she’s supposed to. Sleeping and eating. And it was then that I realized that it wasn’t normal for a newborn to cry as much as Landon did. He was just crying out from his hunger. But I didn’t know. I should’ve known. I still struggle daily, feeling as though I failed him.
Landon received a brain MRI in the hospital which confirmed brain injury consistent with hypoxic-ischemic encephalopathy or brain injury from oxygen deprivation due to low blood pressure from dehydration and cardiac arrest. He was diagnosed with diffuse seizure activity on EEG, the consequence of severe, wide-spread brain injury. Given his poor prognosis, he was taken off life support 15 days later. The autopsy report deemed the causes of death were hypernatremic dehydration followed by cardiac arrest causing hypoxic-ischemic encephalopathy (diffuse brain injury).

Jill held Landon as he took his last breaths.
That little boy gave me ten of the most incredible life-changing months. I’ve been humbled. Challenged. My relationships have fallen apart. Some have come back together. I’ve learned forgiveness. And the true meaning of “life is short.” I love hard – to a fault. But I couldn’t live with myself knowing his death was in vain. I’ve learned so many lessons. I’ve learned the true meaning of compassion and unconditional love.
— Jillian Johnson
To Learn More About Ensuring SAfe and ADequate Feeding While Breastfeeding Your Newborn
Order the Fed Is Best book at all major retailers or by clicking on the button below. With it comes the Fed Is Best Book Resource Page, a free online guide to safe and adequate breastfeeding.
The Fed is Best Foundation is dedicated to the prevention of newborn and infant starvation from insufficient exclusive breastfeeding. We do so by studying breastfeeding stories sent by mothers and the scientific literature on breastfeeding complications that lead to infant brain injury and death. Since the beginning of our campaign almost two years ago, we have received tens of thousands of newborn and infant starvation stories leading to the complications of hyperbilirubinemia, dehydration, hypernatremia, hypoglycemia, and failure to thrive. These complications occur because the current breastfeeding guidelines have not been studied for safety and operate with little awareness of the caloric and fluid requirements of newborns nor the amount transferred to babies until complications have already occurred. “Just one bottle” can save a child from these tragedies as it is often a mother’s first clue that a child is, in fact, starving from exclusive breastfeeding.
If your baby is experiencing distress and signs and symptoms of starvation, we encourage you to advocate for your child. We encourage mothers to notify hospital administrators if they are pressured to avoid supplementation to alleviate their child’s hunger. You have the right to feed your child, and your child has the right to be fed. No one but your baby knows how close they are to empty. The only way they can communicate distress is by crying. Listen to your baby and listen to your instincts.
Our message is simple. Feed your baby. Feed them as much as they need to stay safe and satisfied.
How to supplement your baby until your milk comes in:
How To Prepare For Supplementing When Breastfeeding Your Baby In The Hospital
Jillian Johnson: My Message To Parents During World Breastfeeding Week-Just One Bottle
https://fedisbest.org/2022/01/nigerian-mother-speaks-out-about-her-babys-death-after-being-told-to-keep-exclusively-breastfeeding-what-she-wants-human-rights-organizations-to-know/
My Baby Suffered And Almost Died–Why Are The Risks Of Exclusive Breastfeeding Not Taught To Mothers?
Just One Bottle Would Have Prevented My Baby’s Permanent Brain Damage from Hypoglycemia
Feeding Your Baby—When Supplementing Saves Breastfeeding and Saves Lives
U.S. Study Shows Baby-Friendly Hospital Initiative Does Not Work
NICU Nurse Discloses Newborn Admission Rates From Breastfeeding Complications in BFHI Unit
Nurses Are Speaking Out About The Dangers Of The Baby-Friendly Health Initiative
https://fedisbest.org/2018/11/neonatal-nurse-practitioner-speaks-out-about-the-dangerous-and-deadly-practices-of-the-bfhi/
Hospital Drops Baby Friendly Program After Doctors Baby Was Harmed
Letter to Doctors and Parents About the Dangers of Insufficient Exclusive Breastfeeding
Two Physicians Describe How Their Baby-Friendly Hospital Put Their Newborn in Danger
I Supplemented My Baby Until My Milk Came In And We Are Still Breastfeeding At 3 Months
Fed is Best Statement to the USDA Regarding the Harms of the Baby-Friendly Hospital Initiative
Nurses Quit Because Of Horrific Experiences Working In Baby-Friendly Hospitals
Nurses Are Speaking Out About The Dangers Of The Baby-Friendly Health Initiative
“Is Baby-Friendly Safe?”: BFHI Safety Issues Discussed at National Neonatology Conference
CONTACT US/VOLUNTEER
THANK YOU FOR YOUR INTEREST IN THE FED IS BEST FOUNDATION!
Our mission statement is:
The Fed Is Best Foundation works to identify critical gaps in the current breastfeeding protocols, guidelines, and education programs and provides families and health professionals with the most up-to-date scientific research, education, and resources to practice safe infant feeding, with breast milk, formula or a combination of both.
Above all, we strive to eliminate infant feeding shaming and eliminate preventable hospitalizations for insufficient feeding complications while prioritizing perinatal mental health.
HOW YOU CAN SUPPORT FED IS BEST
There are many ways you can support the mission of the Fed is Best Foundation. Please consider contributing in the following ways:
- Join us in any of the Fed is Best volunteer and advocacy, groups. Clickhereto join our health care professionals group. We have: FIBF Advocacy Group, Research Group, Volunteer Group, Editing Group, Social Media Group, Legal Group, Marketing Group, Perinatal Mental Health Advocacy Group, Private Infant Feeding Support Group, Global Advocacy Group, and Fundraising Group. Please send an email to Jody@fedisbest.org if you are interested in joining any of our volunteer groups.
- If you need infant feeding support, we have a private support group–Join us here.
- If you or your baby were harmed from complications of insufficient breastfeeding please send a message tocontact@fedisbest.org
- Make adonationto the Fed is Best Foundation. We are using funds from donations to cover the cost of our website, our social media ads, our printing and mailing costs to reach health providers and hospitals. We do not accept donations from breast- or formula-feeding companies and 100% of your donations go toward these operational costs. All the work of the Foundation is achieved via the pro bono and volunteer work of its supporters.
- Sign our petition!Help us reach our policymakers,and drive change at a global level. Help us stand up for the lives of millions of infants who deserve a fighting chance. Sign theFed is Best Petition at Change.orgtoday, and share it with others.
- Share the stories and the message of theFed is Best Foundationthrough word-of-mouth, by posting on your social media page and by sending our FREE infant feeding educationalresourcesto expectant moms that you know. Share theFed is Best campaign letterwith everyone you know.
- Write a letter to your health providers and hospitals about the Fed is Best Foundation.Write to them about feeding complicationsyour child may have experienced.
- Print out ourletter to obstetric providersand mail them to your local obstetricians, midwives, family practitioners who provide obstetric care and hospitals.
- Write your local elected officialsabout what is happening to newborn babies in hospitals and ask for the legal protection of newborn babies from underfeeding and of mother’s rights to honest informed consent on the risks of insufficient feeding of breastfed babies.
- Send us your stories.Share with us your successes, your struggles and everything in between. Every story saves another child from experiencing the same and teaches another mom how to safely feed her baby. Every voice contributes to change.
- Send us messages of support.We work every single day to make infant feeding safe and supportive ofeverymother and child. Your messages of support keep us all going.
- Shop atAmazon Smileand Amazon donates to Fed Is Best Foundation.
Or simply send us a message to find out how you can help make a difference with new ideas!
For any urgent messages or questions about infant feeding, please do not leave a message on this page as it will not get to us immediately. Instead, please email christie@fedisbest.org.
Thank you and we look forward to hearing from you!

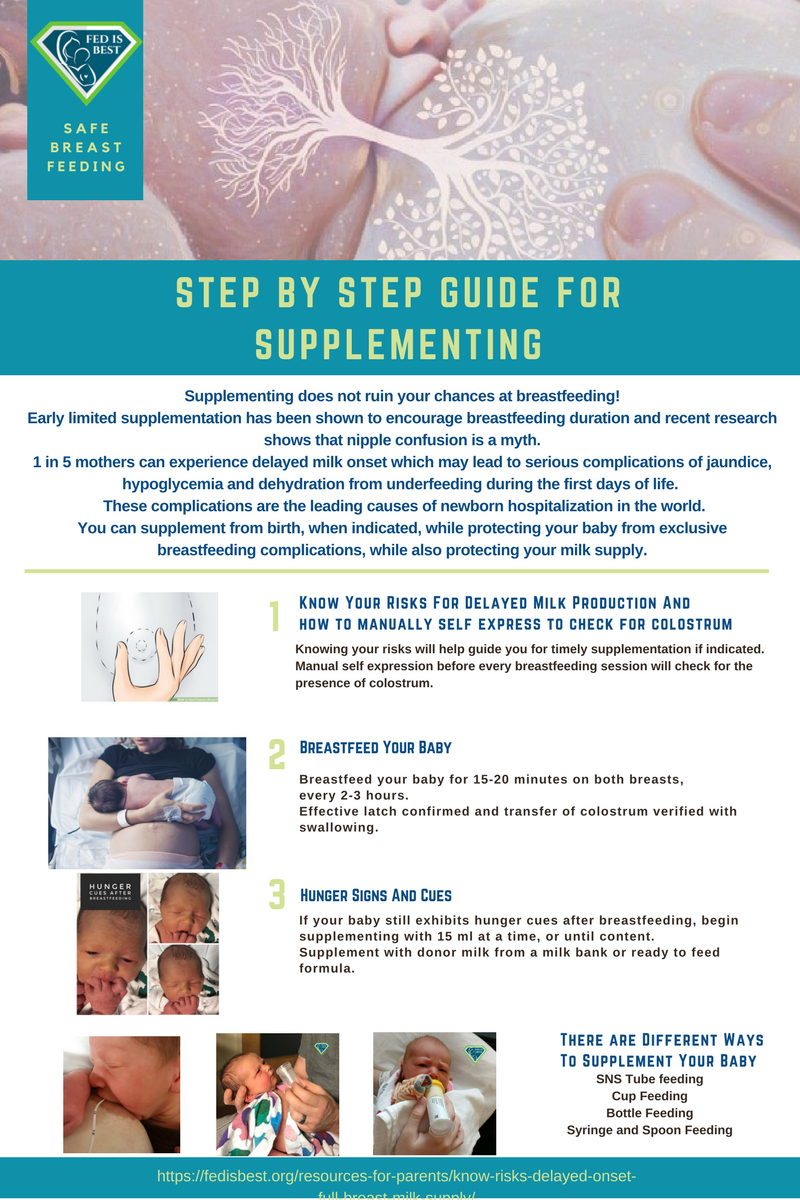
Parents tell us they were not taught how to supplement their babies safely, if necessary to prevent exclusive breastfeeding complications.
For more information on how to protect your baby from feeding complications due to early exclusive breastfeeding, please read and download the Fed is Best Feeding Plan, a way to communicate your feeding choices to your health care providers.
In addition, please read and download the Fed is Best Weighing Protocol to prevent newborn dehydration and failure to thrive.
Lastly, for more detailed information, please watch our educational videos onPreventing Feeding Complications.
Our full list of parent resources can be found on our Resource Page.
If you wish to help parents learn how to protect their newborns from accidental starvation, please share this story and sign our petition to demand that the CDC, the AAP, the U.S. Surgeon General and the WHO/UNICEF Baby-Friendly Hospital Initiative warn parents about the dangers of newborn and infant starvation from insufficient exclusive breastfeeding. Go to https://fedisbest.org/sign-our-petition/.
Please consider making a donation to the Fed is Best Foundation to support its mission of providing safe infant feeding education and support and raise awareness on the harms of insufficient infant feeding.
We believe all babies deserve to be protected from hunger and thirst every single day of their life and we believe that education on Safe Infant Feeding should be free. If you would like to make a donation to support the Fed is Best Foundation’s mission to teach every parent Safe Infant Feeding, please consider making a one-time or recurring donation to our organization.
Donate to Fed is BestThank you so much from the Founders of the Fed is Best Foundation!





yeah. That is impressive article because they have shown us exact point.
This is the saddest story about the saddest event possible. I am so sorry this happened to Landon and to you. When professionals, or any other people for that matter, embrace ideology beyond all semblance of common sense, that is unconscionable. Landon was their victim, as are you and the rest of your family. Yes, we want and support the best natural health for ourselves and our families that we can attain; sometimes we can’t attain it naturally, and then the cheering section needs to just let it go and let “us” do whatever works. I am so grieved by your devastating loss.
I am so sorry for your experience, as well. The US has abominable maternal/infant morbidity and mortality rates, and seems to have an official nationwide policy to discount anything women say about their own health.
My middle-aged daughter just experienced an extremely difficult pregnancy, was hospitalized midpoint with a high fever of unknown origin, and was even accused by one of the nurses of tampering with the thermometer for attention. (She had viral meningitis.)
In my own life, my complaints of frequent, heavy menses; severe pelvic pain, and low back pain were dismissed and called a psychiatric problem for 10 years, and when I had a medically necessary hysterectomy, 13 pounds of endometriosis and scar tissue were removed – so much for my severe pelvic pain and low back pain being a psychiatric problem.
There is so much surrounding women’s health that needs to change.
So many women have stories like these.
The horrible “numbers” the US experiences on maternal/infant morbidity and mortality and other aspects of women’s health need to be made alive with the truth of these stories and brought up front and center where they have to been heard and seen.
I am so very sorry you and your family had to experience this.
Impressive post. Very deep and informative article.
Thanks for sharing it!
I am so unbelievably heartbroken to hear of your loss. It’s very brave of you to tell your story and Landon’s. Thank you, this just as easily could have happened to me. One of my nurses asked how long I was feeding, I said an hour. She said thats too long no more than 30 mins, but she was always crying like she was hungry. I was also confused about the cluster feeding. We were discharged with weight loss 10% and they put us on formula supplementation and it turned out that orange was concentrated urine from dehydration. Things could have been much worse and things can happen so fast, especially with dehydration. I wish I could hug you. More people need to hear your and Landon’s story to spread awareness. Much Love ❤️
I am so sorry this happened to you and your sweet baby! I also had a hospital that pushed for breast only and sent us home. I had a lactation consultant come to the house who claimed everything was fine. Thankfully the state we were living in at the time required a nurse come to the home to check on babies 48 hours after going home. She was the one who realized we had a major problem. My baby had lost was too much weight. I wish more hospitals would inform new mom on how to properly feed their babies rather than them claiming all is well.
Praying for you today!