by Jillian Johnson with commentary from Dr. Christie del Castillo-Hegyi
Landon would be five today if he were still alive. It’s a very hard birthday–five. It’s a milestone birthday. Most kiddos would be starting kindergarten at this age. But not my little guy. I wanted to share for a long time about what happened to Landon, but I always feared what others would say and how I’d be judged. But I want people to know how much deeper the pain gets.
I share his story in hopes that no other family ever experiences the loss that we have.
Jarrod and I wanted what was best for Landon, as every parent does for their child. We took all of the classes. Bought and read all of the books. We were ready! Or so we thought….every class and book was geared toward breastfeeding and how it’s so important if you want a healthy child. Landon was born in a “Baby-Friendly” hospital. (What this means is everything is geared toward breastfeeding. Unless you’d had a breast augmentation or cancer or some serious medical reason as to why you couldn’t breastfeed, your baby would not be given formula unless the pediatrician wrote a prescription.)

Sleeping comfortably a few hours after birth
Landon was born full-term weighing 3360 g or 7 lbs. 7 oz, born by urgent cesarean due to fetal intolerance to labor after the water had broken. [Previous publication of this blog said he had an emergency c-section. He was delivered by low transverse incision over 12-14 minutes, which is considered an urgent, not a STAT section.] Apgars were 8 and 9 and he was stabilized. He was transferred 2.5 hours later to the Mother-Baby Unit and returned to his mother. He exclusively breastfed with excellent latch for 15 – 40 minutes every 1-2 hours.

Landon, is 12 hours old.
Landon was on my breast —ALL OF THE TIME. The lactation consultants would come in and see that “he had a great latch and was doing fine,” but there was one who mentioned I may have a problem producing milk. The reason she gave was that I was diagnosed with PCOS (polycystic ovarian syndrome), and it was just harder for women with hormone imbalances to produce milk. She recommended some herbs to take when I got out of the hospital.
While in the hospital, his mother’s risk factors for failed and delayed lactogenesis II (copious milk production) were identified by the IBCLC-lactation consultant. They were borderline diabetes, PCOS, issues with infertility, small, widely spaced breasts with minimal growth during pregnancy, being a first-time mom, and emergency c-section. Despite that, she was encouraged to exclusively breastfeed. She was closely monitored by a nurse, lactation consultant, and physician support. Her baby’s latch was rated as excellent.
By the first 24 hours, he had nursed a total of 9.3 hours, had zero wet diapers and four dirty diapers. By 27 hours, he had lost 4.76%. His nursing sessions became longer and longer until he was on the breast continuously by the second day of life. On the second day, he produced 3 wet diapers and 6 dirty diapers and nursed for almost 14 hours total. By 53 hours of life, he had lost 9.72%.
At this time, the scientific literature on wet and dirty diaper production has shown that the number of diapers produced have no correlation with adequacy of milk intake in the first 4 days of life. The only study on diaper counts has shown that even newborns who lose excessive weight can produce up to 6 wet and dirty diapers a day. In addition, at this time, the Baby-Friendly Hospital Initiative has produced no data on the safety of newborn fasting and weight loss caused by exclusive colostrum feeding and what degree of weight loss protects a child from brain-threatening complications like hyperbilirubinemia, hypernatremic dehydration, and hypoglycemia. So far, the scientific literature shows that babies who lose greater than 7% of their birth weight are at the highest risk of developing excessive jaundice and hypernatremia to levels that can cause long-term developmental disability. It has also been found that 10% of healthy, term, exclusively breastfed babies undergoing the Baby-Friendly protocol experience hypoglycemia to levels that are associated with 50% declines in the ability to pass the literacy and math proficiency test at 10 years of age, even if aggressively corrected.
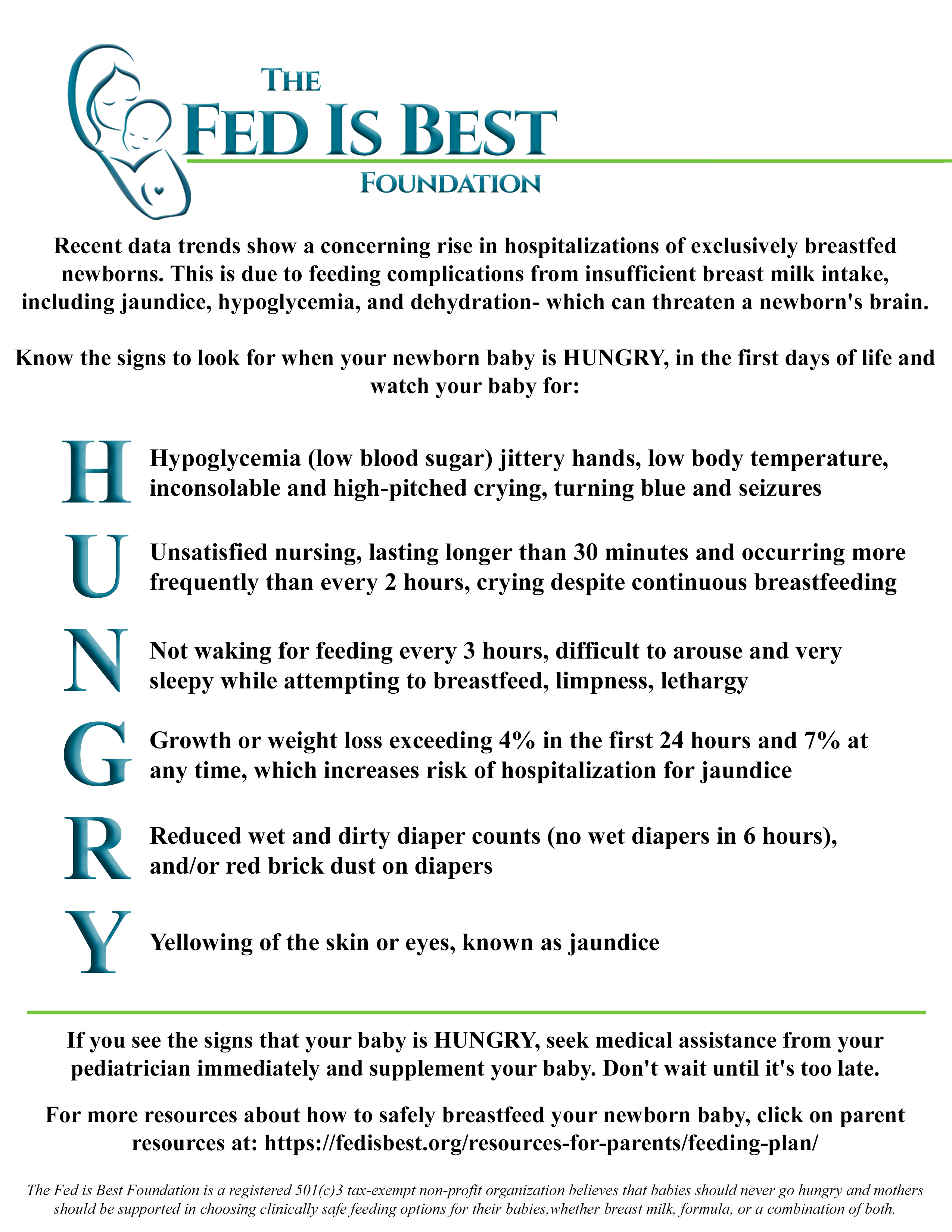
Constant, unsatisfied nursing and inconsolable crying are two of the signs of newborn starvation that lead to brain-threatening complications. If a child is receiving a fraction of their caloric requirement through early exclusive breastfeeding, they can experience severe hunger and thirst, which is why they will cry inconsolably and breastfeed continuously when it is the only source of calories and fluid they are offered. If a mother’s colostrum does not meet the child’s caloric requirement, they will breastfeed for hours a day in an attempt to relieve their hunger. A child who is “cluster-feeding” may actually burn more calories breastfeeding than they receive in return, which can result in fasting conditions and accelerated weight loss. The constant nursing and crying often found in newborns by the second day of life have been called“The Second Night Syndrome” in the breastfeeding industry. This is also whenmothers receive the most pressure to avoid supplementation in order to increase rates of exclusive breastfeeding at discharge. Babies who reach critically low levels of reserve fuel and fluids before their mother’s milk comes in can be found lethargic with compromised vital signs after hours of constant nursing and fussing, at which time they are often diagnosed with hypoglycemia, excessive weight loss, and/or hyperbilirubinemia, all markers of starvation.
Did you know that newborns aren’t supposed to cry all of the time? They’re supposed to eat and sleep and dirty their diapers. I had no idea he was inconsolable because he was literally starving. And when a baby is only on the breast, how do we gauge how much they’re actually getting out? Sure, there should be wet and soiled diapers and weight checks, right? And where is the limit as to weight loss and a minimum for the diapers changed?

Being discharged with visible weight loss.
Landon was discharged at 64 hours (2.5 days) of life having lost 9.7% of his birth weight continuously and exclusively breastfeeding with a mother whose milk had not come in. These are routine and unremarkable findings in newborn babies discharged home to exclusively breastfeed. At this time, there are no studies using standardized developmental testing or serum markers of starvation that show that allowing babies to lose up to 10% of their birth weight protects them from brain- and life-threatening complications, despite wide-spread perception that it is normal for exclusively breastfed babies to lose. Therefore, Landon’s mother was given no instruction to supplement. He was discharged with next-day follow-up.
So we took him home….not knowing that after less than 12 hours home with us, he would have gone into cardiac arrest caused by dehydration from unintended starvation because I was the mother who had no colostrum for my baby. The best advice I was given by one of his NICU doctors while he was on life support is that the breast is best, but follow with the bottle if they are still hungry.
This way you know your baby has eaten enough….if only I could go back in time.
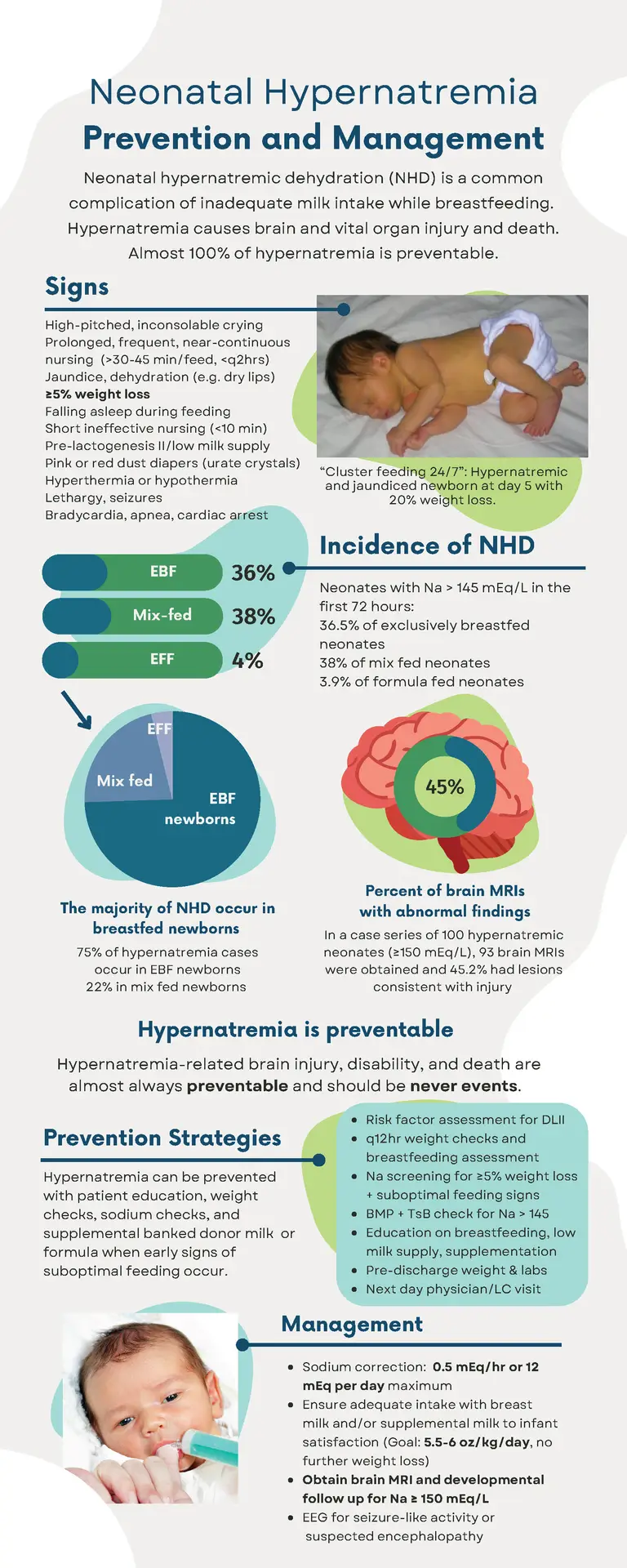
Landon continued to breastfeed at home continuously and was found unresponsive, pulseless, and blue after eventually falling asleep from cluster feeding. His parents called 911. Per EMS, he was asystolic (no heart rate), and he received CPR en route to the local ER. By the time they arrived at the ER, he was found to have pulseless electrical activity (heart rate with no blood pressure). There, he was intubated and received several rounds of epinephrine. He was hypothermic with a temperature of 93.1 F. After 30 minutes of CPR, no cardiac activity was found on ultrasound. With parental consent, CPR was stopped, and he was left on the ventilator while continuing to receive IV saline. Twenty minutes later, with IV fluids, he regained his pulse. He was transferred to a Level III NICU to get the head cooling protocol for babies that experience a brain injury. He was diagnosed with hypernatremic dehydration and cardiac arrest from hypovolemic shock.

Landon is in the NICU on full life support.
I still have many, many days of guilt and questions – what if I had just given him a bottle? And anger because how would I have known? I trusted my healthcare professionals to protect my baby from harm. I remember when Stella, my daughter was born, and she was always quiet. I kept asking the nurses what was wrong with her. They said nothing. She’s doing what she’s supposed to. Sleeping and eating. And it was then that I realized that it wasn’t normal for a newborn to cry as much as Landon did. He was just crying out from his hunger. But I didn’t know. I should’ve known. I still struggle daily, feeling as though I failed him.
Landon received a brain MRI in the hospital which confirmed brain injury consistent with hypoxic-ischemic encephalopathy or brain injury from oxygen deprivation due to low blood pressure from dehydration and cardiac arrest. He was diagnosed with diffuse seizure activity on EEG, the consequence of severe, wide-spread brain injury. Given his poor prognosis, he was taken off life support 15 days later. The autopsy report deemed the causes of death were hypernatremic dehydration followed by cardiac arrest causing hypoxic-ischemic encephalopathy (diffuse brain injury).

Jill held Landon as he took his last breaths.
That little boy gave me ten of the most incredible life-changing months. I’ve been humbled. Challenged. My relationships have fallen apart. Some have come back together. I’ve learned forgiveness. And the true meaning of “life is short.” I love hard – to a fault. But I couldn’t live with myself knowing his death was in vain. I’ve learned so many lessons. I’ve learned the true meaning of compassion and unconditional love.
— Jillian Johnson
To Learn More About Ensuring SAfe and ADequate Feeding While Breastfeeding Your Newborn
Order the Fed Is Best book at all major retailers or by clicking on the button below. With it comes the Fed Is Best Book Resource Page, a free online guide to safe and adequate breastfeeding.
The Fed is Best Foundation is dedicated to the prevention of newborn and infant starvation from insufficient exclusive breastfeeding. We do so by studying breastfeeding stories sent by mothers and the scientific literature on breastfeeding complications that lead to infant brain injury and death. Since the beginning of our campaign almost two years ago, we have received tens of thousands of newborn and infant starvation stories leading to the complications of hyperbilirubinemia, dehydration, hypernatremia, hypoglycemia, and failure to thrive. These complications occur because the current breastfeeding guidelines have not been studied for safety and operate with little awareness of the caloric and fluid requirements of newborns nor the amount transferred to babies until complications have already occurred. “Just one bottle” can save a child from these tragedies as it is often a mother’s first clue that a child is, in fact, starving from exclusive breastfeeding.
If your baby is experiencing distress and signs and symptoms of starvation, we encourage you to advocate for your child. We encourage mothers to notify hospital administrators if they are pressured to avoid supplementation to alleviate their child’s hunger. You have the right to feed your child, and your child has the right to be fed. No one but your baby knows how close they are to empty. The only way they can communicate distress is by crying. Listen to your baby and listen to your instincts.
Our message is simple. Feed your baby. Feed them as much as they need to stay safe and satisfied.
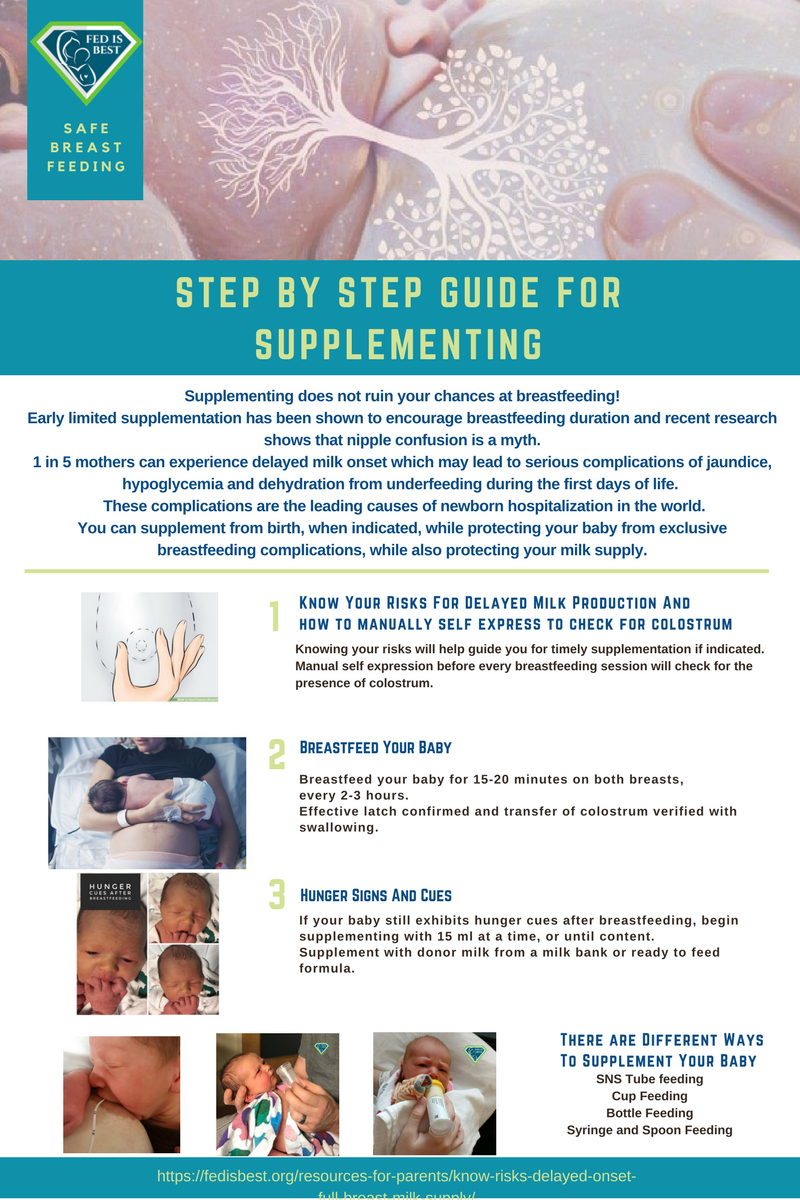
How to supplement your baby until your milk comes in:
How To Prepare For Supplementing When Breastfeeding Your Baby In The Hospital
Jillian Johnson: My Message To Parents During World Breastfeeding Week-Just One Bottle
http://fedisbest.org/2022/01/nigerian-mother-speaks-out-about-her-babys-death-after-being-told-to-keep-exclusively-breastfeeding-what-she-wants-human-rights-organizations-to-know/
My Baby Suffered And Almost Died–Why Are The Risks Of Exclusive Breastfeeding Not Taught To Mothers?
Just One Bottle Would Have Prevented My Baby’s Permanent Brain Damage from Hypoglycemia
Feeding Your Baby—When Supplementing Saves Breastfeeding and Saves Lives
U.S. Study Shows Baby-Friendly Hospital Initiative Does Not Work
NICU Nurse Discloses Newborn Admission Rates From Breastfeeding Complications in BFHI Unit
Nurses Are Speaking Out About The Dangers Of The Baby-Friendly Health Initiative
http://fedisbest.org/2018/11/neonatal-nurse-practitioner-speaks-out-about-the-dangerous-and-deadly-practices-of-the-bfhi/
Hospital Drops Baby Friendly Program After Doctors Baby Was Harmed
Letter to Doctors and Parents About the Dangers of Insufficient Exclusive Breastfeeding
Two Physicians Describe How Their Baby-Friendly Hospital Put Their Newborn in Danger
Fed is Best Statement to the USDA Regarding the Harms of the Baby-Friendly Hospital Initiative
Nurses Quit Because Of Horrific Experiences Working In Baby-Friendly Hospitals
Nurses Are Speaking Out About The Dangers Of The Baby-Friendly Health Initiative
“Is Baby-Friendly Safe?”: BFHI Safety Issues Discussed at National Neonatology Conference
CONTACT US/VOLUNTEER
THANK YOU FOR YOUR INTEREST IN THE FED IS BEST FOUNDATION!
Our mission statement is:
The Fed Is Best Foundation works to identify critical gaps in the current breastfeeding protocols, guidelines, and education programs and provides families and health professionals with the most up-to-date scientific research, education, and resources to practice safe infant feeding, with breast milk, formula or a combination of both.
Above all, we strive to eliminate infant feeding shaming and eliminate preventable hospitalizations for insufficient feeding complications while prioritizing perinatal mental health.
HOW YOU CAN SUPPORT FED IS BEST
There are many ways you can support the mission of the Fed is Best Foundation. Please consider contributing in the following ways:
- Join us in any of the Fed is Best volunteer and advocacy, groups. Click here to join our health care professionals group. We have: FIBF Advocacy Group, Research Group, Volunteer Group, Editing Group, Social Media Group, Legal Group, Marketing Group, Perinatal Mental Health Advocacy Group, Private Infant Feeding Support Group, Global Advocacy Group, and Fundraising Group. Please send an email to Jody@fedisbest.org if you are interested in joining any of our volunteer groups.
- If you need infant feeding support, we have a private support group– Join us here.
- If you or your baby were harmed from complications of insufficient breastfeeding please send a message to contact@fedisbest.org
- Make a donation to the Fed is Best Foundation. We are using funds from donations to cover the cost of our website, our social media ads, our printing and mailing costs to reach health providers and hospitals. We do not accept donations from breast- or formula-feeding companies and 100% of your donations go toward these operational costs. All the work of the Foundation is achieved via the pro bono and volunteer work of its supporters.
- Sign our petition! Help us reach our policymakers, and drive change at a global level. Help us stand up for the lives of millions of infants who deserve a fighting chance. Sign the Fed is Best Petition at Change.org today, and share it with others.
- Share the stories and the message of the Fed is Best Foundation through word-of-mouth, by posting on your social media page and by sending our FREE infant feeding educational resources to expectant moms that you know. Share the Fed is Best campaign letter with everyone you know.
- Write a letter to your health providers and hospitals about the Fed is Best Foundation. Write to them about feeding complications your child may have experienced.
- Print out our letter to obstetric providers and mail them to your local obstetricians, midwives, family practitioners who provide obstetric care and hospitals.
- Write your local elected officials about what is happening to newborn babies in hospitals and ask for the legal protection of newborn babies from underfeeding and of mother’s rights to honest informed consent on the risks of insufficient feeding of breastfed babies.
- Send us your stories. Share with us your successes, your struggles and everything in between. Every story saves another child from experiencing the same and teaches another mom how to safely feed her baby. Every voice contributes to change.
- Send us messages of support. We work every single day to make infant feeding safe and supportive of every mother and child. Your messages of support keep us all going.
- Shop at Amazon Smile and Amazon donates to Fed Is Best Foundation.
Or simply send us a message to find out how you can help make a difference with new ideas!
For any urgent messages or questions about infant feeding, please do not leave a message on this page as it will not get to us immediately. Instead, please email christie@fedisbest.org.
Thank you and we look forward to hearing from you!

Parents tell us they were not taught how to supplement their babies safely, if necessary to prevent exclusive breastfeeding complications.
For more information on how to protect your baby from feeding complications due to early exclusive breastfeeding, please read and download the Fed is Best Feeding Plan, a way to communicate your feeding choices to your health care providers.
In addition, please read and download the Fed is Best Weighing Protocol to prevent newborn dehydration and failure to thrive.
Lastly, for more detailed information, please watch our educational videos on Preventing Feeding Complications.
Our full list of parent resources can be found on our Resource Page.
If you wish to help parents learn how to protect their newborns from accidental starvation, please share this story and sign our petition to demand that the CDC, the AAP, the U.S. Surgeon General and the WHO/UNICEF Baby-Friendly Hospital Initiative warn parents about the dangers of newborn and infant starvation from insufficient exclusive breastfeeding. Go to http://fedisbest.org/sign-our-petition/.
Please consider making a donation to the Fed is Best Foundation to support its mission of providing safe infant feeding education and support and raise awareness on the harms of insufficient infant feeding.
We believe all babies deserve to be protected from hunger and thirst every single day of their life and we believe that education on Safe Infant Feeding should be free. If you would like to make a donation to support the Fed is Best Foundation’s mission to teach every parent Safe Infant Feeding, please consider making a one-time or recurring donation to our organization.
Donate to Fed is BestThank you so much from the Founders of the Fed is Best Foundation!




This is so sad! DD: I’m literally crying here in front of my display …
I heard some really hard stories about this “breastfeeding-trend”. I think it’s great when you do breastfeeding! But It’s not ok to force parents in this corner. As a doctor, you should help the parents decide what’s best for the kid. And I just can’t understand why no one noticed that the pretty guy was starving to death and therefore was crying for his life :((
I think I can feel happy because from beginning it was clear that I never would’ve been able to breastfeed, shouldn’t I? I had to feed formula on day 1. I used organic formula from and it worked. I think if you use a good formula, there are only very very little disadvantages from breastfeeding. I and my two siblings got only formula, too. And all of us were at university. People have to stop this “formula is so bad!”-opinion. It could save lifes.
I’m so sorry for your loss and want to thank you for sharing it.
I first read your story on the news while I was pregnant. I had no complications during pregnancy and delivered a healthy baby via vaginal birth and had chosen to breast feed. I am a first time Mom, also. I was a bit inexperienced about the baby’s hunger cues at first so I may have not been aware of when to feed or the importance of proper feeding time. Silly, as it sounds I thought baby would cry when hungry when that is actually when they are starving.
By second day, I felt I was feeding baby for several hours at a time and taking barely any breaks because baby was crying non-stop. Baby would not sleep or rest so I didn’t get much either.
There were signs that something didn’t feel right to me. Like, I visited other babies when they were delivered and they seemed calm and didn’t cry. Also, my baby’s lips were so smooth after delivery that I noticed the wrinkles when they appeared, but couldn’t pinpoint the cause was probably dehydration. Same with my baby’s eyes, they would barely open and only open one at a time. It was peculiar because at birth, I remember my baby’s blinking eyes staring at me. Finally, I remember one of the technician commenting that every time they came in the room, baby was always on my breast.
We were discharged 3 days later. We were kept an extra day because my baby’s bilirubin levels were high and needed phototherapy. Baby lost over 10% body weight. Before leaving, I asked for formulas and tips on it in case I had trouble producing milk. I was told the same thing, milk would come in and colostrum is fine. Went home and tested out the pump, saw very little milk. I felt sad for my baby that I knew my supply was inadequate. Remembering this site, I gave him a bottle. Baby slept. Next day, pediatrician phoned me and told me to supplement with a bottle. I’m glad I trusted my instinct.
Reading this story that Jillian so bravely shared makes me think back to our now 4 year old son. Her story and ours were nearly identical with different outcomes. Our little guy ended up in cardiac arrest, was rushed to a local hospital and transferred to St. Louis Children’s hospital. Those amazing people helped save our son. As a new mom, I had no idea I was not feeding him. We talked to many nurses and lactation consultants and all of them said we were doing what we were supposed to be doing. I blame no-one, but I wish there was a way to communicate this to(especially) new moms without scarring them. I am so thankful Jillian is sharing her story…I hope it can help others going forward.
Let me first start out saying I’m sorry for your loss no mother should ever go through something like that. I’m due in a couple of months and I was wondering what hospital was this at so I know to protest and throw it fit if they want to send me there. Because I don’t think you did anything wrong this is like you said this is your first baby and you were just doing with the hospital told you to there to blame for your baby’s death not you.
Yes the drs should be responsible for what happened. I don’t see how they did not see the baby was dehydrating or losing too much weight. When I had my daughter the nurse and drs came in at all hours to check both me andy.baby. at that point I did give only breast milk but at at time it might have been enough. A couple days after being released she did lose just a little (2 oz) more then they wanted. She was still In the right weight range but she needs to gain more. The Dr said either supplement or pump to know how much she’s eating. A couple days later they weighed her n she gained it. And I do t even think I had lunch w supply. Do I do that know why nobody knew. I would think in first couple days the small amount of colosyrom is what they need but if not I would think the nurses would see and give baby needed formula. Anyway a sad story.
Unfortunately, colostrum is not enough for many babies. Also, for many moms, they do not produce enough colostrum. That is why we advocate for newborns who are crying and nursing non-stop, showing signs of dissatisfaction with breastfeeding, that they be offered supplementation. Only babies know how much they need to keep from starving. Avoiding supplementation in a baby who showing obvious signs of hunger and starvation is gambling with childrens’ lives and futures. Complications that result in brain injury from insufficient feeding of breastfed newborns happen every single day, which is the reason why our Foundation exists.
I am so sorry about your loss and thank you so much for sharing your story . You are such a strong woman and mum. I went through the same thing after my son was born except we were lucky enough to spot urin crystal on his diaper so took him to A&E on the same night as he was discharged.
He had tongue tie so while we were in the hospital he wasn’t taking in milk from the 2nd day he started to cry non stop and we were told he was fine and loads of wet diapers.
By the time we took him to A&E he lost 12% weight already. We live in Singapore and I delivered in one of the most expensive hospitals here, almost all hospitals here are claimed to be prob natural, breast feeding etc. but we were absolutely shocked that nobody had the knowledge to address his tongue tie issue and when he cries they simply said babies cry.
I absolutely support this blog and I have shared this article on the hospital’s facebook page and hope this can draw some attention. My son now has been having formula top ups and he is a very happy baby. He was born big so I m totally fine that my milk is a little short for his appetite but while we were in the hospital nobody ever mentioned to us that formula might be considered if my milk wasn’t enough. As first time parents were thought feeding a baby would be a simple thing..
I would be more than happy to help get in touch with the hospital if it’s needed.
Thank you Jillian for calling out the ‘Breast is best’ campaign. Anne Diamond pioneered the “Back to Sleep” campaign in the 60/70s which has saved thousands of lives a year since and saved the most lives of any single piece of medical research in recent history. I have no doubt that you will help save thousands of lives too.
My experienced something similar. My son from the moment he was born found it difficult to latch and when he eventually did latch I was told he’s latching fine don’t be so anxious but I knew something wernt right. I stayed 24 hours in hospital after birth and during that time I asked four Midwife’s to watch me feed, each of them all said he’s latching fine but still I knew and felt something was wrong with his feeding. Anyways fast forward going home, feeding became incredibly painful (cracked, bleeding and sore nipples) feeding constantly, he never seemed satisfied and would always cry after every feed. Then in one crying session I noticed his tongue and found that he had a tongue tie. I told my Midwife and she didn’t believe me she sent me to a lactating consultant and when I tried to show her pictures that I had taken she refused to see them instead she made me practice latching him on in front of her. 3 weeks later baby was still unhappy feeding I was exhausted, nipples were sore my husband begged me to give a bottle (which I did) I then got seen my another Midwife shortly afterwards who examined him finally and saw his tongue and referred me to have the procedure straight away. It was a terrible and anxious three weeks, I was made to feel like I just wasn’t trying hard enough with the breastfeeding and that as long as I got the latch right, that he was feeding ok. What I’ve realised and my advice to anyone is that you know your baby best. Do not be pressured into feeling guilty for supplementing or giving up breastfeeding… a fed and happy baby is the number 1 priority regardless of whether it’s by breast or bottle.
Thank you for sharing your most personal experience. My heart goes out to you and Landon. Trust in God plan and remain strong. Stella is counting on you.
Yes thank you for sharing you brave, wonderful woman. My heart breaks for your loss.
Im so sorry and I really feel for your loss as I experiencing something similar.
We are first time parents and we lost our child. I gave birth last January 18, 2018, Thursday at 2:14pm (Philippine time) under c section. My baby was at 36 4/7 weeks, he weigh 2.2 kg. The doctor said that he was healthy and scored 9 in the apgar. At around past 6:30 pm i was moved to our private room and shortly after they room-in our baby with me. The lactation nurse instructed us to breastfeed but i cannot see any milk coming from my breast. She told us its fine only the baby could see or feel or taste the milk of course we listened and believe. Friday night our baby was crying hard, irritated and inconsolable. Me, my husband and my mother in law panicked and so worried that maybe he really wasn’t getting any milk from me. We called the nurses every now and then but still instructed us to breastfeed. I asked if we can have formula instead and they refuse still insisted breastfeeding. Their accreditation/certification might be put into jeopardized. I told them i already tried using electric breast pump but still i cant see any milk coming out from my breast. They still insist of breastfeeding and told us that baby stomach is so tiny and as long as he is pooping means he is getting milk from me. He pooped 3 times that friday night all his poop was color black. We thought that he might really eating because he pooped. Come saturday my baby is always sleeping we thaught it was normal for a newborn. I still breastfeed him every now and then but still not sure if I’m producing any milk as i could not see it. The nurses and resident doctors have their usual rounds to see us and always saying thay me and baby are ok. Saturday at around 10pm or past 10pm my mother in law noticed that my baby heartbeat was slow and told my husband. My husband carried our baby and notice that our baby’s skin is getting darker. We called the nurse but my husband couldn’t wait for the nurse to come. He ran carrying our baby to the NICU which is located at same floor of our room. There they resucitate, iv him and etc. He was revived but still he can not breathe on his own. The pedia told us that there is a slim chance he will survive.(lack of oxygen and etc.) I was crying all night. Sunday morning he was moved to incubator but still with life support, etc. They told us they need to reintubate him. Sunday, January 21, 2018 11:07 am (Philippine time) he passed away. The death certificate stated that the cause of death was SIDS. Monday, January 22, 2018 after we attended our son’s burial we came home, I went to the bathroom to change and that was the only time I see myself lactate I called my husband for him to see and we couldn’t do anything else we just cried. Those events were so traumatizing to us and all those events happened while me and my baby are still inside the hospital.
Am speechless. My cheeks are wet and whilst typing this I feel yet another tear filling my eyes. I just read your story and halfway through I stopped reading because I didn’t want to actually read the words to come in the next line. I took a breath and decided to continue reading. To be (at least) brave enough to ‘face’ the words and let the emotions behind them hit me…
I realised how close my son and me came. I remembered how I (with hestitation and sleep deprivation) decided after two days that he needed to eat (and that I needed to sleep) and ‘asked’ for formula. So that we could try breastfeeding again tomorrow. We tried, he tried, o yes, he tried. After ten days of struggling ( During those days I was a mummy-cow: every hour and a half it was either a baby or a pump, he also got the occasional formula to provide the energy he needed to try stimulate my production ), he kept losing weight and wouldn’t wake on his own because he was hungry, I was told that my production was most likely without nutriciens. So I switched to formula and gave up breastfeeding by one last session to imprint the experience. I cried and smiled while he – quite satisfied because he just had a bottle – took in the ‘empty’ milk for the very last time.
Thank you for making me realise how lucky we were (and are).
Thank you for being so brave to share!
Thank you for making me humble!
———————————————-
I’ve also read many of the replies here. I am so surprised by all the stories about hospitals and midwifes who refuse to grant a mothers wish by not allowing formula! I was trying to figure out in what part of the world this actually happens in the present days after the first few of similar replies. Then I realised that all replies are in English and that there were to many to only come from the UK. Meaning it most probably are stories from the USA. ( Im still not sure and I am not yet able to believe that the knowledge of medical professionals lacks such crucial information.)
I didnt know any better than that my case was an well monitored exception with the main rule that the parents make the decisions after explanation by the medical staff about their options.
I am from the Netherlands and know no better that the patient always decides and never the medical staff.
I was also shocked to read that formula has a negative reputation and must therefor be avoided ( at all costs?!) I think I remember reading that giving formula to a baby will make him less smart…
How come that people still believe this is true/proven etc?
And even if it were true: I would rather have a living ignorant child than the alternative.
———————————————-
Jillian, to me you and! your son are heroes. I hope you are a hero to you as well.
Thank you so much for sharing your story. This breaks my heart in so many ways. I had a similar situation in that I wasn’t producing enough and my little guy wasn’t getting enough. He cried endlessly those first few days and I didn’t know what to do for him. He was “feeding” round the clock, but inconsolable. I am so thankful I brought him in to the pediatrician’s office by day 4. He lost a little over 10% of his birth weight and she immediately gave me a bottle to feed him. No one at the hospital even suggested that or told me it was okay. I look back now and can’t believe it never really occurred to me to supplement. I just didn’t know. I’m so sorry that your situation ended up in the loss of your beautiful boy. But thank you for sharing. I hope no other mother has to experience such a tragic loss like this. Thoughts, prayers, and love to you and your family.
Thank you for sharing. Thank Gid for internet and having 2 girls breastfed with no problem or my 3 year old son would be too. I gave him a bottle at 1 week check up and he was fine. I produced plenty of milk but when I looked up types of cries his was a pronounced different then I had ever known a weak yell out(from hunger). He was starving due to my having no fat content. I only gained 15 lbs. Pregnant with him and lost all plus within 2 days of his birth. I was eating 2000 in healthy food along with McDonald’s it was not enough to support us both. After 1 week he was starving at day 6 I knew it. The nurse at 1 week check up told me to give bottle extra. I had 2 girls I breast fed perfect til thet were 2 heavy. I gave him a baba and never even tried a breast again. He slept did not cry anymore and gained all weight back in 3 days. I knew he was about to die. I am so so sorry for your loss. I was experienced with plenty of breast support people and I just got flipping lucky. Please don’t blame yourself. You sound like a wonderful mommy I hope you go have a bunch more babies. It will not bring him back but your sharing this experience may save 1000s of little guys. If I would have read this before I had him. It wouldn’t have taken so long for me to try a bottle. Also the doctors never knew abiut my fat content in milk. I pumped milk last day and when I went to get it out of fridge it 6 hours later there was no seperate layers No Fat on top. My ❤ to you. Prayers and thoughts forevermore. Thank you I hope you know how many children you are saving by sharing.
I just read CHRISTIE DEL CASTILLO-HEGYI MD reply to someone else’s comment. it is perfect and is what really needs to be addressed!!!
I have posted it on my website and have shared it on social media.
This is where the issue is!!!
“Unfortunately, colostrum is not enough for many babies. Also, for many moms, they do not produce enough colostrum. That is why we advocate for newborns who are crying and nursing non-stop, showing signs of dissatisfaction with breastfeeding, that they be offered supplementation. Only babies know how much they need to keep from starving. Avoiding supplementation in a baby who showing obvious signs of hunger and starvation is gambling with childrens’ lives and futures. Complications that result in brain injury from insufficient feeding of breastfed newborns happen every single day, which is the reason why our Foundation exists”
This answers the anxieties in my previous comment. instead of saying things like “exclusively breastfeeding kills” or “supplement if baby cries” or “if they appear hungry within 2 hours of previous feed then supplement
supplementing will further limit supply UNLESS there is an underlying condition- baby tongue tie/latch/ mothers milk supply due to health issue or illness.
In the majority of cases, women can breastfeed exclusively if many factors are on her side.
If you feel your baby is starving- YOU NEED TO GIVE THEM A BOTTLE.
it does not matter how pro-breastfeeding you are, you can address this once the baby is a little more contented. if babies are losing 10-15% and becoming jaundice it is usually because they are not fed enough colostrum- this could be due to insufficient latch or not enough tie at the breast OR it could be an underlying cause!
this is what we need to target- the underlying cause! what puts women at risk of low milk supply! how to spot the signs!
poor lady was really failed by health professionals. they have made a rod for their own backs. trying to push breastfeeding on women who have a genuine supply issue!!! the putting women off breastfeeding all together!
If I can give one bit of advice for mothers who are breastfeeding is- keep them on your breast for as long as possible! for me, this was the case, my daughter sucked me for hours and hours on end in the first week. (I must have had natural low milk supply in early days).
However, if still your baby is inconsolable, despite hours of endless sucking…theres something up.
Thank you so much for sharing. While Reading this I realized that things could have been so much worse for my babyboy. I was also exclusively breastfeeding. And I knew that he was not eating, but nurses wouldn’t really listen. At home I also bottle fed him, but only small amounts. ‘Luckily’ my boy turned quite yellow on day three. So we went back to the hospital where they told me; A baby this size should be eating much more! They doubled his milk and put him under A blue light. Thank god we could take him home healthy after A week!
Hi Jillian,
I believe it has been at least 5 maybe 6 years since you lost your sweet boy Landon. I am so sorry for your loss. I want to let you know that I do believe your story saved my little boys life this April 2018. That Landon’s story is still impacting new babies and their families.
I brought my little boy home from the hospital 2 days after a cesarean birth, with little to no wet diaper production and no sign of milk coming in. They kept telling me, “it’ll eventually come in, just keep feeding”. I was apprehensive as I’d had a susbstantial breast reduction years prior and my breasts just didn’t seem to change at all during pregnancy and after birth. My son was crying constantly and rarely sleeping immediately following birth and by his 1 week check up had lost 11% of his birthweight. I just knew with my instincts that something was not right, but like you thought I needed to exclusively breast feed my dear son. That night we got home from his first pediatrician visit where they told me it was a normal weight loss and to keep breastfeeding, and after feeding him on the breast every hour all day and an hour straight for the last entire hour, he was still crying every time I’d try to put him down. Finally I began researching his symptoms online and came across Landon’s story. That’s when I decided to do something that may have saved his life.
Your brave choice to share Landons story prompted me to prepare a 3 oz bottle of formula that night. He drank it so quickly and soon after began to relax for the first time since his birth. He slept for 2 hours for the first time since his birth and that was when I knew for certain my poor baby boy had been starving all week. After that I vowed to feed my boy if he was hungry no matter what. He is now two months old, and since that revelation, I breast feed him 8-12 times a day for 30-40 minutes and always need to give him a bottle of formula afterward with 1-4 ounces in order to satisfy his hunger. You see, even after all the breastfeeding (and constant pumping when I’m not breastfeeding) my milk still hasn’t fully ‘come in’ as all the lactation specialists, doctors and midwives told me it would.
I want to thank you for sharing Landon’s story because I do think that by my finding it online that night, you and Landon helped save the life of my baby boy. You and Landon are true angels.
tragedy.. thanks for sharing your story
Jillian I hope you can read this…it’s 2020 and I happened to stumble onto your article. First and foremost you are one courageous soul. Women can often be reluctant to share our most vulnerable sides because of that feeling of failure and guilt. Social media often portrays perfect scenarios of everyone’s life…but hopefully we all know…reality vs fantasy. I am a grandmother to 9 blessed young ones, I raised 5 children whow are wonderful kind beings…but we lost our first little girl Heather…she was stillborn. I had a healthy pregnancy with no complications. The day we came into the hospital when I was in labor was July 2nd. At first the fetal monitor I was hooked up to seemed to be working fine…then I saw the numbers bounce around. The 2 nurses who cared for me told me the machine wasn’t working properly…they finally brought in another machine…now an hour later…that one did the same thing. I got very worried and asked for the Dr right away. I was told because I was a first time mom…this Dr doesn’t need to come in until I’m at 8 cm. I begged them to manually check my baby with their stethescope…I told them I feel somethings wrong with my baby…they told me the Dr would be here shortly. Nobody seemed eager to help manage the situation. The Dr on call finally arrived and did an internal fetal monitor. Then he put a gloved hand inside out came greenish stool. Then he listened with his stethescope and in the most cold manner spoke the words. “I believe your baby is dead. I am ordering an xray for confirmation.” My Heather would be 43 today but sadly she never got to see her mommy’s happy smile and we never saw hers…thank god a different older nurse came in and asked what we named her and then asked me if I wanted to hold Heather. She was the only person in that hospital experience that showed compassion and kindness. The Dr never uttered a single word of consolation…and we never saw those 2 nurses again. When the nurse brought our baby to me she had tears in her eyes and said “she’s a sleeping angel…and so beautiful.” My husband baptized our daughter as tears ran down his face. It changed everything about our perspective on life. That horrible experience taught me to take a firm loud stand as my children’s advocate and never back down. God blessed us with a beautiful family, and every July 2nd we celebrate Heathers life and her gift of a parents love.
I’m so sorry for loss. This is one of the saddest stories I’ve read. I truly cried and I’m truly heartbroken for you and pray you have peace at this time. May your Landon forever be with you. A mother’s instinct is the purest form of alarm. I am a new mom, with a beautiful daughter and I have learned to listen to my instincts more than anything. Thank you for sharing.
Sadly, this crap is still happening in 2020. I just had my beautiful baby boy 3 weeks ago via c-section. I knew for a fact that I was not producing any milk. My breast started leaking at 28 weeks and then stopped so I knew what it felt like to produce milk. They forced my baby on my breast. I told them that he was not getting any milk and the nurse said, “Yes, he is!! You need to just relax and trust the process. He is definitely drinking your breastmilk right now.” After telling another nurse once again that my baby is not getting any milk, I finally requested a bottle of formula. I had to ask 3 times before someone brought me one. When he finished that bottle, I asked for another one for his next feeding. The nurse then gave me a strange and judgmental look and started telling me about WIC and how I can sign up if I need more milk. Me and my partner make more than enough money to take care of our baby so me asking for formula had absolutely nothing to do with my ability or inability to purchase formula. The nurses have all been terrible! If I would’ve listened to them and believed that he was drinking breast milk when he wasn’t, my baby boy might not have made it either.
Dear Angie,
We are so saddened to learn about your experiences with your baby. How are you both doing now? We have a Facebook support group to join if you are interested. Take good care.
Felt so emotional when I read about your loss. So sorry
https://tinytwig.com.au/