Jody Segrave-Daly, RN, MS, IBCLC
Mothers are taught that it’s rare not to produce enough milk to exclusively breastfeed in nearly every breastfeeding book, mommy group, and hospital breastfeeding class. The truth is we have limited studies that provide an accurate percentage of mothers who can produce enough milk for their babies for the recommended six months. Although actual rates of adequatemilk productionare unknown, some estimates range from 12-15 percent or more.
- Dr. Marianne Neifert, Clinical Professor of Pediatrics at theUniversity of Colorado Denver School of Medicine, co-authored a 1990 study of 319 breastfeeding women and found that 15 percent of the women could notproduce sufficient milk by three weeks after delivery.
- Data from the Infant Feeding PracticesStudy (IFPS) II, a study of U.S. women, showed that one in eight women experienced early, undesired weaning from disrupted lactation due to physiologic reasons. According to the study, pain, difficulty with latch, and insufficient breast milk supply were the most common reasons for early weaning.
- Dr. Shannon Kelleher talks about these staggering numbers in herpublication, “Biological underpinnings of breastfeeding challenges: the role of genetics, diet, and environment on lactation physiology,†where she says the prevalence of lactation insufficiency may be much higher, as 40–50% of women in the US and 60–90% of women internationally cite “not producing enough milk†or that their baby was “not satisfied with breast milk†as the primary reasons for weaning before six months.
- We are learning that mothers in Western societies are experiencing delayed lactogenesis II (onset of full milk production) for complex and unknown reasons. This studysuggests that the prevalence of DOL has reached epidemic proportions.
In my 32 years of experience working clinically with moms and babies in the NICU as a registered nurse and an IBCLC in private practice, I have seen vast differences in colostrum and milk production. The WHO 10 Steps to Successful Breastfeeding and its counterpart, The Baby-Friendly Hospital Initiation, were implemented in hospitals’ maternity departments to help increase breastfeeding initiation because of the known benefits for both the mother and baby.The goal is to promote exclusive breastfeeding for the first six months of life. All mothers are taught about breastfeeding benefits and how to breastfeed exclusivelyduring their hospital stay. The breastfeeding initiation rate is higher now than ever, but the complications from inadequate colostrum intake and low breast milk production are now rapidly emerging!
Exclusive breastfeeding at discharge from the hospital is likely the single greatest risk factor for hospital readmissionin newborns.
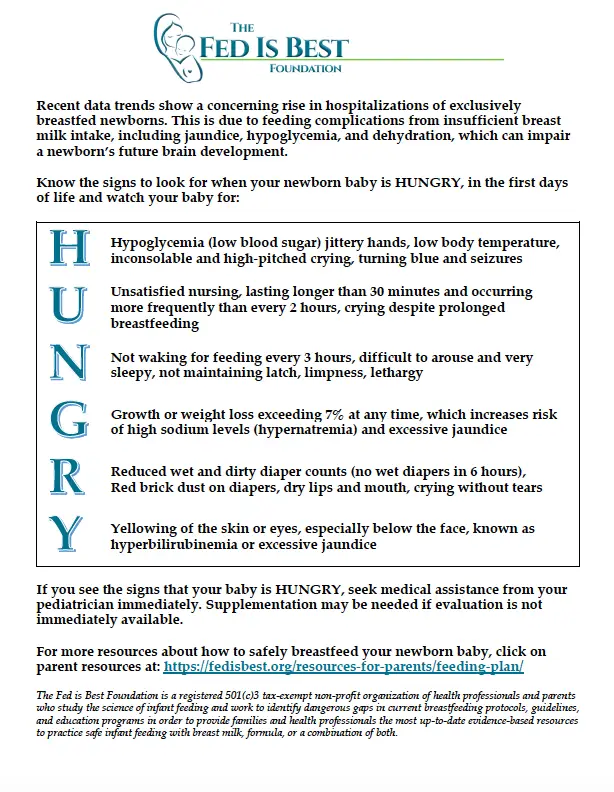
These readmissions are due to hyperbilirubinemia, dehydration, hypernatremia, and hypoglycemia from inadequate breast milk intake and have very serious risks, sometimes long-term disability and, rarely, death. Ironically, inadequate intake can be prevented with temporary supplemental nutrition, so why are babies suffering from unintended starvation?
For every 77 babies breastfed, 1 is readmitted to the hospital for hyperbilirubinemia, dehydration, hypernatremia, or weight loss.
In my daily practice, I commonly see underfed babies who have been discharged from the hospital with little to no intake and sometimes under the guidance of previous lactation consultants. I have seen an acceptance of persistent infant hunger and poor growth to protect and achieve exclusive breastfeeding ‘status,’ especially among avid breastfeeding advocates. I have had to refer many of these malnourished babies for admission to the hospital for rescue feeding and treatment for jaundice, dehydration, hypoglycemia, and/or hypernatremia. I believe some healthcare professionals and LCs are overly focused on protecting the exclusive breastfeeding relationship rather than protecting the baby from inadequate breast milk intake.
‘Successful breastfeeding management protects the baby from hunger, optimizes milk supply, protects the parents breastfeeding goals, while supporting optimal maternal mental health.’
~Jody Segrave-Daly
Anna
Anna contacted me to help her breastfeed her second baby. Her first baby struggled to gain weight despite seeing multiple IBCLCs and spending over $1,000 for services. He didn’t gain enough weight, was malnourished, and Anna became profoundly exhausted from pumping after every nursing. Anna’s baby experienced the common occurrence of not being the priority. Anna’s mental and physical healthwas also not a priority.
In order for the baby to receive the full benefits of breast-milk, adequate and safe feeding must be the number one priority, every time.
With her second baby, we reviewed all of her risk factors prenatally and created a flexible feeding plan that would adequately feed her baby. I provided Anna with a realistic feeding and pumping schedule that would accommodate caring for a toddler while maximizing her time for rest. Her overall goal was to breastfeed while ensuring her baby was well fedthis time so she could be present and enjoy the first weeks of having a newborn that she missed with her first baby.
Our contact began right after delivery, and she followed the breastfeeding plan that we created. After delivery, we talked multiple times a day as she needed guidance. She experienced a delayed onset of milk again, arriving on day five, but wanted her baby to be supplemented on the first day to avoid the unintended starvation that her first baby experienced. She continued to nurse, self-express, and power pump to maximize her milk production. The first weeks at home required multiple contacts daily, and she supplemented until her full milk supply was in. She had many bumps along the way, but we quickly tweaked her feeding plan to help her cope so she could continue breastfeeding. Her full milk supply was in at three weeks, and she could breastfeed with occasional supplementation.

Left, the first baby, exclusively breastfed, malnourished and underweight at one month. Right, the second baby supplemented after nursing from birth until three weeks, safely fed and thriving at one month.
What we know
Failed lactogenesis ll, known as the onset of breast milk ‘coming in,’ can be for three reasons.
- First, a maternal biological reason interferes with adequate milk production.
- Second, multiple reasons can hinder effective sucking and removal of breast milk by the baby.
- Third, there can be a combination of maternal and newborn reasons and improper breastfeeding management.
Fortunately, most moms do make enough milk to feed their babies adequately. Still, the estimated 12-15% of mothers who don’t are often in shock and disbelief when they realize they are not making enough milk to feed their babies fully. It breaks my heart whenever I have to tell a mother her baby is hungry and needs immediate rescue supplementation after they were instructed to keep breastfeeding. They are commonly told to avoid supplementation despite their baby displaying signs of persistent hunger. Their guttural cries motivate me to continue teaching families about #SafeBreastfeeding.
Tonya
Tonya contacted me because her 6-week-old baby was very sleepy and was not waking up to feed. She was an experienced breastfeeding mom of two and thought he was just a really good baby. She thought he looked small, but everyone kept telling her not to worry as he was long. She panicked when she weighed him at home when he was a full pound under his birth weight at six weeks. She wanted to continue to breastfeed but needed help. After talking with her pediatrician, she contacted me, and we safely began to supplement after every nursing. Her milk supply was very low and was just enough to keep her baby hydrated for the first six weeks.

Left, Her baby was one pound below birth weight at six weeks. Right, gained 7 ounces in 2 days from supplementing.
Supplementing an underfed baby will provide enough calories and fluids to increase alertness and the strength to nurse effectively. Why? Babies who are being underfed will become very sleepy and sometimes lethargic as they are shutting down to conserve energy and calories. Even the smallest amountsof supplementation will help the baby have enough energy to nurse more vigorously and remove milk effectively, which in turn stimulates the milk-making hormone cascade optimally.
In 2 days, Tonya’s baby became much more alert, demanded to be fed every 2-3 hours, and gained 7 ounces! Tonya included power-pumpingto increase her milk supply, and gradually, he could breastfeed exclusively. He continued to gain weight and thrive.

Left at 8 Weeks and Right at four months of age
Supplementation when necessary will not decrease a mother’s milk supply if her breasts are stimulated with direct nursing, pumping or hand expression for each supplemental feeding. But, it is very important not to miss any breastfeeding or pumping sessions when supplementing. Once the milk volume increases, supplementing will decrease or stop.
Krystal
Krystal was a first-time mom whose baby was born at 37 weeks by emergency c-section. Her baby was admitted to the NICU for 24 hours with respiratory support. She could breastfeed him several times in the NICU, but he was not satisfied and would cry and not settle after nursing. She was asked if he could be supplemented during the night as she was on another floor in the hospital and was not well enough to visit him during the night. She agreed and assumed he was being supplemented. She learned the pediatrician refused her baby supplementation because he insisted she be brought back to the NICU to nurse him.
He was released from the NICU after 24 hours, and for the next 24 hours, he was profoundly sleepy, jaundiced, and nursed poorly. He only had drops of colostrum, which Krystal self-expressed. She was concerned about how ‘orange’ his skin was, but she was told he was fine because he had wet diapers.
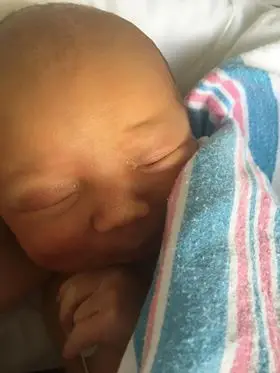
Sleepy, lethargic, and jaundiced.
When his pediatrician saw him the next morning, he was profoundly jaundiced and had lost 17 percent of his birth weight. He required immediate supplementation and ended up in the NICU for phototherapy and full feedings. His bilirubin level was 20, which is dangerously elevated.Supplementing this baby saved his life,but if he had been supplemented sooner, he would have avoided needless suffering. His parents were also saddled with debt from his second NICU admission.

Seventeen percent weight loss and profoundly jaundiced.
What we are learning
- We are learning that mothers in Western societies are experiencing delayed lactogenesis II (onset of full milk production) for complex and unknown reasons. This studysuggests that the prevalence of DOL has reached epidemic proportions.
- 22% of motivated, lactation-supported, exclusively breastfeeding mothers experience delays incopiousmilk productionthat increase the risk of excessive weight loss in their newborns by 7-fold.
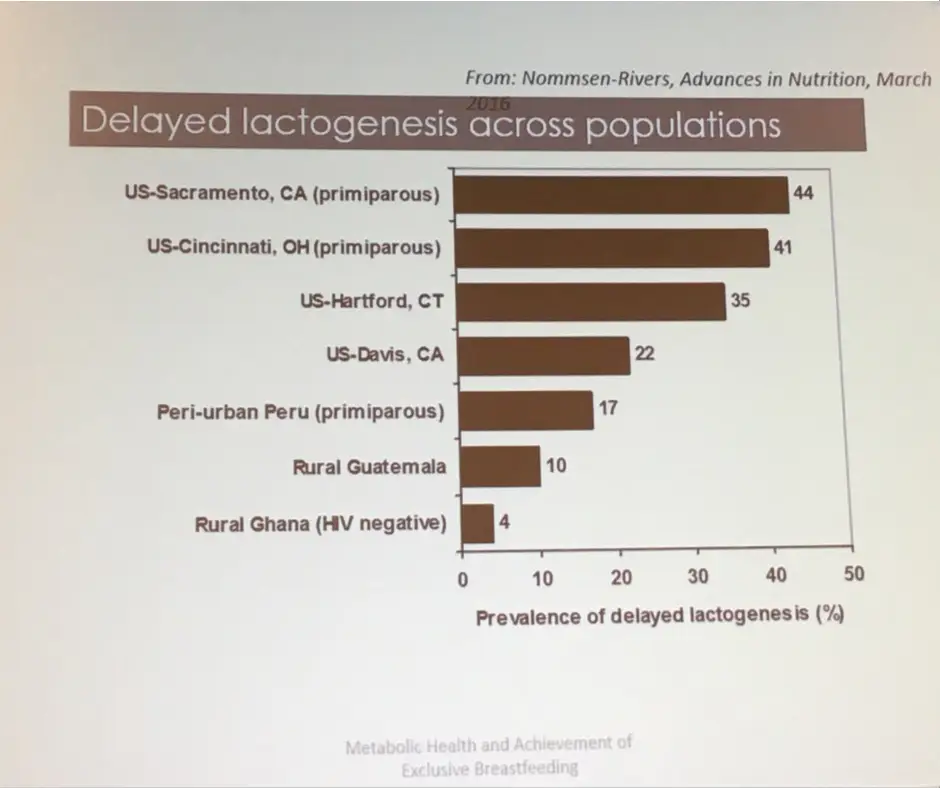
Nommsen-Rivers, Presented at 2017 ABM conference
Delayed onset of full milk production does not mean a mother won’t make enough milk. It means her baby will likely need supplementation along with breastfeeding or pumping until her milk suppy increases to meet her baby’s needs.
The mothers I see are terribly distraught when they find out they were not informed of the consequences of delayed onset of milk production, how to recognize the signs of hunger, or how to supplement safely.
No mother can accept that she unintentionally starved her baby.
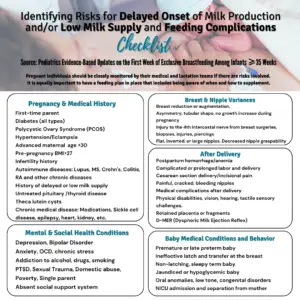
There is a lengthy list of maternal biological risk factorsfor mothers who may experience delayed onset of milk production and/or chronic low milk supply. Healthcare professionals are responsible for educating mothers about the signs of inadequate milk production and the risk factors for delayed milk production. At the same time, they are educating mothers on breastfeeding benefits and techniques.Identifying mothers with risk factors can help health professionals prevent newborn feeding complications while providing optimal breastfeeding management, which is critical in the first weeks after delivery.
Here, you’ll find various educational materials to help you best feed your newborn and some materials to help your clinicians best support you in doing so.
If you need help, please join our support groupor contact me directly at jody@fedisbest.org
Jody Segrave-Daly’s entire 32-year nursing career has been dedicated to caring for healthy and medically fragile babies in the nursery and NICU. When she began her community-based infant feeding practice ten years ago, she was unprepared to see the significant numbers of babies suffering from accidental starvation complications. The stories she heard were the same —distressed mothers were being told never to supplement their crying, sleepy, jaundiced, and dehydrated babies — or risk ruining their breastfeeding relationship and milk supply. She has comforted countless mothers worldwide who believed it was rare to under-produce breast milk and often felt betrayed by their healthcare teams, their bodies, and the social pressure that insisted “Breast Is Best.†Now a staunch advocate for the Fed Is Best movement, Jody works to debunk those myths while supporting mothers to breastfeed, mix-feed, pump-milk-feed,formula-feed and tube-feed their babies.

Contact directly atjody@fedisbest.org
Accidentally Starving My Baby Broke My Heart, But Made Me Want To Help Other Moms
https://fedisbest.org/2019/08/mandy-dukovan-talks-about-her-son-failing-to-thrive-from-constant-cluster-feeding/
References:
How To Breastfeed For The First 2 Weeks
The Truth About Not Being Able To Breastfeed
Breast Milk Production in the First Month after Birth of Term Infants
Know Your Risks for Delayed Onset of Full Breast Milk Supply
How To Deal With Low Breast Milk Supply
The Scientific Evidence on the Effects of Underfeeding on the Newborn Brain
Recognizing and Treating Delayed or Failed Lactogenesis II
The Truth About Not Being Able To Breastfeed
Anomalies in the Female Adolescent Breast
Breast Milk May Arrive Late for Obese New Moms
Most Cow’s Milk Baby Formulas Don’t Up Risk of Type 1 Diabetes
Breastfeeding and Allergy Protection
Does Circadian Disruption Play a Role in the Metabolic-Hormonal Link to Delayed Lactogenesis II?

5 thoughts on “Feed Your Baby—When Supplementing Saves Breastfeeding and Lives”