By Michelle M., Psychiatrist, MD, and First-Time Mother
It’s taken me a long time to really have the strength to talk about this, but I think it’s time.
I’m a 40-year-old, first time mom to an amazing 9-month-old son. Throughout my pregnancy I was repeatedly asked if I would breastfeed and received endless lectures on the benefits. I was honestly skeptical about the claimed breastfeeding benefits… (liquid gold? seriously?), but continued to answer “yes”, as it felt like saying “no” would be the wrong answer.
I figured I would try, and if it worked, great! If it didn’t, then formula was “Plan B”. I really didn’t think much of it, and figured the baby would get fed one way or another.
Fast forward to my 37th week of pregnancy. My water broke with no warning, and I had an awful labor due to a failed epidural and uterine tachysystole. Then to top it all off, I had an emergency c-section when my baby’s heart rate disappeared from the monitors. Labor and delivery didn’t go exactly as planned, but I was elated when it was over, and I had my beautiful baby.
However, the bliss I felt began to unravel quickly once I was in the recovery room. I was weak, nauseous and covered in blood and I realized I was expected to care for my baby. My husband was there to help, but the reality set in that no one was going to let me rest and recovery from my surgery.

My son being born at 37 weeks was weak and couldn’t latch effectively when trying to breastfeed. He also had what looked like the worst tongue tie I’d ever seen. His tongue was completely bowed in the front and stuck to the bottom of his mouth with a thick band of tissue. However, none of the hospital personnel seemed concerned.
“In my heart I knew things were wrong, but I felt powerless to change anything.”
When I had originally imagined this day, I imagined peacefully laying with my baby on my chest. But as the nurse repeatedly shoved my son’s face into my breast, causing him to scream and flail in protest, I realized that wasn’t going to happen. Nothing had prepared me for any of the chaos and stress I was experiencing.
Being unable to sustain a latch and breastfeed, my son’s hunger grew until he became more and more agitated. I only slept about 2 hours that first night as I listened to him cry and continued to try to feed him. In the morning, my first morning as a new mother, I felt miserable and like a failure instead of elated and joyful.
Blog post: I May Never Forgive The Hospital For Starving My Baby While Under Their Care!
Due to my son being unable to latch, the nurse attached a pump to my chest, which only drew blood, not milk. But despite that fact, I was told I needed to pump every 2 hours, or I would never produce milk. I was dehydrated, hypotensive and sweating profusely and my baby screamed and screamed cried. I felt inadequate and deeply ashamed.
I began to ask the obvious question, “How long can this go on for?”
–My baby was under 6 pounds and looked so tiny. He was clearly uncomfortable. I was told repeatedly his stomach is the size of a cherry and he doesn’t really need to eat. I was assured a few drops of colostrum would be enough.

Note: A term newborns stomach size is at least 20 ml. One teaspoon of colostrum is only THREE calories. Drops of colostrum are never enough to feed and hydrate a newborn.
“At what point do you intervene and give him formula?” I kept asking. No one seemed concerned. But I was. In my heart I knew things were wrong, but I felt powerless to change anything.
On day 3, my mother visited, and she intervened. The baby was alternately listless and screaming, though apparently, producing enough wet diapers for the nurses to not be concerned. My mother demanded a bottle of formula which the baby was given with a small cup.
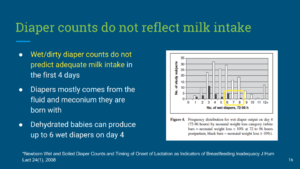
Note: Diaper counts do not reflect adequate hydration or nutrition status.
Blog post: f I Had Given Him Just One Bottle, He Would Still Be Alive. – Fed Is Best
I eventually insisted on a bottle, seeing how hungry he was, and he sucked down 2 ounces right away. My mother ushered the lactation consultant and nurses out of the room, and I was finally able to feed and soothe my baby.
This was the first peaceful bonding moment I had with him.
After another exhausting, sleepless night, we were discharged. I was still pumping every 2 to 3 hours as instructed, which still produced nothing but drops of blood. I resented pumping due to the way it took me away from my baby and isolated me in my bedroom. We had no instructions on feeding requirements with formula as the hospital didn’t recognize it.
Things only continued to go badly at the pediatrician’s office. The nurse who saw him noted his excessive weight loss. She said, “You really need to get him back on the breast.” But he had never been on the breast in the first place!
She demanded to know how many hours a day I was pumping, and I began to feel irritated because it was the only thing any provider seemed to care about. I wondered when I was supposed to sleep in between pumping and caring for a newborn.
I was so exhausted I was hallucinating.
Then, as if to try to deter me from using formula, the nurse told me formula would cause a rash on his chin because it’s full of sugar. And another nurse insisted we limit his feedings due to the risk of iron overload from formula. How on earth was I supposed to withhold feedings from a newborn?
In tears, and feeling like even more of a failure, we returned home from that first doctor’s appointment.
Dutifully, I returned to my breast pump, which caused nothing but pain and worsened my growing sense of isolation. My mental health was worsening by the day, and I wasn’t bonding with my baby because I was so busy pumping and worrying that I’d never produce milk.
Finally, one day maybe two weeks in, I decided I was done. My mother was the only person who supported this decision. Everyone else told me in different ways that I wasn’t trying hard enough or trying the right things. But I knew it was time to stop. With the encouragement of my mother, I boxed up the pump and put it out of sight in a closet.
That is when I truly began to enjoy time with my son.
It has been a long way back from those frightening first days in the hospital. I experienced depression and guilt that I didn’t stand up for myself and baby and anger at the tunnel vision of my healthcare providers.
As a psychiatrist I have been a staunch advocate for women’s mental health, and I have always treated women with high-risk mental health conditions during their pregnancies and beyond. After my birthing and breastfeeding experience, I am deeply concerned that women are being pressured and lied to at the most vulnerable time in their lives. A time when they need to feel empowered; not doubted, gaslighted and coerced.
We need to do better.
-Michelle M. Psychiatrist, M.D.
Michelle M. is a Board Certified Psychiatrist dedicated to caring for the psychological health of all of her patients. It was not until she struggled with her own mental health due to the pressures of exclusive breastfeeding that she felt her story needed to be shared with other new mothers. In an effort to help change the narrative about exclusive breastfeeding to one of empowering women to choose what is best for them, she has allowed us to share her story with you.
Clinicians’ Guide to Supporting Parents with Guilt About Breastfeeding Challenges
Feeding Your Baby—When Supplementing Saves Breastfeeding and Saves Lives
HOW YOU CAN SUPPORT FED IS BEST
There are many ways you can support the mission of the Fed is Best Foundation. Please consider contributing in the following ways:
- Send us your stories. Share with us your successes, your struggles and everything in between. Every story saves another child from experiencing the same and teaches another mom how to safely feed her baby. Every voice contributes to change.
- If you need infant feeding support, we have a private support group– Join us here.
- If you or your baby were harmed from complications of insufficient breastfeeding please send a message to contact@fedisbest.org
- Make a donation to the Fed is Best Foundation. We are using funds from donations to cover the cost of our website, our social media ads, our printing and mailing costs to reach health providers and hospitals. We do not accept donations from breast- or formula-feeding companies and 100% of your donations go toward these operational costs. All the work of the Foundation is achieved via the pro bono and volunteer work of its supporters.
- Share the stories and the message of the Fed is Best Foundation through word-of-mouth, by posting on your social media page and by sending our FREE infant feeding educational resources to expectant moms that you know. Share the Fed is Best campaign letter with everyone you know.
- Write a letter to your health providers and hospitals about the Fed is Best Foundation. Write to them about feeding complications your child may have experienced.
- Print out our letter to obstetric providers and mail them to your local obstetricians, midwives, family practitioners who provide obstetric care and hospitals.
- Write your local elected officials about what is happening to newborn babies in hospitals and ask for the legal protection of newborn babies from underfeeding and of mother’s rights to honest informed consent on the risks of insufficient feeding of breastfed babies.
- Join us in any of the Fed is Best volunteer and advocacy, groups. Click here to join our health care professionals group. We have: FIBF Advocacy Group, Research Group, Volunteer Group, Editing Group, Social Media Group, Legal Group, Marketing Group, Perinatal Mental Health Advocacy Group, Private Infant Feeding Support Group, Global Advocacy Group, and Fundraising Group. Please send an email to Jody@fedisbest.org if you are interested in joining any of our volunteer groups.
- Send us messages of support. We work every single day to make infant feeding safe and supportive of every mother and child. Your messages of support keep us all going.

One thought on “How Breastfeeding Coercion Stripped this Psychiatrist of Her Confidence and Mental Health”