by Christie del Castillo-Hegyi, M.D.
On October 14, 2019, the Journal of Pediatrics published astonishing findings regarding the effects of the Baby-Friendly hospital certification on sustained breastfeeding rates as defined by the 2020 Healthy People Goals of:
- any breastfeeding at 6 and 12 months
- exclusive breastfeeding at 3 and 6 months.
They did so by measuring the relationship between statewide breastfeeding initiation rates data and the above breastfeeding rates. They then measured the contribution of Baby-Friendly hospital designation on these same breastfeeding outcomes.
According to the study authors, the increase in hospital designation in the Baby-Friendly Hospital Initiative (BFHI) began in 2011 when the U.S. Surgeon General issued a call to action for maternity care practices throughout the U.S. to support breastfeeding. The Centers for Disease Control (CDC) became involved in promoting the BFHI policies in hospitals and health facilities, as breastfeeding was thought to be associated with lower rates of childhood obesity. The assumption was that by increasing breastfeeding rates through the BFHI, there would be a concomitant decline in childhood obesity. Upon initiation of this program, the CDC initiated surveillance of state-specific data on breastfeeding outcomes after discharge including BFHI designation rates. This data is made available to the public through the CDC Breastfeeding Report Card, which provides annual reports from 2007 through 2014 and biennial reports from 2014.
As expected, they found that states with higher breastfeeding initiation rates had higher rates of these sustained breastfeeding outcomes. You cannot have high breastfeeding rates unless mothers are given education and successfully initiate breastfeeding. However, when they measured the effects of Baby-Friendly certification, this is what they found.
“Baby-Friendly designation did not demonstrate a significant association with any post-discharge breastfeeding outcome (Figures 1, B and 2, B). There was no association between Baby-Friendly designation and breastfeeding initiation rates.”
In other words, Baby-Friendly hospital certification did not meet the intended goal of increasing breastfeeding rates in the U.S.
Here are the graphs showing these relationships:

Figure 1, A shows increasing rates of breastfeeding at 6 and 12 months with higher statewide breastfeeding initiation rates. Figure 1, B shows no effect of the Baby-Friendly Hospital certification (as measured by percent of births occurring in BFHI hospitals) on 6 and 12-month breastfeeding rates.

Figure 2. Higher rates of statewide breastfeeding initiation was shown to predict higher rates of 3 and 6-month exclusive breastfeeding, while percent of Statewide BFHI hospital births had no effect on exclusive breastfeeding rates.
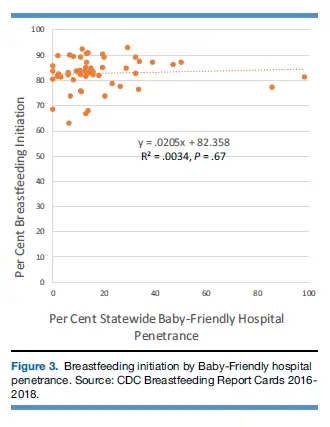
Figure 3 shows no relationship between higher breastfeeding initiation rates and percent of births at BFHI hospitals.
They state that this is particularly important given “recent concerns about adverse neonatal sentinel events associated with some of the prescribed compliance requirements of Baby-Friendly designation.” They also state that the CDC and a US Preventive Services Task Force report called into question the efficacy of Baby-Friendly designation in meeting its breastfeeding objectives. They referred to reports regarding associated “neonatal sentinel events including sudden unexpected postnatal collapse (SUPC), newborn falls, and newborn dehydration and jaundice, which are recognized by the American Academy of Pediatrics, the WHO, The Joint Commission, and the CDC.”
What are the requirements of BFHI hospital credentials that distinguish it from simple breastfeeding initiation?
Everyone agrees that it is important to teach mothers the techniques of breastfeeding before and in the days after birth in order to ensure successful sustained breastfeeding after hospital discharge. The process of teaching mothers to breastfeed in the first hours to days after birth is what is considered “breastfeeding initiation.” This includes exclusive and non-exclusive breastfeeding practices. However, BFHI certification requires more rigid adherence to the WHO/UNICEF Ten Steps to Successful Breastfeeding policies and emphasizes exclusive breastfeeding. It actively discourages formula-feeding and even formula supplementation of breastfed newborns (with exception to medical complications caused by the policy as well as other indications) through its patient education curriculum and health professional training. The policy commonly results in negative patient experiences and serious negative patient outcomes. Among the Baby-Friendly policies that have limited to no benefit and has repeatedly been documented to result in patient harm are the following:
Step 4: Place babies in skin-to-skin contact with their mothers immediately following birth for at least an hour.
Step 6: Give infants no food or drink other than breast-milk, unless medically indicated.
Step 7: Practice rooming in – allow mothers and infants to remain together 24 hours a day
Step 9: Give no pacifiers or artificial nipples to breastfeeding infants.
Step 4: Skin-to-Skin Contact
According to the 2017 WHO revised breastfeeding guidelines, moderate-quality evidence showed modest benefits of immediate (<10 min after birth) or early (10 min – 24 hours) skin-to-skin contact (SSC) (Step 4) in increasing breastfeeding rates at discharge to 1 month of age by 30%. Low-quality evidence shows it improved breastfeeding from 6 weeks to 6 months by 50%. Similar findings were seen in low-birth-weight infants showing any and exclusive breastfeeding rates “probably” increased at discharge from the hospital or at 40-41 weeks gestation (for premature infants), showing a 16-20% increase. SSC was also associated with a 17-20% increase in any and exclusive breastfeeding at 1-4 months but no effect on exclusive breastfeeding at 6-12 month follow-up.
However, skin-to-skin care, especially in unsupervised, sleep-deprived mothers recovering from labor and delivery, particularly those recovering from cesarean section, is associated with accidental bed-sharing and infant falls and suffocation. This has led to newborn brain injuries, cardiac arrest, and deaths among previously healthy infants, also known as Sudden Unexpected Postnatal Collapse (SUPC). SUPC is estimated to occur 2.6 to 133 cases per 100,000 newborns. This has gained recent media attention and has prompted the American Academy of Pediatrics to publish an policy in 2016 called, “Safe Sleep and Skin-to-Skin Care in the Neonatal Period for Healthy Term Newborns.” This is a known complication of the Baby-Friendly initiative, which parents are currently not informed of through proper informed consent upon recruitment to the Baby-Friendly protocol.
Step 7: 24-hour rooming-in
Step 7 of the BFHI policy encourages parents to room in 24 hours a day immediately after delivery. Mothers are commonly sleep-deprived and exhausted after labor and delivery, some laboring for > 24 hours, some recovering from major surgery. They are required to nurse and care for a newborn almost immediately after delivery with few exceptions while sleep-deprived and exhausted. In combination with unsupervised skin-to-skin care (Step 4) and frequent (sometimes continuous) breastfeeding and crying, maternal exhaustion has lead to tragic and preventable accidental newborn falls from bed and suffocation while breastfeeding and doing SSC. These have resulted in brain injury, severe disability and rare deaths in previously healthy infants. The elimination of newborn nurseries by hospitals has increased as a result of this policy. Hospital policies that implicitly or explicitly pressure parents to avoid nursery care even when they are impaired have lead to these tragic outcomes.
What is more ludicrous is that the 24-hour rooming-in policy has been shown to have no effect on increasing sustained breastfeeding after discharge. The 2017 WHO revised breastfeeding guidelines reviewed all the data regarding this policy and showed no effect of 24-hour rooming-in on breastfeeding rates at 3-4 months. Despite the negative short-term effects of this policy on parental sleep and rare serious effects on the infant in the form of falls and SUPC, neither the WHO nor Baby-Friendly USA have changed this recommendation. In fact, health professionals are scripted to try to discourage parents from sending their infants to the nursery if they express the need for sleep, which ultimately puts infants at risk by perpetuating the unsafe condition of being cared for by an impaired parent. Furthermore, the policy is inhumane to women recovering from childbirth.
Step 9: No pacifiers and artificial nipples
Step 9 of the Ten Steps recommends no pacifiers and artificial nipples for breastfeeding infants. Why would a newborn need a pacifier? Exclusively breastfed newborns often experience persistent hunger from the low caloric yield of exclusive colostrum feeding. They often experience what is called, “Second Night Syndrome,” or constant crying and nursing from persistent hunger and thirst. Parents have commonly requested pacifiers to soothe their hungry babies, which is discouraged by Step 9. However, the 2017 WHO revised breastfeeding guidelines found no effect of avoiding pacifiers on breastfeeding rates. In combination with evidence that pacifier use reduces Sudden Infant Death Syndrome (SIDS), the WHO dropped its recommendation to discourage pacifier use. Similarly, the use of artificial nipples and bottles when supplementing with pumped breast milk, donor breast milk or formula in cases where direct breastfeeding is not possible showed no effect on exclusive and “any” breastfeeding rates at discharge, at 2 and 6 months. As a result, the WHO stated that bottles and teats are now acceptable methods of supplementary feeding. This recommendation has not been adopted by Baby-Friendly USA and is still in effect in Baby-Friendly hospitals.
Step 6: Give no food or water other than breast milk unless medically indicated
Lastly, Step 6 recommends giving no food or water other than breast milk unless medically indicated. This recommendation has consistently been shown to increase the risk of excessive jaundice, dehydration, hypoglycemia, extended and repeat hospitalization from insufficient feeding while exclusively breastfeeding.

Compilation of Feeding Complications in Exclusively Breastfed vs. Ad-Lib Supplemented and Formula-Fed Newborns. References found in the Fed is Best Foundation Submitted Comments to the USDA Dietary Guidelines Committee.
Exclusive breastfeeding is now identified as the leading risk factor for newborn rehospitalization, which occurs to 1 in 25 to 1 in 71 previously healthy, term newborns. While this is the most prominent recommendation of the BFHI and is its primary hospital quality metric, randomized controlled trials (the gold standard for determining the effectiveness of interventions) continue to show that judicious supplementation either don’t interfere or slightly improve breastfeeding rates and patient outcomes (e.g. reduction of readmissions for feeding complications). Two of those studies were available at the time of 2017 WHO revised breastfeeding guidelines and the systematic review showed that the combined data showed a 20% increase in 3-month exclusive breastfeeding rates among supplemented newborns compared to exclusively breastfed newborns (low-quality evidence due to the size of the studies). Despite this evidence, the WHO continued to recommend exclusive breastfeeding from birth while failing to mention the most common and most serious adverse effects of the recommendation, namely increased rates of jaundice, dehydration, and hypoglycemia, all known causes of long-term developmental disability and rare deaths. Since 2017, three more randomized controlled trials on the effects of judicious supplementation with formula or donor milk on sustained breastfeeding rates have been published, which showed no impact on 3-month breastfeeding rates, one showing reduced readmissions for supplemented newborns, another showing no impact on 6- and 12-month breastfeeding rates when controlled for maternal intended duration to breastfeed.
Randomized, Controlled Trials on Effects of Limited Formula or Donor Milk Supplementation on Breastfeeding Rates
- Limited Amount of Formula May Facilitate Breastfeeding: Randomized, Controlled Trial to Compare Standard Clinical Practice versus Limited Supplemental Feeding
- The Effect of Early Limited Formula on Breastfeeding, Readmission, and Intestinal Microbiota: A Randomized Clinical Trial
- Limited Amount of Formula May Facilitate Breastfeeding: Randomized, Controlled Trial to Compare Standard Clinical Practice versus Limited Supplemental Feeding
- Effect of Donor Milk Supplementation on Breastfeeding Outcomes in Term Newborns: A Randomized Controlled Trial
- Effect of Early Limited Formula on Breastfeeding Duration in the First Year of Life
Conclusion
Despite these updates to the original WHO Ten Steps to Successful Breastfeeding, Baby-Friendly USA has failed to adopt the revised WHO recommendation of removing the “no pacifier and no bottles or artificial teats” rule. In addition, despite lack of evidence on efficacy and widely published evidence of harm caused by Step 6, “Give no food or water other than breast milk unless medically indicated,” neither Baby-Friendly USA nor the WHO have relinquished their recommendation to avoid formula supplementation in the days after birth. Lastly, while the risk of infant falls and death from maternal exhaustion caused by 24 hour rooming and unsupervised skin-to-skin care and breastfeeding are rare, the policies continue to be recommended despite little to no effect on sustained breastfeeding after discharge. These practices continue to be recommended to families with no process of providing informed consent regarding the risks when they are recruited to follow the Baby-Friendly policies.
To this day, the Fed is Best Foundation regularly receives stories from unsuspecting parents who were encouraged to follow the original Ten Steps by their Baby-Friendly credentialed and non-credential hospitals, leading to preventable insufficient feeding complications and hospitalizations of their newborns. We have also received reports of deaths from infant starvation as well as accidental bed-sharing and suffocation from parents and health professionals. We have submitted a comment to the 2020 USDA Dietary Guidelines Committee asking them to advise the Health Secretary to withdraw support from the Baby-Friendly Hospital Initiative given U.S. data showing that it is ineffective at increasing breastfeeding rates and extensive data demonstrating its harms. We asked the Committee to engage experts in the field of infant feeding to redesign recommended hospital policies to improve breastfeeding initiation for families who choose to breastfeed. We hope they will model these recommendations after new hospital initiatives like the Rush Family-Friendly Initiative, whose model provides support to breastfeeding, combination-feeding and formula-feeding families alike while prioritizing safety and respect for patient choice.
Nurses Are Speaking Out About The Dangers Of The Baby-Friendly Health Initiative
https://fedisbest.org/2018/11/neonatal-nurse-practitioner-speaks-out-about-the-dangerous-and-deadly-practices-of-the-bfhi/
NICU Nurse Discloses Newborn Admission Rates From Breastfeeding Complications in BFHI Unit
If I Had Given Him Just One Bottle, He Would Still Be Alive.
CONTACT US/VOLUNTEER
THANK YOU FOR YOUR INTEREST IN THE FED IS BEST FOUNDATION!
Our mission statement is:
The Fed Is Best Foundation works to identify critical gaps in the current breastfeeding protocols, guidelines, and education programs and provides families and health professionals with the most up-to-date scientific research, education, and resources to practice safe infant feeding, with breast milk, formula or a combination of both.
Above all, we strive to eliminate infant feeding shaming and eliminate preventable hospitalizations for insufficient feeding complications while prioritizing perinatal mental health.
HOW YOU CAN SUPPORT FED IS BEST
There are many ways you can support the mission of the Fed is Best Foundation. Please consider contributing in the following ways:
- Join us in any of the Fed is Best volunteer and advocacy, groups. Click here to join our health care professionals group. We have: FIBF Advocacy Group, Research Group, Volunteer Group, Editing Group, Social Media Group, Legal Group, Marketing Group, Perinatal Mental Health Advocacy Group, Private Infant Feeding Support Group, Global Advocacy Group, and Fundraising Group. Please send an email to Jody@fedisbest.org if you are interested in joining any of our volunteer groups.
- If you need infant feeding support, we have a private support group– Join us here.
- If you or your baby were harmed from complications of insufficient breastfeeding please send a message to contact@fedisbest.org
- Make a donation to the Fed is Best Foundation. We are using funds from donations to cover the cost of our website, our social media ads, our printing and mailing costs to reach health providers and hospitals. We do not accept donations from breast- or formula-feeding companies and 100% of your donations go toward these operational costs. All the work of the Foundation is achieved via the pro bono and volunteer work of its supporters.
- Sign our petition! Help us reach our policymakers, and drive change at a global level. Help us stand up for the lives of millions of infants who deserve a fighting chance. Sign the Fed is Best Petition at Change.org today, and share it with others.
- Share the stories and the message of the Fed is Best Foundation through word-of-mouth, by posting on your social media page and by sending our FREE infant feeding educational resources to expectant moms that you know. Share the Fed is Best campaign letter with everyone you know.
- Write a letter to your health providers and hospitals about the Fed is Best Foundation. Write to them about feeding complications your child may have experienced.
- Print out our letter to obstetric providers and mail them to your local obstetricians, midwives, family practitioners who provide obstetric care and hospitals.
- Write your local elected officials about what is happening to newborn babies in hospitals and ask for the legal protection of newborn babies from underfeeding and of mother’s rights to honest informed consent on the risks of insufficient feeding of breastfed babies.
- Send us your stories. Share with us your successes, your struggles and everything in between. Every story saves another child from experiencing the same and teaches another mom how to safely feed her baby. Every voice contributes to change.
- Send us messages of support. We work every single day to make infant feeding safe and supportive of every mother and child. Your messages of support keep us all going.
- Shop at Amazon Smile and Amazon donates to Fed Is Best Foundation.
Or simply send us a message to find out how you can help make a difference with new ideas!
For any urgent messages or questions about infant feeding, please do not leave a message on this page as it will not get to us immediately. Instead, please email christie@fedisbest.org.
Thank you and we look forward to hearing from you!


These so-called baby friendly hospitals are putting babies lives at risk in more ways than one and we would like to go back to the days when moms are able to relax after giving birth and know that their babies are safe in the nursery and not at risk for fall or suffocation because they are exhausted or their babies are not at risk for dehydration, hypoglycemia, hyperbilirubinemia or even starvation because they’re not being forced to exclusively breastfeed when there’s not much breast milk supply. Baby friendly hospitals are also putting nurses lives at risk by forcing the nurse to wash an infant born to a covid + mom in the room (rooming in) which most of the time is very small and clustered and pretty much unsafe and therefore further exposing themselves to covid unnessarily. In many of these cases both mom and dad /support person are covid+.