Frequently Asked Questions
WRITTEN AND EDITED BY JODY SEGRAVE-DALY, RN, IBCLc, LYNNETTE HAFKEN, MA, IBCLC, and Christie del Castillo-Hegyi, MD
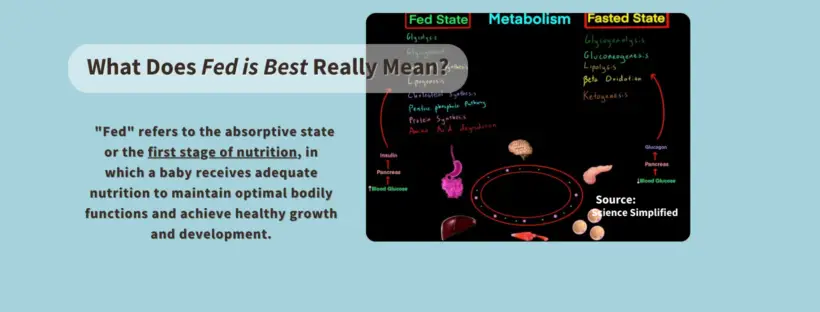
Our goal is to respond to the many statements that have been made about the Fed is Best Foundation and to answer questions we receive about what the Foundation stands for. Unfortunately, our #FedIsBest phrase has been used incorrectly by others, and it’s important that we clarify what it means and doesn’t mean. Our mission statement has evolved over time and reflects what our parents tell us they need to support them.
Mission statement:
The Fed is Best Foundation works to identify critical gaps in current breastfeeding protocols, guidelines, and education programs. We provide families and health professionals with the most up-to-date scientific research, education, and resources to practice safe infant feeding with breast milk, formula, or a combination of both. To be fully informed, parents must be taught about the risks of insufficient breast milk intake while supporting exclusive breastfeeding in order to eliminate preventable hospitalizations for insufficient feeding complications. Finally, we strive to eliminate infant feeding shaming while prioritizing perinatal mental health.
We will be answering 20 questions that we have received, and this blog is Part 1.
Questions:
1. Why do you spend so much time on the risks of exclusive breastfeeding and so little on the benefits?
We promote safe breastfeeding because no other health organization informs parents about the risks and how easy they are to prevent. As part of this mission, we want lactating parents who choose to exclusively breastfeed to be successful in their long-term goals while ensuring the safety and long-term health and development of their infants.
For parents who wish to avoid formula use, we believe that donor milk should be made available in hospitals if supplementation is needed so that they can meet their exclusive breast milk feeding goals. But for mothers who wish to use formula supplementation in order to avoid donor milk, their wishes should be respected as well.
Formula milk has a healthy place in infant feeding and saves lives too, particularly for infants whose mothers cannot produce enough milk. We believe that characterizing properly-prepared formula as substandard or even dangerous, as has been done by many exclusive breastfeeding advocacy groups, is irresponsible and puts infants and mothers’ lives at risk. Furthermore, it is untruthful and emotionally abusive to families who use it.
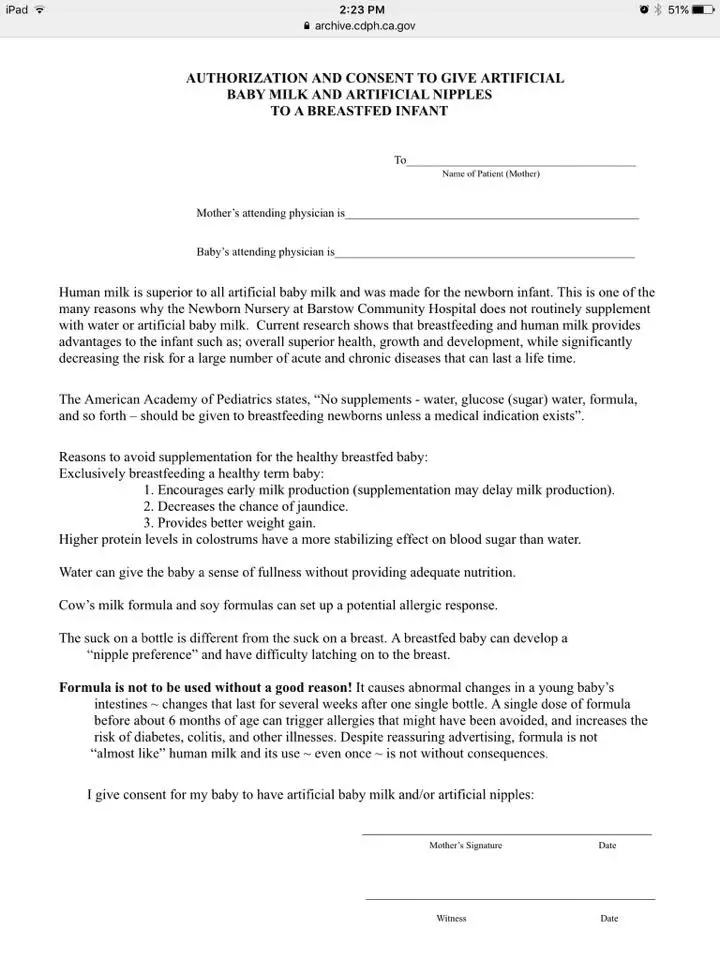
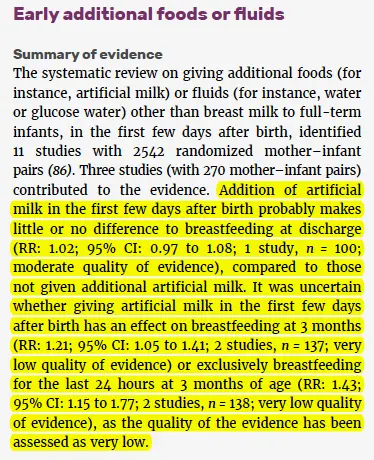
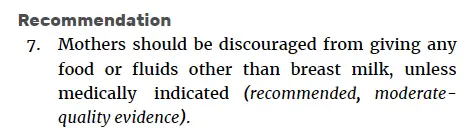
We feel that hospital infant formula “informed consent” forms that deliberately characterize supplemental formula as harmful provide inaccurate information and can lead parents to avoid formula supplementation that may ultimately prevent serious outcomes. Given that the multiple diseases commonly listed have not been studied in cases of short-term formula supplementation in properly controlled trials, there is no proven causal relationship between judicious formula supplementation and these negative health outcomes.
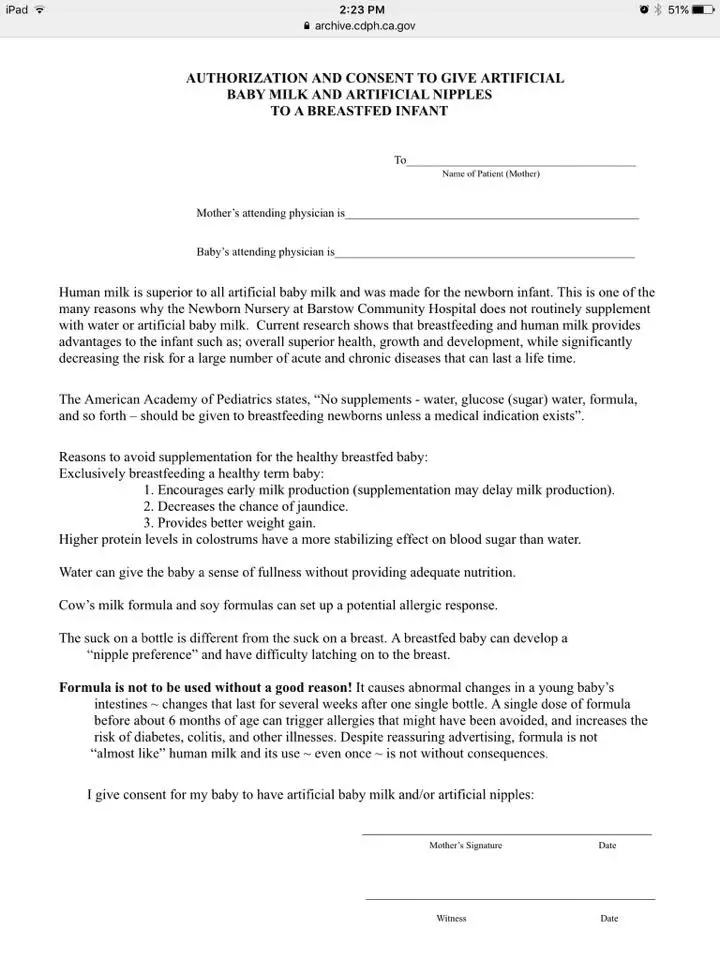
A consent form mothers are required to sign before feeding their babies formula.

Example of text scripting given to nurses to respond to parents who are asking to feed their babies formula, using pacifiers or the nursery.

Example of text scripting given to nurses for parents who are asking for formula, pacifiers or the nursery.
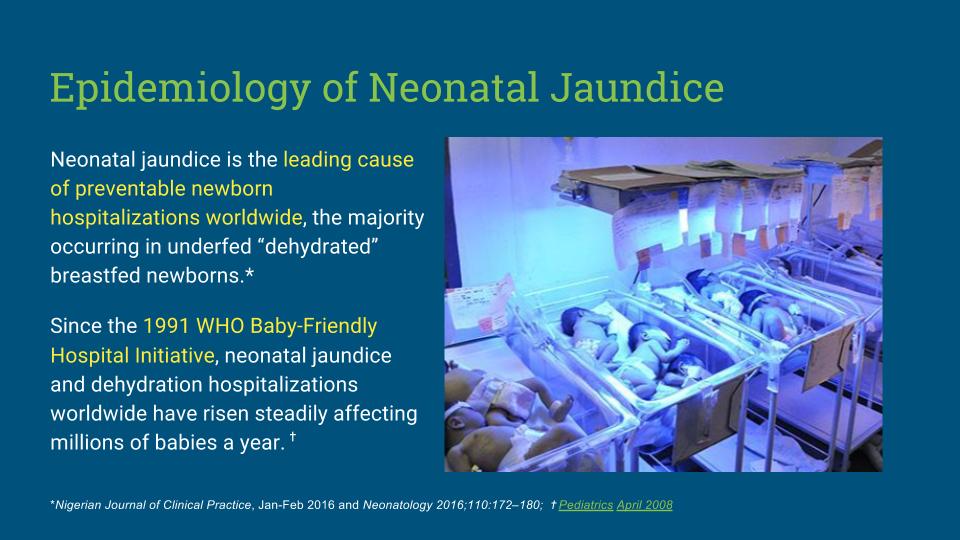
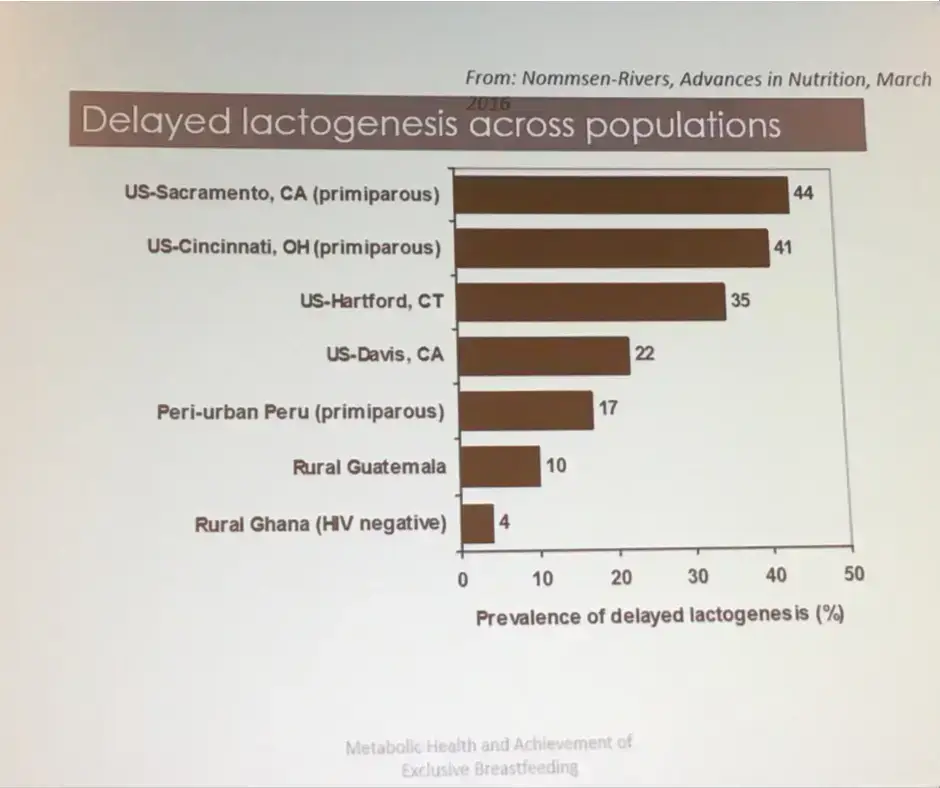
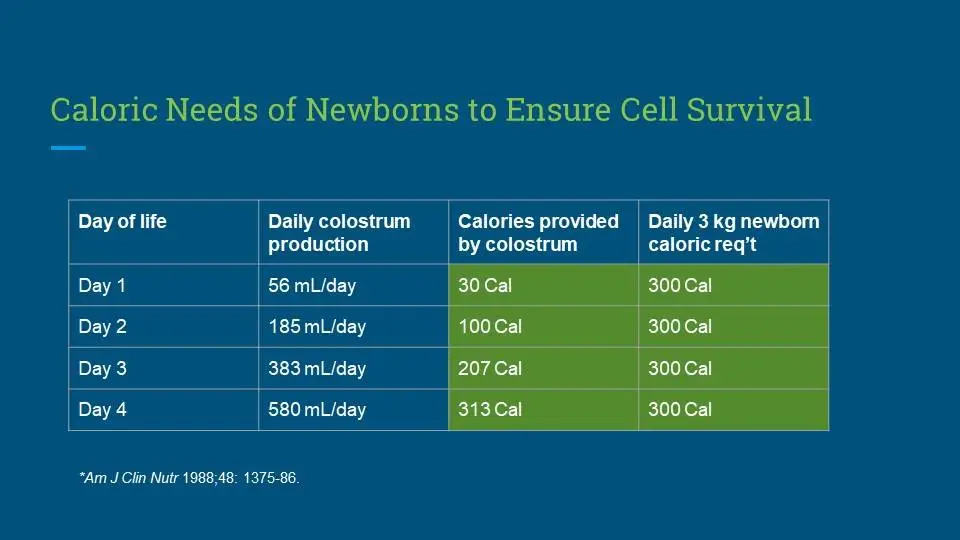
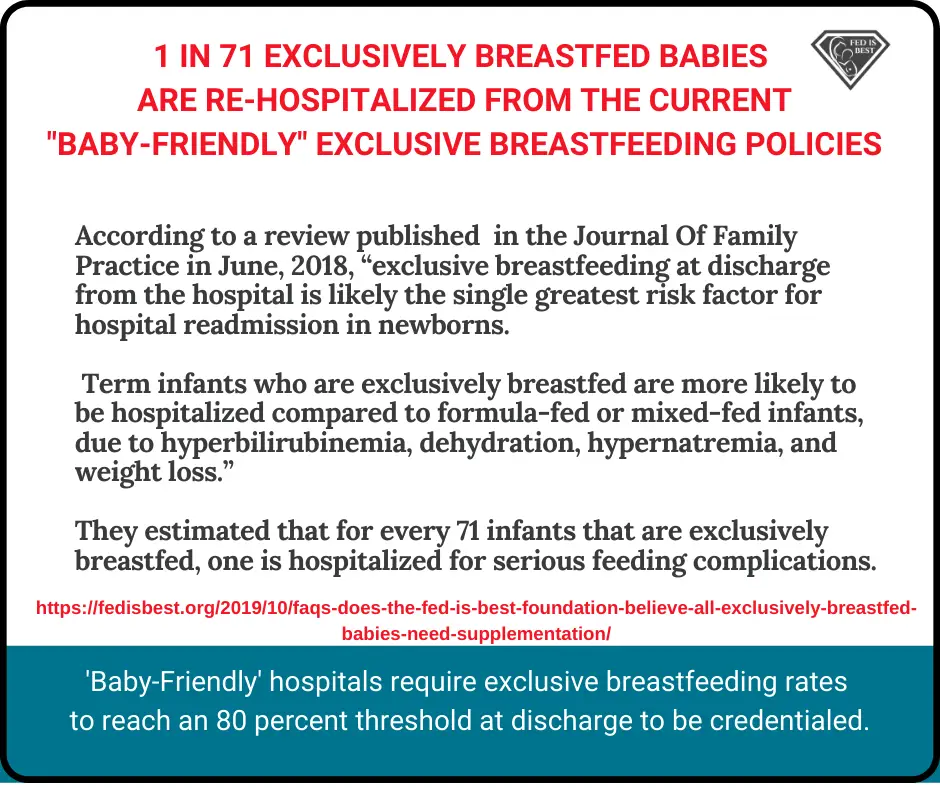
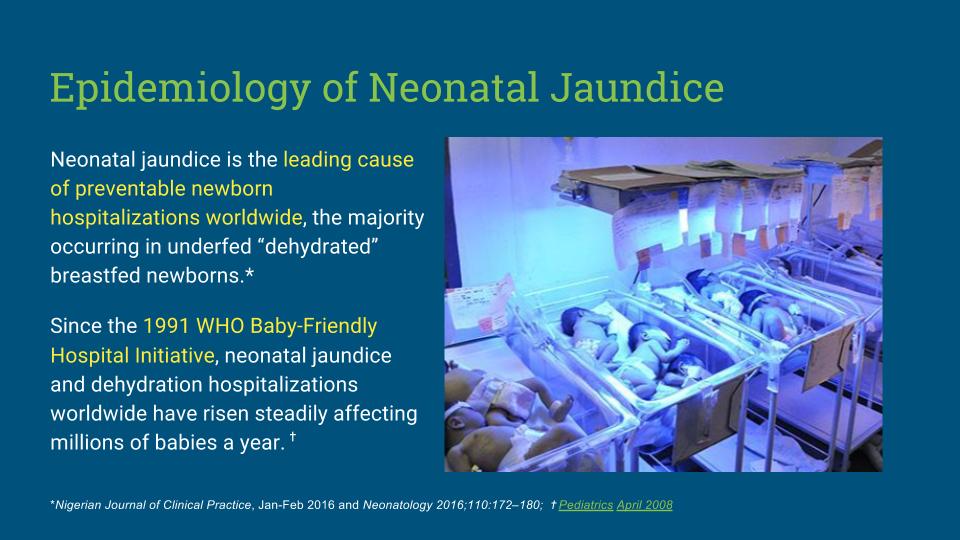
We also feel that the message that exclusive breastfeeding is best for all lactating parents and infants is not only inaccurate given how common it is to be unable to sustain breastfeeding even with maximal lactation support, but it also leads to thousands of preventable hospital admissions every year in the U.S. alone. As health care professionals we take an oath to do no harm and readmitting a previously healthy newborn who has become critically ill because they did not receive enough breast milk as a result of our counseling is a violation of that oath and should be a “never event.” Unfortunately, it has become a routine, even expected outcome of exclusive breastfeeding promotion that occurs in every hospital that uses the Baby-Friendly protocol.
| According to the National Quality Forum (NQF), “never events” are errors in medical care that are clearly identifiable, preventable, and serious in their consequences for patients, and that indicate a real problem in the safety and credibility of a healthcare facility. |
Breastfeeding Benefits
2. How can a doctor and nurse IBCLC support the idea that formula and breast milk are equal? Do you think formula is as good as breast milk?
Our message has always been that breast milk has health benefits for babies, and breastfeeding also has health benefits for mothers. When we study breastfeeding vs. formula-feeding, there appear to be advantages to breastfeeding on average. One advantage is the reduction of gastrointestinal and respiratory infections which may be related to the presence of infection-fighting antibodies or other immune factors in breast milk that is not present in formula.
There has never been a time that we said formula milk and breast milk are the same. We want to make this very clear as our message has been co-opted by others in order to discredit the Fed is Best Foundation’s mission.
The health benefits of breastfeeding for both mother and baby are well documented in the scientific literature and include:
- Reductions in respiratory infections
- Reductions in gastrointestinal infections up to 12 months
- Reductions in necrotizing enterocolitis in premature infants
- A small but measurable reduction in SIDS and childhood leukemia
However, the scientific data has also shown, when we account for maternal income, education and even maternal intention to breastfeed, those advantages are not so solid. When comparing breastfed versus formula-fed siblings, the differences in health outcomes and intelligence are even less. Furthermore, the studies are unable to account for the effects of breast milk supply on infant health outcomes, which vary widely. Feeding complications in breastfed infants who do not get timely and adequate supplementation also have negative health consequences, which are not accounted for in those studies, but may ultimately affect outcomes in babies are categorized as “formula-fed.”
For individual mother-baby dyads for whom breast milk is insufficient, where breastfeeding causes excessive maternal sleep deprivation and postpartum depression or otherwise fails to allow the mother and baby to thrive physically and emotionally, there are clear harms to promoting exclusive breastfeeding and characterizing formula as substandard or harmful. For those mothers and babies, partial or exclusive formula-feeding may provide the best health outcomes over breastfeeding. For a smaller portion of mother-infant dyads, breastfeeding is contraindicated, like for galactosemia.
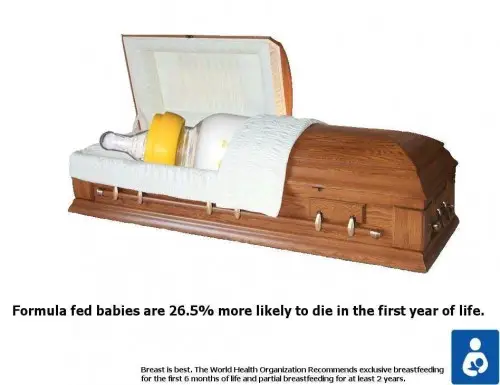
The promotion of exclusive breastfeeding has taken an irresponsible detour by demonizing formula milk in the hopes of encouraging mothers to exclusively breastfeed when for up to 15% of the population, it is not only impossible, it is unsafe. Formula milk has been depicted as a dangerous form of nutrition for babies, which is absolutely false. The intent is to shame and guilt parents for using it. Such characterization of formula as harmful and substandard puts infant lives at risk as mothers with insufficient milk have and will sometimes unwittingly starved their infants in order to meet the socially expected standard of exclusive breastfeeding, particularly if they are not informed of the harmful consequences like impaired brain development and disability.
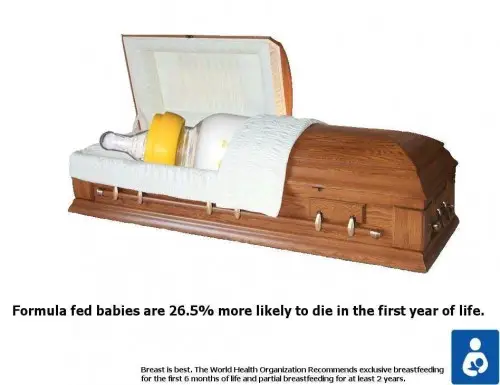
The image above is an example of a bullying tactic mothers are subjected to.
Laura: At first, I felt like a total failure and could not understand why my breasts would not do what they were supposed to. I would sob as I fed her. But over time I saw how much she was thriving and I started to forgive myself. I truly believe supplementing and then EFF saved me from hurting myself and allowed me finally to love my baby.
When a breastfeeding mother does not make enough breast milk, they are taught to avoid formula supplementation, while not being taught the signs and consequences of insufficient feeding. They will follow their health professionals’ advice even if their child exhibits persistent hunger until it becomes blatantly obvious that their child is critically ill. Formula milk is a nutritious food for babies and it does not need to be denigrated to encourage mothers to breastfeed. In a world where breastfeeding insufficiency is common, families need to be told how to recognize insufficient feeding and how to properly prepare formula when supplementation is needed. Such information should also be respectfully provided to families who make the informed-decision to formula-feed without judgment or harassment from health professionals.
We acknowledge and condemn the scandalous actions of Nestle corporation in the 1970s where formula was aggressively marketed to mothers in developing nations and ultimately led to the death of millions of babies from malnutrition and gastrointestinal illness from contaminated and diluted milk. It has created a very negative bias among some lactation professionals against formula itself. Let’s start separating the product, which was developed by doctors and is tightly regulated by the FDA, from the ethical violations of its manufacturer. We cannot let history be repeated by allowing aggressive marketing of the exclusive breastfeeding policy to harm millions of babies in the form of insufficient feeding complications, injuries, and deaths. Infant formula has saved millions of lives. Ethical and safe support of breastfeeding and formula-feeding are needed in order to achieve optimal health and development for all infants across the globe.
We will continue to support and protect breastfeeding without denigrating formula use because it’s the ethical thing to do. We believe that being respectful of formula-feeding families and of formula itself is not anti-breastfeeding, it is responsible, inclusive, and pro-safe infant feeding for all infants.
3. Why do you promote formula instead of donor milk?
We absolutely support screened banked donor milk and think it should be widely available for mothers who want to use it. The reality though is that it is not currently available to most term babies due to its limited availability and the need to prioritize its use in premature babies. While banked donor milk for short-term supplementation may be feasible and covered by health insurance, long-term supplementation with banked donor milk is financially not feasible for most families. Casual breastmilk donation and sharing, especially obtained from people through the internet, is particularly unsafe as it can carry transmittable infections and be contaminated with bacteria from inappropriate handling and storage. While we don’t shame mothers who use it, as licensed health care professionals, we follow the AAP and the CDC recommendations on casual milk sharing.
Ultimately, we need to work with the current situation that mothers are in, and most of the time safe donor milk is not feasible. Our top priority is to make sure babies are sufficiently fed.
4. How do you respond to concerns about “scaring new mothers” so they don’t even try to breastfeed because of the stories you write about?
We know our blog stories are very difficult to hear. Our intention is not to scare anyone, but to raise awareness on the risk factors and signs of feeding complications and by giving accurate information to mothers and health professionals. All parents are informed by their health professionals about other difficult but necessary parenting topics such as car seat safety, safe sleep practices, and even shaken baby syndrome to help prevent injury or death. But they are not told about the risks and serious consequences of inadequate breast milk intake to their babies and how to prevent complications.
We provide parents an actionable breastfeeding plan that allows them to make informed decisions in cases of insufficient or delayed copious milk production while protecting their right to successfully breastfeed. Parents commonly give us positive feedback on our breastfeeding plan and are thrilled when they are able to meet their breastfeeding goals safely and without the tears and trauma (for both mom and baby) that some experienced during their first attempt. Many moms report succeeding in sustaining a breastfeeding relationship that they could not while following the rigid rules of the WHO Ten Steps.
There is a significant amount of emerging research that validates our mothers’ stories. The adverse effects of programs like the BFHI/WHO Ten steps are now under critical review and their consequences are serious and irreversible. As health care professionals, we are ethically and legally obligated to educate parents on how to prevent complications of insufficient breastmilk intake. Failure to meet this obligation can result in serious outcomes that not only put infants and families at risk but also health professionals and hospitals in the form of litigation.
We oppose inaccurate ”fear-mongering” campaigns by lactation professionals, which began in 1996 when lactation consultant Diane Wiessinger wrote an article that was published in the Journal Of Human Lactation called “Watch Your Language! ”
She wrote:
“When we fail to describe the hazards of artificial feeding, we deprive mothers of crucial decision-making information. The mother having difficulty with breastfeeding may not seek help just to achieve a “special bonus”; but she may clamor for help if she knows how much she and her baby stand to lose. She is less likely to use artificial baby milk just ‘to get him used to a bottle’ if she knows that the contents of that bottle cause harm.”
Wiessinger’s goal was to inform parents of the “risks of formula feeding,” and it worked.
Every single parent who contacted us told us they were terrified to supplement their hungry babies, even when medically necessary, because of this message! Some parents refused to supplement, opting for IV glucose, unscreened and untested breast milk, or homemade formula when human milk was unavailable.
Dr. Alison Steube reinforced Wiessinger’s message in 2009 when she wrote a blog for The Academy of Breastfeeding Medicine:
“We need to talk about the “risks of formula feeding” so that we hold policy-makers and health care providers accountable. The “Booby traps” are more than a clever pun: they are a public health problem that’s undermining the health of women and their children.”
But then in 2016, Dr. Steube back-tracked:
She writes:
“I’ve also thought about the risks of risk vs. benefit language when talking with health professionals. Shouldn’t we use breastfeeding as the normative standard in that context? Here, again, I’ve not found a study. It would be ideal to compare a health provider’s motivation to engage with patients after hearing a talk on the “risks of formula” vs the “benefits of breastfeeding.” However, my experience is that in every audience, there are parents, and there are friends and relatives of parents. For many, the topic of infant feeding stirs deep emotions. And when we frame the conversation about “risks of formula,” there’s a real risk that we will trigger negative emotions that will cause those in the audience to shut down, such that they will not be able to hear the evidence-based, clinically applicable messages that could enable their patients to achieve their own infant feeding goals [our emphasis].”
In 2010, Marsha Walker, RN, IBCLC stoked the fear in her article Just One Bottle which was also intended to persuade parents to avoid formula citing risks of formula that are mostly speculative. But the message of this campaign continues to be taught to parents daily.
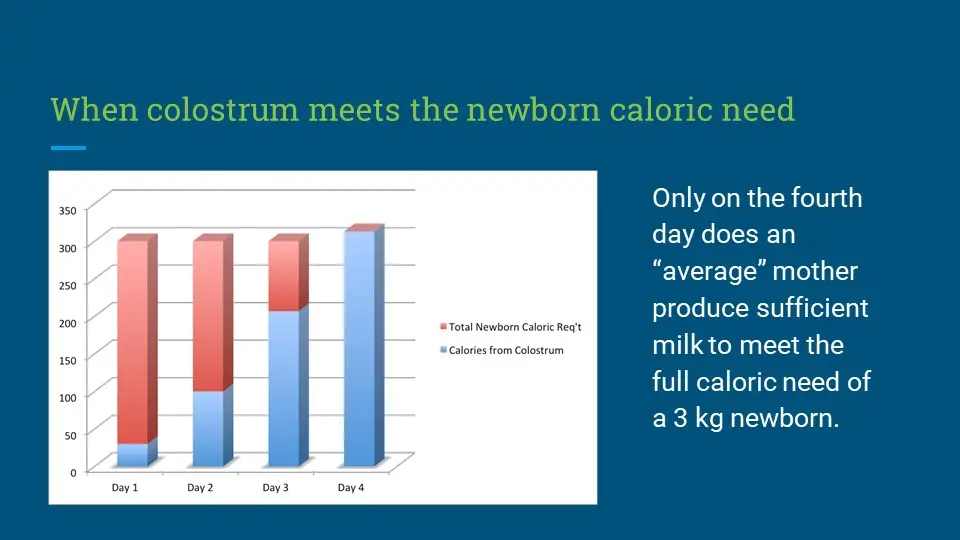
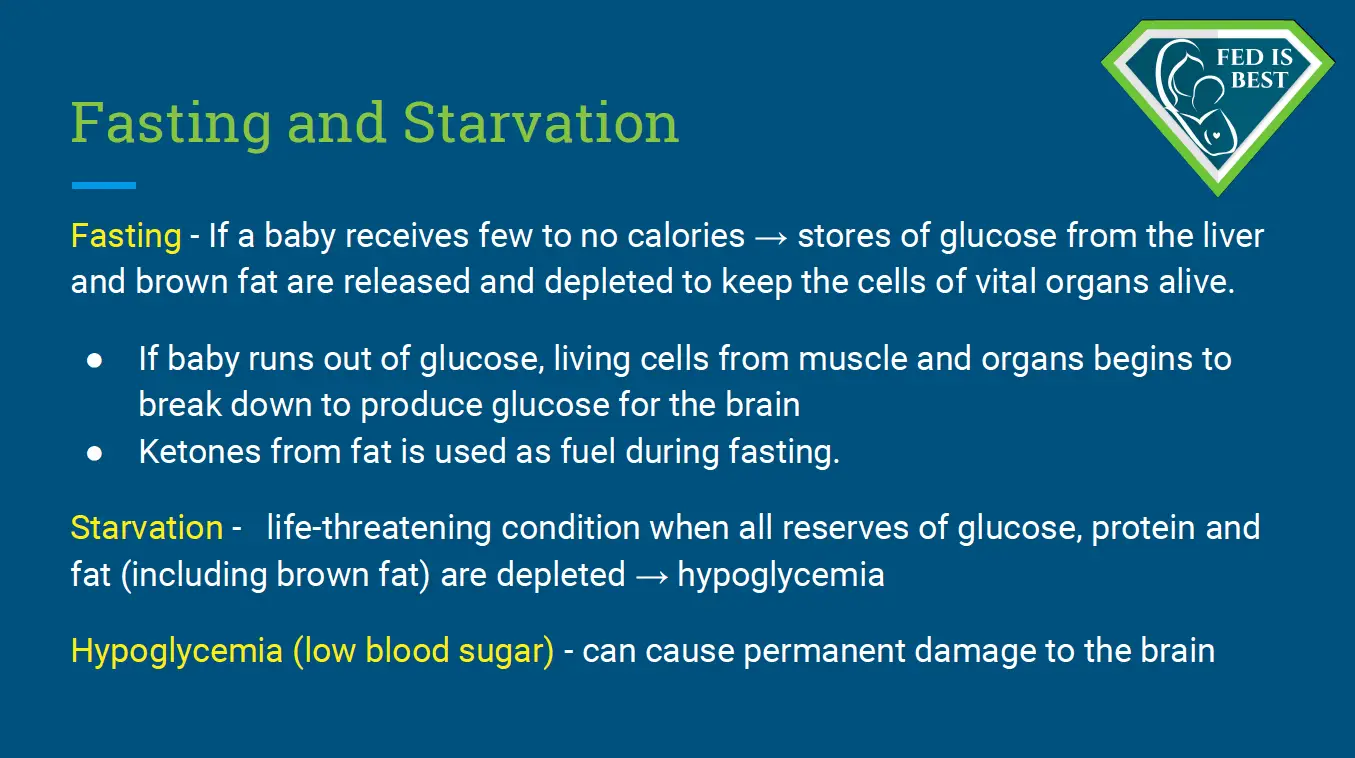
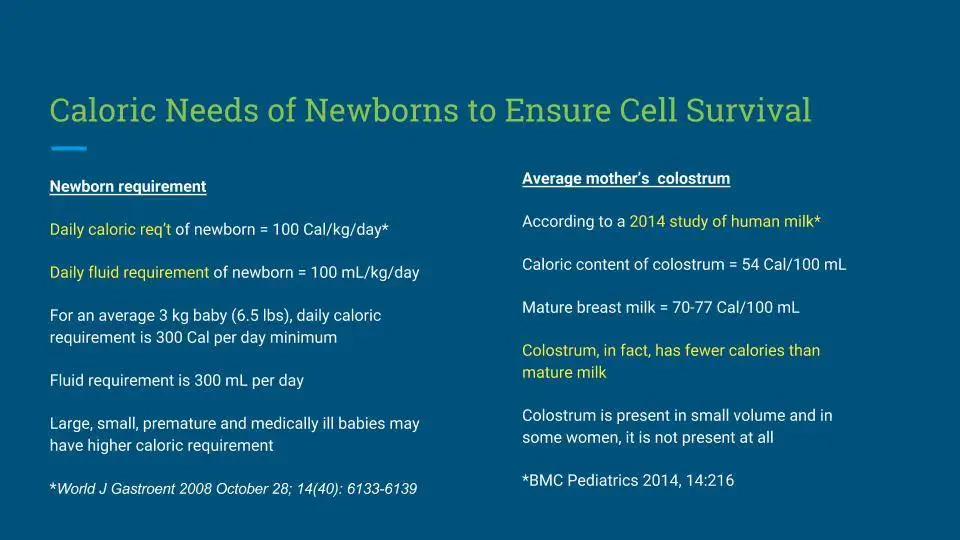
All of these negative campaigns worked. Now we have babies who are admitted routinely for starvation-related hypoglycemia, dehydration and jaundice, some cases resulting in brain injury and rare deaths because parents fear to feed their babies formula.
Our ultimate goal should be the goal of every health care professional: to prevent feeding complications and ensure infant safety by informing parents of both the risks and benefits of all their infant feeding choices in an ethical and unbiased fashion. This includes teaching parents that supplementation to prevent hunger and feeding complications can be achieved while ensuring sufficient stimulation to preserve and maximize the breastfeeding relationship.
5. How can you prove you aren’t connected to the formula industry?
We have responded to these accusations by sharing our tax returns as proof. All of the money that we spent to launch our Foundation was from our own personal bank accounts and we continue to use our own money for expenses. We receive modest donations from families and health professionals who believe in the Fed is Best mission and/or have witnessed the harms of aggressive pursuit of exclusive breastfeeding personally and/or professionally. We have also been compensated for assisting in medico-legal cases of infants who have suffered brain injuries from insufficient breastfeeding complications, all the proceeds from which are donated back to the Fed is Best Foundation.
The Fed is Best Foundation, without exception, has not and will not accept any donations from formula- or breastfeeding-affiliated companies or organizations to avoid conflicts of interest. In order to maintain the integrity of the Fed is Best campaign, we routinely monitor for unauthorized use of the “Fed is Best” trademark and send cease-and-desist letters to companies who try to use it to promote their infant feeding products or services.
Ultimately, our organization is an all-volunteer, grassroots organization that includes 1200 parent advocates and over 200 nurses, doctors and allied health professionals who believe in the Fed is Best mission. We are rapidly growing and currently have over 720,000 supporters because of our inclusive and responsible message and because of the passionate support of our volunteer supporters.
https://fedisbest.org/2019/10/faqs-does-the-fed-is-best-foundation-believe-all-exclusively-breastfed-babies-need-supplementation/
THANK YOU FOR YOUR INTEREST IN THE FED IS BEST FOUNDATION!
Our mission statement is:
The Fed is Best Foundation works to identify critical gaps in current breastfeeding protocols, guidelines, and education programs. We provide families and health professionals with the most up-to-date scientific research, education, and resources to practice safe infant feeding with breast milk, formula, or a combination of both. To be fully informed, parents must be taught about the risks of insufficient breast milk intake while supporting exclusive breastfeeding in order to eliminate preventable hospitalizations for insufficient feeding complications. Finally, we strive to eliminate infant feeding shaming while prioritizing perinatal mental health.
HOW YOU CAN SUPPORT FED IS BEST
There are many ways you can support the mission of the Fed is Best Foundation. Please consider contributing in the following ways:
- Join us in any of the Fed is Best volunteer and advocacy, groups. We currently have– Health Care Professional Advocacy Group, Advocacy Group, Research Group, Volunteer Group, Editing Group, Social Media Group, Legal Group, Marketing Group, Maternal Mental Health Advocacy Group, Private Infant Feeding Support Group, Global Advocacy Group, and Fundraising Group. Please send an email to Jody@fedisbest.org– if you are interested in joining any of our volunteer groups. For our health professional advocacy group, join us here.
- If you need infant feeding and parenting support, we have a support group– Join us here.
- Make a donation to the Fed is Best Foundation. We are using funds from donations to cover the cost of our website, our social media ads, our printing and mailing costs to reach health providers and hospitals. We do not accept donations from breast- or formula-feeding companies and 100% of your donations go toward these operational costs. All the work of the Foundation is achieved via the pro bono and volunteer work of its supporters.
- Sign our petition! Help us reach our policymakers, and drive change at a global level. Help us stand up for the lives of millions of infants who deserve a fighting chance. Sign the Fed is Best Petition at Change.org today, and share it with others.
- Share the stories and the message of the Fed is Best Foundation through word-of-mouth, by posting on your social media page and by sending our FREE infant feeding educational resources to expectant moms that you know. Share the Fed is Best campaign letter with everyone you know.
- Write a letter to your health providers and hospitals about the Fed is Best Foundation. Write to them about feeding complications your child may have experienced.
- Print out our letter to obstetric providers and mail them to your local obstetricians, midwives, family practitioners who provide obstetric care and hospitals.
- Write your local elected officials about what is happening to newborn babies in hospitals and ask for legal protection of newborn babies from underfeeding and of mother’s rights to honest informed consent on the risks of insufficient feeding of breastfed babies.
- Send us your stories. Share with us your successes, your struggles and everything in between. Every story saves another child from experiencing the same and teaches another mom how to safely feed her baby. Every voice contributes to change.
- Send us messages of support. We work every single day to make infant feeding safe and supportive of every mother and child. Your messages of support keep us all going.
- Shop at Amazon Smile and Amazon donates to Fed Is Best Foundation.
Or simply send us a message to find out how you can help make a difference with new ideas!
For any urgent messages or questions about infant feeding, please do not leave a message on this page as it will not get to us immediately. Instead, please email christie@fedisbest.org.
Thank you and we look forward to hearing from you!

Health Care Professionals Advocacy Group