Dear Obstetrician-Gynecologist, Family Practitioner or Midwife,
I am writing to you as a mother and advocate for Fed is Best.
You may have seen the story of Landon Johnson, who was welcomed into the world by his parents in February 2012. Like most new parents, Landon’s mom and dad were lead to believe that Jillian would produce enough breast milk to meet Landon’s caloric needs. The hospital where they delivered was “Baby-Friendly” and would only provide formula with a doctor’s prescription.
While in the hospital, Landon cried whenever he was not latched onto his mom’s breast. Jillian described him as inconsolable. She was told that this was normal. At less than 3 days of life they were discharged from the hospital after having the appropriate number of wet and dirty diapers. However, less than 12 hours later, Landon was readmitted to hospital after suffering cardiac arrest due to severe dehydration. He suffered brain injury and ultimately died in the arms of his parents when life support was terminated. His is a story that you cannot read without tears in your eyes.
Because of the Fed is Best Foundation, I learned about the risk of accidental newborn starvation and my husband and I were able to come up with a plan to reduce the possibility of any adverse health outcomes while we waited for my milk to come in. Almost 5 years to the day of Landon’s birth, on February 22, 2017 we welcomed our daughter to the world. After every nursing session, my husband offered a bottle of formula. In this manner, we were able to minimize her weight loss. Interestingly, she did not go through the “second night” of crying that we were warned about. In fact, she rarely cried but instead ate and slept, no doubt because she had a full tummy from our supplementing efforts. She remains, to this day, a happy breastfed baby.
The goal of the Fed is Best Foundation is to ensure that no newborn suffers complications while they wait for mother’s milk to come in. Landon’s parents tell the story about how just one bottle could have saved him and that is the message that the Fed is Best Foundation wants to spread: that just one bottle can protect a newborn from potentially serious consequences from being underfed. Jillian Johnson and Dr. Christie del Castillo-Hegyi, Co-Founder of the Fed is Best Foundation, recently spoke about Landon’s story and the importance of being aware of the signs of accidental infant starvation on the Doctors Show.
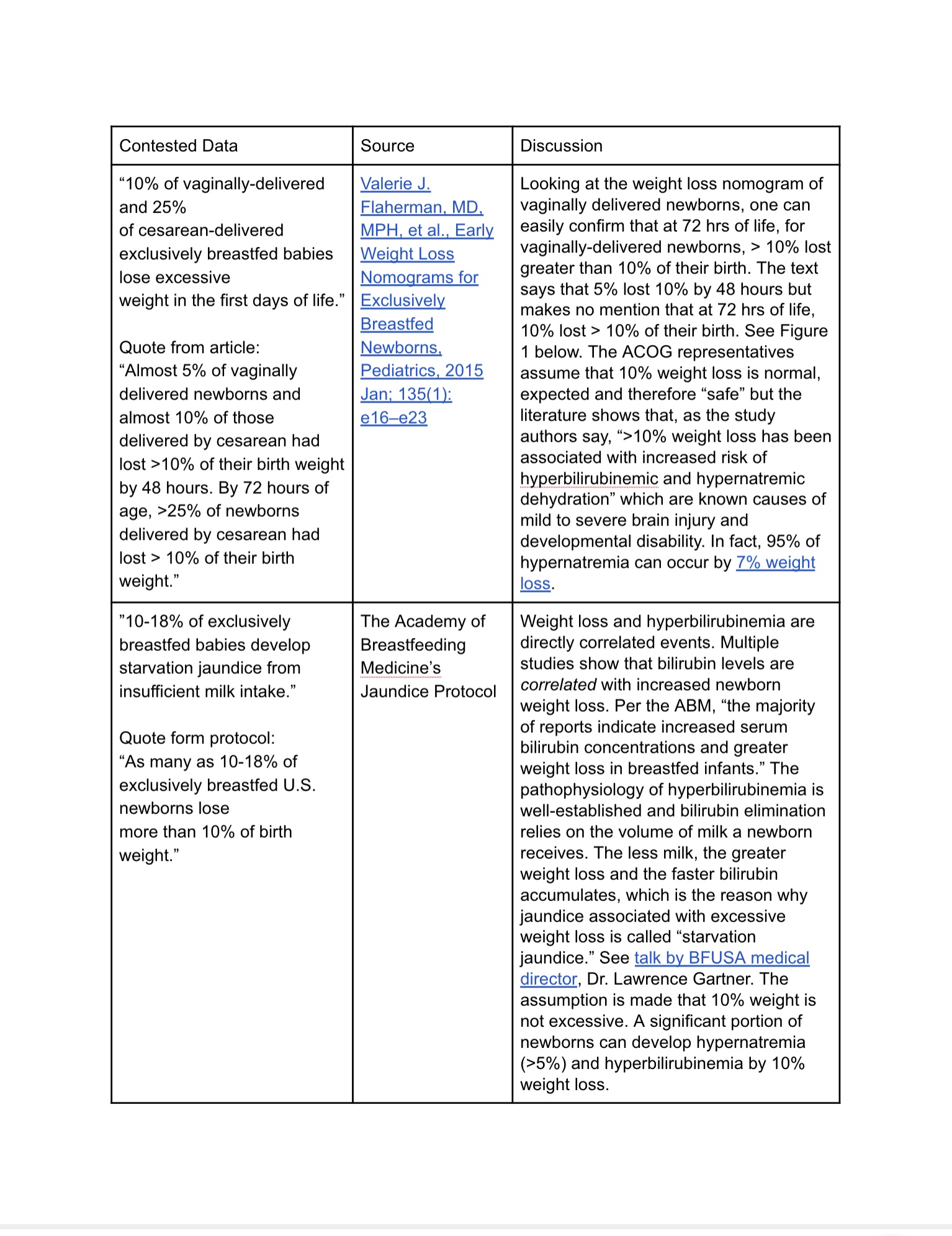
According to peer-reviewed literature on breastfeeding complications as collected by the Fed is Best Foundation.
- 10% of vaginally-delivered and 25% of cesarean-delivered exclusively breastfed (EBF) babies lose excessive weight in the first days of life.[i]
- 12-35% of well-monitored EBF newborns develop hyperbilirubinemia and 5.7% of newborns born in hospitals with high exclusive breastfeeding rates require phototherapy,the majority caused by excessive weight loss and insufficient feeding.[ii]
- 10% of well-monitored exclusively breastfed babies undergoing the World Health Organization’s Baby-Friendly Hospital Initiative protocol develop hypoglycemia of less the 40 mg/dL within the first 48 hours. This incidence is reported as 23% in babies born to first-time mothers.[iii] These levels of hypoglycemia are low enough to cause long-term cognitive impairment. [iv]
- In a study of 280 mother-baby dyads, 22% of motivated mothers intending to exclusively breastfeed who received close lactation support experienced delayed onset of copious milk production which put her child at a 7-fold increased risk of excessive weight loss greater than 10%. This means more than 1 in 5 newborns are at risk of starvation-related complications if exclusively breastfed from birth.[v]
- A glucose of less than 46 mg/dL within the first 24 hours of life has been associated with a 3.7-fold increased risk of brain injury on MRI and a 4.8-fold increased odds of lower motor, cognitive and language scores at 1 year of age.[vi]
- Cognitive impairment can have life-long effects as evidenced by a study of 1395 newborns showing that newborns who develop transient hypoglycemia of less than 40 mg/dL had a 50% reduction in passing their fourth-grade proficiency test in literacy and math. Even a glucose less than 45 mg/dL resulted in a 38% reduction in passing the literacy test.[iv]
- The current standard of care tolerates a glucose between 40 and 45 mg/dL within the first 4 hours of life when there is no evidence that neurons have greater tolerance for hypoglycemia in the first hours than they do at any other time.[vii]
- Exclusive breastfeeding at discharge has been associated with an 11-fold higher risk of rehospitalization for underfeeding and dehydration.[ix]
The Fed is Best Foundation would like to offer you printed materials to make available to your patients so that they can learn about the potential negative health consequences of underfeeding and how to prevent feeding complications through the Fed is Best Foundation parent resource page (fedisbest.org/resources). If you are interested in helping your patients learn how to best feed their babies safely, through breastfeeding, formula-feeding or any combination of both, please consider counseling them on the importance of prioritizing the health and safety of their babies through adequate feeding and please email the Fed is Best Foundation with your mailing address at contact@fedisbest.org to receive our educational material.
Sincerely,
Alicia Bayley
Mother and Fed is Best Advocate
To members of acog in response to the recent editorial published about the Fed is Best foundation:
Dear Colleague,
When patients speak by the thousands regarding serious harm caused to their infants, our duty to our patients is to stop and critically evaluate our assumptions about the standard of care. As physicians, we have sworn to act in our patients’ best interests, to do no harm and to evaluate the scientific and clinical data to protect our patients’ health and safety above all things. Our organization is responding to the tens of thousands of stories we have received from parents whose children have been hospitalized by the current standards of exclusive breastfeeding education and management. We are responding to the same stories of breastfeeding tragedies shared with us by newborn nurses, general pediatricians and neonatologists. These breastfeeding tragedies occur routinely in every hospital in the country because we have allowed patient education to hide common and serious newborn complications related to exclusive breastfeeding from parents.
We are raising awareness on the harms caused by aggressive promotion of exclusive breastfeeding, which is resulting in an epidemic of newborn hospitalizations for feeding complications, jaundice, dehydration and hypoglycemia, complications that cause mild to severe brain injury and neurodevelopmental disabilities. The incidence of these complications in exclusively breastfed newborns have been published as well as their devastating long-term effects. While we can always say that more research is needed and that confounding data may alter those outcomes, when data is published regarding serious and irreversible harm to patients, the expected response of the medical community is to act conservatively and protect our patients from complications until solid evidence of safety is available regarding those complications. That evidence of safety does not exist for the Baby-Friendly newborn exclusive breastfeeding guidelines. To wait for more data to be published at the expense of harming more children is unacceptable. Since the current breastfeeding guidelines and the guidelines for medical supplementation have never been tested or monitored for safety, in the face of thousands of parents and health professionals reporting serious and irreversible harm from the guidelines, we are obligated to carry out our duty to our patients to warn them of these life and death matters and teach them how to avoid complications.
As much as we would like to believe that these preventable and unacceptable outcomes of exclusive breastfeeding promotion are not happening, they in fact are. There has never been a single issue in medicine where reports of patient harm are ignored and buried. Sadly that is what is happening with regard to exclusive breastfeeding promotion in order to protect those who have written and supported the guidelines who may be held accountable for patients harmed, among whom may be members of the ACOG Breastfeeding Committee who co-authored the editorial. When it comes to exclusive breastfeeding, independent and critical thinking of patient safety issues is discouraged and suppressed. As a result, not only do the guidelines put patients at risk, they put the health professionals who follow them at risk.
100% of breastfeeding tragedies are preventable with honest education on breastfeeding, its complications and indications for emergency parent-led supplementation. When risk factors can be identified in all mothers and when nearly all newborns are showing signs of distress before brain-threatening complications occur, there is no excuse for allowing newborns to be hospitalized for breastfeeding complications. Hiding those risk factors and the serious negative consequences of breastfeeding complications is commonplace in exclusive breastfeeding education. When judicious use of supplementation with safe, tested donor milk or formula can protect a baby’s brain and life without compromising long-term breastfeeding success, it is unethical to hide these interventions from mothers, especially when waiting for permission to supplement can result in serious and irreversible harm.
We hope that our obstetrician colleagues refer to their own clinical experience and their own critical analysis of the data to come to their own conclusions on how to provide the safest and most ethical advice to breastfeeding mothers. We hope that our colleagues listen to mothers whose children have experienced these preventable breastfeeding tragedies as well as their pediatric and neonatology colleagues who are having to correct these complications on a routine basis. The mothers who have shared their deeply painful breastfeeding stories on the Fed is Best website are disappointed with ACOG for suggesting that their stories are not real or that they have been sensationalized for publicity. These mothers have shared their stories in order to prevent the same thing from happening to other babies. They are deeply disappointed that ACOG is choosing to ignore patient and health professional reports and the peer-reviewed published data on serious safety issues associated with the current exclusive breastfeeding protocol.
With regard to the contested data on exclusive breastfeeding complications and their neurological sequelae, please click on the following PDF:
For those who wish to learn more about safe breastfeeding promotion and would like to join our health professional group, please contact us at contact@fedisbest.org.
Sincerely,
Christie del Castillo-Hegyi, M.D. and Jody Segrave-Daly, RN, IBCLC
Co-Founders of the Fed is Best Foundation
Update: Response from Dr. Christopher Zahn, ACOG Vice President
Thank you to the American College of Obstetricians and Gynecologists for Supporting All Mothers and Their Infants
To the Leadership of the American College of Obstetricians and Gynecologists:
We want to thank Dr. Christopher Zahn, Vice President of Practice Activities for the American College of Obstetricians and Gynecologists for responding to our letter regarding safe support of breastfeeding in the newborn period and inclusive support of all mother’s informed infant feeding choices.
We thank you for endorsing that Obstetrician-Gynecologists and midwives provide counseling on when a mother should seek help regarding breastfeeding problems. We are encouraged by your support of providers maintaining knowledge and skills on normal breastfeeding physiology and management of breastfeeding complications, including anticipatory pre-hospital discharge feeding guidance for mothers on those matters. We, too, feel that providing mothers the tools to recognize safe and unsafe conditions in their infants during the course of breastfeeding is critical to providing safe and ethical breastfeeding support. Most of all, we are so grateful for ACOG’s recommendation that Obstetrician-Gynecologists and other obstetric care providers support each woman’s informed decision about what form of infant feeding is best for her child, whether it be exclusive breastfeeding, mixed feeding or formula feeding. We, too, believe that mothers are uniquely qualified to determine what optimal nutrition looks like for her child depending on breast milk supply, anatomy, infant nutritional needs and the complex social, psychological and economic realities of the family unit.
Thank you for your continued support of mothers and their infants as well as the health providers that care for them.
Sincerely,
Christie del Castillo-Hegyi, MD and Jody Segrave-Daly, RN, IBCLC, Co-Founders and The Fed is Best Foundation
Note: We are offering U.S. health care providers printed business cards, postcards and brochures sent by mail for free while supplies last. You may opt to donate the shipping and printing costs or any amount to help support the educational outreach efforts of the Fed is Best Foundation. We are also offering this printed material all over the world at the cost of printing and shipping through VistaPrint, an international shipping company. You may also choose to print out your own promotional material for your patients by clicking on the downloadable material below. Please contact us at contact@fedisbest.org. Thank you so much for your support.
If You would like to help us reach your local OBstetrician-Gynecologist, Family Practitioner or General Practitioner, Please Print Out this Letter and Send it to them:
Letter to Obstetrics Providers
Please download the full health provider packet to see the educational material offered to mothers through fedisbest.org
Fed is Best Foundation Postcards
Fed is Best Foundation Business Cards
[i] Valerie J. Flaherman, MD, MPH, et al., Early Weight Loss Nomograms for Exclusively Breastfed Newborns, Pediatrics, 2015 Jan; 135(1): e16–e23.
[ii] ABM Clinical Protocol #22: Guidelines for Management of Jaundice in the Breastfeeding Infant Equal to or Greater Than 35 Weeks’ Gestation, The Academy of Breastfeeding Medicine Protocol Committee, Breastfeeding Medicine, Vol. 5(2):87-93.
[iii] Purnima Samayam, et al., Study of Asymptomatic Hypoglycemia in Full Term Exclusively Breastfed Neonates in First 48 Hours of Life, J Clin Diagn Res. 2015 Sep; 9(9): SC07–SC10.
[iv] Kaiser, J.R., et al., Association Between Transient Newborn Hypoglycemia and Fourth-Grade Achievement Test Proficiency: A Population-Based Study. 2015 JAMA Pediatr 169, 913–921.
[v] Dewey KG, et al., Risk factors for suboptimal infant breastfeeding behavior, delayed onset of lactation, and excess neonatal weight loss, Pediatrics, 2003 Sep;112(3 Pt 1):607-19.
[vi] Emily W.Y. Tam et al., Hypoglycemia is associated with increased risk for brain injury and adverse neurodevelopmental outcome in neonates at risk for encephalopathy, J Pediatr., 2012 Jul; 161(1): 88–93.
[vii] Postnatal Glucose Homeostasis in Late-Preterm and Term Infants, Committee on Fetus and Newborn, Pediatrics, 2011;127:575–579.
[ix] Escobar GJ, et al., Rehospitalization for neonatal dehydration: a nested case-control study, Arch Pediatr Adolesc Med., 2002 Feb;156(2):155-61.




THat is a beautifully written and succinct letter. Thank you.
Thank you! Pass it on to your local OBs!
Hi greetings from Singapore! I just want to say thank you so much for your website and for the valuable information shared. The stories were really heartbreaking. Your website really hit the nail on the head. Like you, while I believe that breastfeeding is good for baby and mum, we have gone “too far” the other way and many mums view formula akin to poison for their babies. Motherhood is so much more than just breastfeeding but somehow that seems to be the only thing people focus on. I never knew the medical implications that could result on the insistence to exclusively breastfeed especially in the early days, which further drives home the point that we’ve somehow turned something good (education on the benefits of breastfeeding) to ugly ( babies suffering needlessly, mothers made to feel like failures) I agree that the societal/media pressure new mums feel to breastfeed is really awful and it even starts almost from day1 after giving birth in the hospital. I too experienced first hand the guilt tripping at the hospital. However I say this only after the experience and insights gained having 3 kids (youngest now being 9 weeks old) . I can definitely identify with these same feelings many of the mums interviewed talked about. Lastly, for perspective, of the 3 children we have, #2 was solely on formula and so far she’s much healthier and robust than #1 who was breastfed! So a lot I think still depends on the child’s own body makeup. Breastmilk is good but fed is best. Thanks again!!
Thank you so much Joanne for sharing your story and for supporting the Fed is Best message! In nature, the fed babies are the healthiest. Even one episode of starvation can compromise the long-term health and brain-development of a child. We hope we can change how mothers are taught to feed their children. Fed is best.
You doing the best and useful job on this topic. I am very impressed with your site and also I like your information. I got the best posts they amazing. Thanks for sharing the best information it very help us.