Dear Colleague and Parent:
My name is Christie del Castillo-Hegyi and I am an emergency physician, former NIH scientist, with a background in newborn brain injury research at Brown University, and mother to a 6-year-old child who is neurologically disabled. I am writing to you because my child fell victim to newborn jaundice, hypoglycemia and severe dehydration due to insufficient milk intake from exclusive breastfeeding in the first days of life. As an expectant mom, I read all the guidelines on breastfeeding my first-born child. Unfortunately, following the guidelines and our pediatrician’s advice resulted in my child going 4 days with absolutely no milk intake requiring ICU care. He was subsequently diagnosed with multiple neurodevelopmental disabilities. Being a physician and scientist, I sought out peer-reviewed journals to explain why this happened. I found that there is ample evidence showing the links between neonatal jaundice, dehydration, hypoglycemia, and developmental disabilities. I wish to explain to you how I believe this could apply to my son and the many children whose care you are entrusted with.
I was an attending physician in the hospital where my son was born at Downtown Presbyterian Hospital in Albuquerque, New Mexico. My son was born 8 pounds and 11 ounces after a healthy pregnancy and normal uneventful vaginal delivery. He was placed directly on my chest and was nursed immediately. He was nursed on demand for 20-30 minutes every 3 hours. Each day of our stay in the hospital, he was seen by the pediatrician as well as the lactation consultant who noted that he had a perfect latch. He produced the expected number of wet and dirty diapers. He was noted to be jaundiced by the second day of life and had a transcutaneous bilirubin of 8.9. We were discharged at 48 hours at 5% weight loss with next-day follow-up. We were told by the lactation consultant before discharge that he would be hungry and we were instructed to just keep putting him on the breast. Upon getting home, he became fussy and I nursed him longer and longer into the night. He cried even after nursing and latched back on immediately. He did not sleep. By the next morning, he stopped crying and was quiet. We saw our pediatrician at around 68 hours of life (end of day 3). Despite producing the expected number of wet and dirty diapers, he had lost 1 pound 5 ounces, about 15% of his birth weight. At the time, we were not aware of and were not told the percentage lost, and having been up all night long trying to feed a hungry baby, we were too exhausted to figure out that this was an incredible amount of weight loss. He was jaundiced but no bilirubin was checked. Our pediatrician told us that we had the option of either feeding formula or waiting for my milk to come in at day 4 or 5 of life. Wanting badly to succeed in breastfeeding him, we went another day unsuccessfully breastfeeding and went to a lactation consultant the next day who weighed his feeding and discovered that he was getting absolutely no milk. When I pumped and manually expressed, I realized I produced nothing. I imagined the four days of torture he experienced and how 2 days of near-continuous breastfeeding encouraged by breastfeeding manuals was a sign of this. We fed him formula after that visit and he finally fell asleep. Three hours later, we found him unresponsive. We squeezed a few milliliters of formula milk into his mouth, which made him more alert, but then he seized. We rushed him to the emergency room. He had a barely normal glucose (50 mg/dL), a severe form of dehydration called hypernatremia (157 mEq/L), and severe jaundice (bilirubin 24 mg/dL). We were reassured that he would be fine, but having done newborn brain injury research, knowing how little time it takes for brain cells to die due to hypoglycemia and severe dehydration, I did not believe it, although I hoped it.

Born healthy, full-term weighing 8 pounds 11 ounces getting skin-to-skin and immediate breastfeeding after birth

The third day of life after the pediatrician visit. He was no longer crying and he was jaundiced and dehydrated with 15% weight loss. We were reassured that we could keep exclusively breastfeeding.

Hypernatremic dehydration and encephalopathy from brain injury. Blank staring is a hallmark of newborn brain injury.
Watch the Doctors Show Interview
At 3 years and 8 months, our son was diagnosed with severe language impairment, autism, ADHD, sensory processing disorder, low IQ, fine and gross motor delays. He was later diagnosed with a seizure disorder associated with injury to the language area of the brain. Since my child’s diagnosis, I have been researching the scientific literature on breastfeeding insufficiency, newborn starvation, brain injury, and developmental disabilities for over three years. In addition, I have collected similar breastfeeding stories of tens of thousands of women through social media.
In the September 2015 issue of Hospital Pediatrics, an article was published describing 11 exclusively breastfed newborn babies who developed profound hypoglycemia between the second and fifth days of life from insufficient breast milk intake. The child described in the body of the article was a healthy full-term baby who presented just like my son. He was seen on the third day of life at his pediatrician’s office. Despite that, he was found on the fourth day of life lethargic and unable to feed. He had lost 10% of his birth weight and had a low glucose of 20 mg/dL (normal > 47 mg/dL). This child was given IV glucose after which he developed a seizure. They obtained a brain MRI which showed extensive areas of injury to almost the entire brain. In addition to this child, 10 other healthy term newborns were identified to have developed hypoglycemia from insufficient breastfeeding as well. They were found lethargic, seizing, hypothermic and/or not breathing. 5 out of the 6 MRIs obtained in these babies showed widespread injury to a third to almost the entire brain in varying patterns. They subsequently developed long-term neurological disabilities including seizure disorders, motor weakness, visual impairment and feeding difficulties requiring speech therapy.
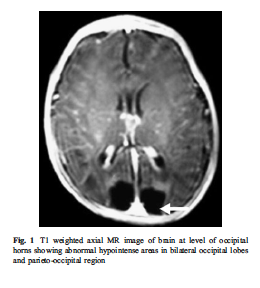
The brain MRI of an exclusively breastfed baby who developed lethargy and hypoglycemia (20 mg/dL) by day 3 of life from insufficient breast milk intake. The dark areas in the posterior part of the brain are the areas of missing brain tissue that resulted one month after the episode of hypoglycemia.
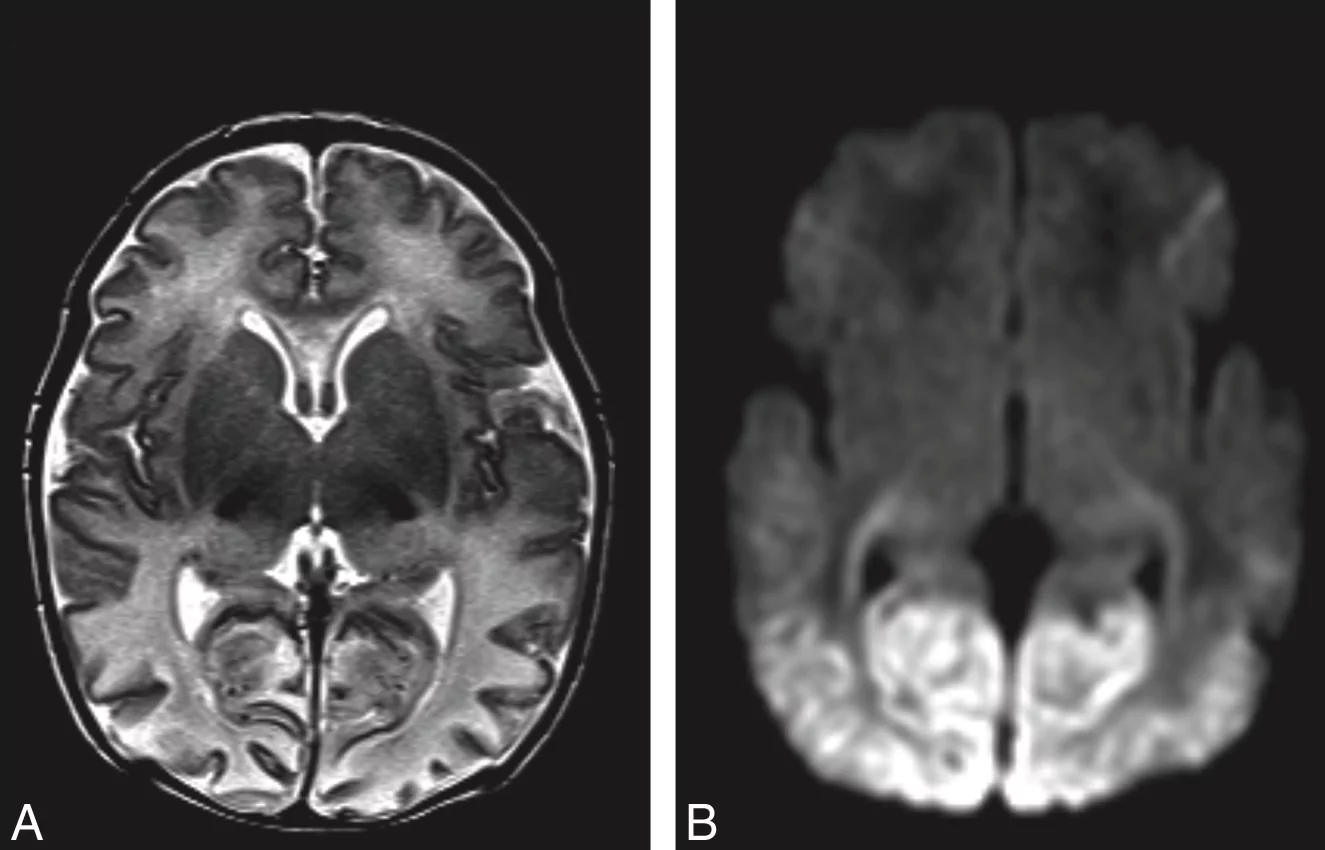
Brain MRI of acute hypoglycemic brain injury. The light appearance in the posterior part of the brain is swelling and injury caused by caloric deprivation to brain cells due to hypoglycemia.
The answer to the epidemic of developmental disabilities we are seeing may be found in this vulnerable period. The risk factors for neurological disabilities in children all have to do with brain injury caused by excessive jaundice, loss of oxygen, circulation, and glucose delivery to the brain. These include pre-eclampsia, intrauterine growth retardation, and prematurity, which are caused by poor function of the placenta and decreased circulation to the baby. Hypoglycemia, umbilical cord prolapse, nuchal cord (cord wrapped around the neck), fetal distress, low Apgar scores, respiratory distress, and other labor complications, events that all cause perinatal brain injury also cause long-term neurological disabilities. Although there are many causes of newborn brain injury that we have no control over, we have control over whether or not a child is fed enough for all their brain cells to survive. I believe we may be inducing hypoglycemic brain injury to many newborns by asking mothers who may not be producing sufficient milk for their newborn’s physiologic need to exclusively breastfeed. We are potentially putting ourselves at odds with the protective natural instinct to respond to a baby’s cry by telling mothers that their colostrum is enough (which for many it may not be) and by making them fear failure by giving their child supplementation when they need it.
My child’s story is not rare. In a study of 280 mother-baby dyads, 22% of motivated mothers intending to exclusively breastfeed who received close lactation support experienced delayed onset of copious milk production, or lactogenesis II, which put her child at 7-fold increased risk of excessive weight loss greater than 10%. This means more than 1 in 5 newborns are at risk of excessive weight loss and the associated complications if exclusively breastfed from birth. In another study, it has been found that 10% of well-monitored exclusively breastfed babies undergoing the Baby-Friendly Hospital Initiative protocol develop hypoglycemia of less than 40 mg/dL within the first 48 hours. This incidence was even higher in babies born to first-time mothers as 23% developed hypoglycemia. This level of hypoglycemia has been shown in other studies to result in brain injury on MRI and long-term declines in cognitive function. One study showed that a glucose of less than 46 mg/dL within the first 24 hours of life was associated with a 3.7-fold increased risk of brain injury on MRI and a 4.8-fold increased odds of lower motor, cognitive and language scores at 1 year of age. This cognitive impairment persists as evidenced by another study of 1395 newborns showing that newborns who develop transient hypoglycemia of less than 40 mg/dL had a 50% reduction in passing their fourth-grade proficiency test in literacy and math. Even glucose less than 45 mg/dL resulted in a 38% reduction in passing the literacy test. The current standard of care tolerates a glucose between 25 and 45 mg/dL when there is evidence that those levels of hypoglycemia result in long-term lower academic achievement and developmental disability.
I hope you feel the same sense of urgency that I do. Since we received our diagnosis, I have come to personally know 43 mothers whose children experience starvation-related complications from exclusive breastfeeding, including pediatricians, other doctors, nurses and lactation consultants. All of them have children with long-term neurodevelopmental impairments. While the literature cites poor education in breastfeeding as the cause of these starvation-related complications, in my research of breastfeeding mothers, it is the most educated in breastfeeding that are at the highest risk. The least educated will respond to a baby’s cry by offering a bottle. The mothers that are most educated in breastfeeding are the ones who have been taught that offering just one bottle will ruin her breastfeeding and potentially harm her child. I have learned that this is a distortion of reality created by breastfeeding education to pressure mothers to exclusively breastfeed that can put her child’s life at risk.
I am writing to let you know I believe the current newborn exclusive breastfeeding guidelines of the Baby-Friendly Hospital Initiative are dangerous. My son suffered an incredible amount of weight loss by the third day, which is often when mothers produce milk. How many newborns are experiencing this same fate? To date, there are no rigorously done studies on the safety of newborn weight loss and exclusive breastfeeding before lactogenesis II on the newborn brain. In fact, a study has shown that exclusive breastfeeding at discharge is associated with an 11-fold higher risk of rehospitalization for underfeeding and dehydration, which few parents are informed of.
I would like to advocate for a patient safety initiative to increase monitoring and supplementation to prevent adverse neurologic conditions in all exclusively breastfed newborns as described by the following:
1) Mothers should be instructed on how to manually express to confirm the presence of milk, which is available through this link. Any baby whose mother has little to no colostrum should be offered supplementation immediately.
2) Twice daily weighing for exclusively breastfed newborns in the hospital and at home as it has been shown that the least-fed newborns can lose the maximum recommended weight loss of 7% within the first 24 hours. This practice should be continued at home until breastfeeding meets the child’s full metabolic requirement as signaled by the onset of daily weight gain. The 7% weight loss threshold should be provided to the mother to help signal the need for supplementation in the hospital and at home.
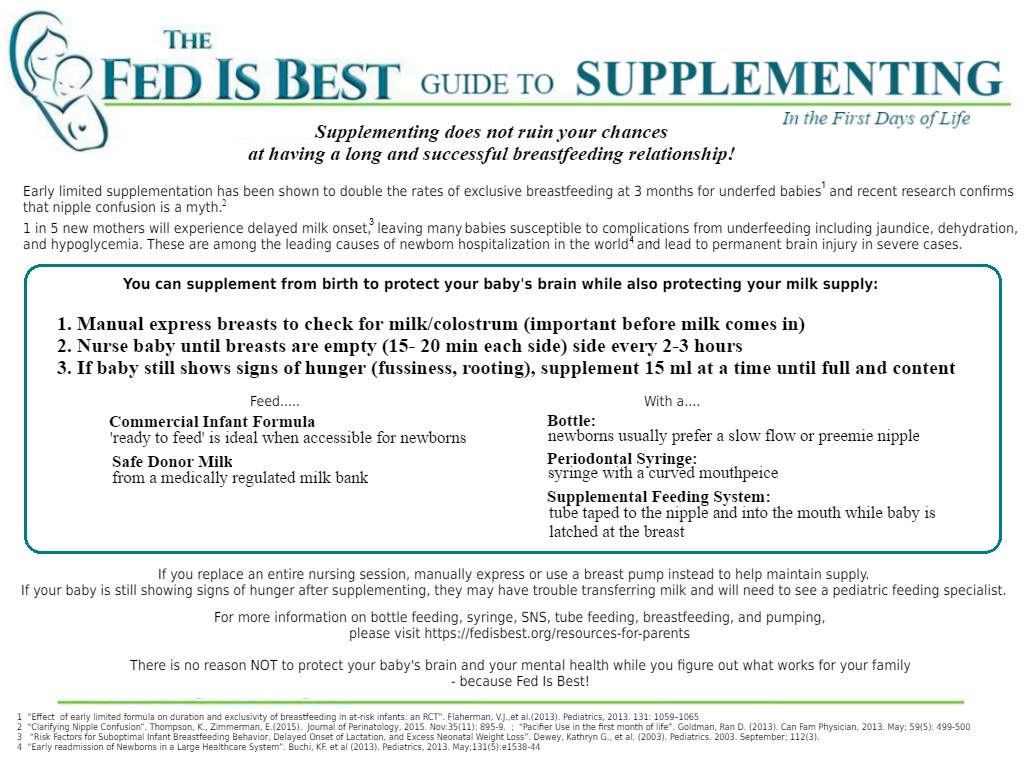
3) Universal daily transcutaneous bilirubin checks and glucose monitoring while in the hospital for exclusively breastfed newborns before the onset of daily weight gain as the scientific literature has now identified them as a high-risk population for hypoglycemia. The physical exam is insufficient to rule out hypoglycemia and pathological hyperbilirubinemia. Any inconsolable child should also have a glucose check as this is an often-missed sign of hypoglycemia. Supplementation with breast milk or formula as well as IV glucose should be given immediately at a glucose level less than 47 mg/dL as this is the only prospectively validated glucose threshold that if corrected immediately prevents the development of developmental delay. Supplementation should also be offered for bilirubin levels exceeding 15 mg/dL or any level considered high risk on the bilirubin nomogram. Not only does supplementation for underfed newborns protect a child’s brain and stabilize glucose but it also doubles the rates of exclusive breastfeeding at 3 months.
4) Pre- and post-breastfeeding weights after lactogenesis II to measure the amount of milk transferred to the baby. The caloric requirement of a newborn baby is 100-120 kcal/kg/day and a mother’s production should be around 2.7 oz/lb/day or 6 oz/kg/day (roughly 2 ounces per feed every 3 hours) to sustain a newborn and prevent feeding complications. Some babies with medical conditions may need more than the above volumes.
5) Next day after discharge follow-up with pediatricians and lactation consultants with universal bilirubin and glucose checks in the office. Children who are crying inconsolably at home especially before lactogenesis II should be supplemented after nursing UNTIL they reach their health care provider in order to prevent the development of hypoglycemia, dehydration and negative neurological consequences.
6) I advocate for mothers to be informed of the possibility that her child can become dehydrated, jaundiced, and hypoglycemic from insufficient breast milk intake and that these conditions can cause developmental and neurological disabilities. Signs of this are a child that is not sleeping or crying repeatedly after breastfeeding as well as nursing near-continuously. Lethargy, poor feeding, seizures, hypothermia (low body temperature), and bradycardia (slow heart rate) are late signs that suggest the presence of profound brain injury from near-complete glucose deprivation to the brain. Lethargic hypoglycemic babies deserve a brain MRI to provide vital information to parents so that they can closely monitor their development and obtain early intervention as needed.
7) Every mother should be educated on supplementation after nursing in order to continue the stimulation needed to promote milk production in case the need for supplementation arises, particularly before discharge if lactogenesis II has not occurred. If a child is hypoglycemic, greater than 7% below the birth weight, hyperbilirubinemia, hypernatremic or crying inconsolably out of hunger, supplementation can be offered 15 MLS at a time as the newborn stomach has been in fact measured to be 20 mL in size at birth, much larger than commonly taught to mothers and health professionals. Supplementation should be offered until a child’s laboratory markers are corrected and the child is no longer in distress. A child’s brain will not wait for food. Once the child is adequately fed, the breastfeeding may then be evaluated to identify the cause of underfeeding. Supplemented breastfeeding is a valid choice as NO BENEFIT of exclusive breastfeeding justifies the risk of life-long disability caused by hypoglycemic brain injury. Any mother sent home before full milk production without a supplementation plan is being sent home to potentially starve and disable her child if her milk does not arrive on time.
Mothers are taught by breastfeeding manuals that they will uniformly be able to produce enough milk for their baby’s needs and will feed them near-continuously for weeks without question if their doctors and lactation consultants tell them not to give formula. But as you have witnessed as a matter of routine, breastfeeding jaundice is very common and mothers do not uniformly produce enough milk for their babies’ needs. The learned wisdom of grandparents who know instinctively the sound of a hungry baby is being supplanted by breastfeeding manuals that cannot teach that sound to the new parent. If you observe non-Western cultures all around the world, babies are given pre-lacteal feeds or milk through wet nurses when mother’s milk is not enough in the first days of life and beyond because instinctively, we as a species protected our newborns by responding to their hungry cry. Thousands of years of evolution have wired mothers to respond to this cry and we are interfering with a biologically protective instinct by telling mothers that their child is getting enough when it is apparent to them that they are not. Babies get admitted to the ICU lethargic, jaundiced and dehydrated every day because their mothers did not know it was possible to have insufficient milk. The most recent publication on hospitalizations for newborn jaundice at a hospital system with high exclusive breastfeeding rates showed that out of 104,468 babies born in a 3 year period, 12.4% of newborns developed excessive jaundice and 5.7% needed hospitalization for phototherapy, the majority of these cases completely preventable with early supplementation. That means millions of babies have been hospitalized since the 1991 publication of the Baby-Friendly Hospital Initiative which codified this protocol. The Baby-Friendly Hospital Initiative and the WHO breastfeeding protocol protects the breastfeeding more than it protects the baby and countless babies have endured days, weeks, and even months of hunger in order to meet its goals.
The time for magical thinking has ended. Breastfeeding education is based on many premises not consistent with reality. Individual health professionals and even mothers have been blamed for accidental infant starvation when in fact, it is the system of breastfeeding education that fails to adequately educate and counsel health professionals and parents on the serious risks of insufficient feeding from exclusive breastfeeding. No time in the history of this planet have we allowed babies to cry out for milk for as long as we tolerate for the purpose of breastfeeding. The first law of nature is and has always been that Fed is Best. Many parents are led to harm their own babies because of what they have been taught about breastfeeding. As you can see, if such a severe case of jaundice and dehydration can occur to two physicians taking home their first-born son, it can happen to anyone.
To all doctors and parents, my message is simple. Feed your baby. Provide your baby its physiologic needs every minute, including the days before milk production. The only person who knows what a newborn needs is that newborn. The accidental starvation of a newborn child is a tragedy by any definition. We are allowing newborns to receive less than their nutritional requirements and telling parents that they are doing what is best for their children. We must be certain an infant is actually getting fed by every available mean. I hope you join me in informing your colleagues, friends, and family of the data and make changes to your practice. Please feel free to share this letter with whomever you wish.
Respectfully,
Christie del Castillo-Hegyi, MD
christie@fedisbest.org
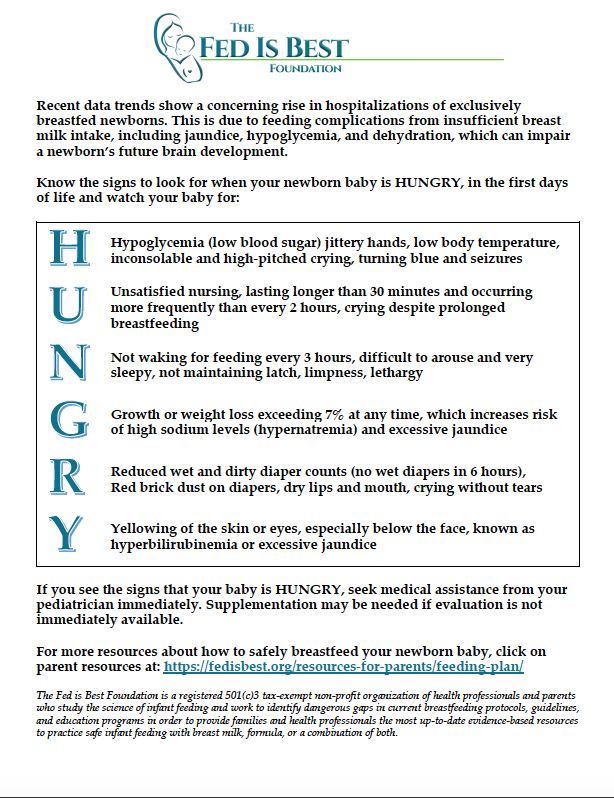
Unfortunately, serious complications occur routinely among newborns who undergo the Baby-Friendly exclusive breastfeeding protocol, namely excessive jaundice, excessive weight loss, dehydration, hypernatremia and hypoglycemia. We would like to help your family protect your baby’s future.
Read the Stories of Thousands of Families, Nurses and Physicians Who Signed the Fed is Best Petition
If I Had Given Him Just One Bottle, He Would Still Be Alive.
Hospital Drops Baby Friendly Program After Doctors Baby Was Harmed
Two Physicians Describe How Their Baby-Friendly Hospital Put Their Newborn in Danger
Jillian Johnson: My Message To Parents During World Breastfeeding Week-Just One Bottle
NICU Nurse Discloses Newborn Admission Rates From Breastfeeding Complications in BFHI Unit
Nurses Are Speaking Out About The Dangers Of The Baby-Friendly Health Initiative
Neonatal Nurse Practitioner Speaks Out About The Dangerous Practices Of The BFHI
Information for Hospitals: Ensuring Safety for Breastfed Newborns
Fed is Best Statement to the USDA Regarding the Harms of the Baby-Friendly Hospital Initiative
Dangers of Insufficient Exclusive Breastfeeding Grand Rounds Presentation
National Women’s Health Advocate Describes How A Baby-Friendly Hospital Starved Her Baby
Nurses Quit Because Of Horrific Experiences Working In Baby-Friendly Hospitals
How To Prepare For Supplementing When Breastfeeding Your Baby In The Hospital
To learn more about the Fed is Best Foundation, please go to our About page.
Disclaimer: This document does not replace in-person physician evaluation and treatment. This document is meant to inform parents of the most recent data regarding infant feeding and to increase their knowledge on how to protect their newborns from hyperbilirubinemia, dehydration, hypernatremia, hypoglycemia and extended or repeat hospitalizations due to complications from underfeeding. Earlier supplementation may be needed for babies who are premature or have medical conditions. It is recommended that a parent seeks evaluation by a pediatrician for any concerns regarding the health and safety of her baby if they arise.


Thank you so much for sharing this article. you details information share that help me and others people. some women feel problems low milk supply and more. its post help their .
Thanks ..
Thank you so much for drawing mine and others attention to such an important matter. Being a postpartum nurse for 8 years I thought I was perfectly well trained and educated in the “art” of breastfeeding, but the more I examine your site, I realize I’ve been fed the same lines as many of the other commenters without adequate evidence. “Cluster feeding is normal” “second night syndrome is to be expected” “just because there’s nothing being hand expressed its okay, only 2% of moms can’t produce milk” “look at how much the baby is peeing and pooing, it’s obviously fine – that’s why it’s lost so much weight” With our hospital heading towards BFI certification, I definitely want to look more into these issues and armed with some peer-reviewed journals I may have to sit down with my manager and educator.
nice article for you, i very happy in here your web. Regards success always for you.
hammer of thor
hammer of thor testimoni
ciri ciri hammer of thor asli
I love what you are doing. I have a family history filled with low milk production. My sister is trying to exclusively breastfeed her first baby who is losing weight in her second week of life. My sister is afraid to bottle feed, and I think it’s insane what our society has done to new moms!
My 9lb 6oz (at birth) baby was routinely checked for low blood sugar and when he dipped out of the normal range my night nurse told me I could offer a bottle or he would be sent to the nicu to keep with hospital policy. Of course I offered the bottle and his blood sugar levels shot up to a healthy range. The next morning another nurse told me that if it had been her, she would have turned a blind eye to the low blood sugar – confident that it would have gone up on its own. I was grateful even then that I had given my baby a bottle. (I continued to primarily breastfeed him for the next 11 months.) In retrospect I find the second nurse’s attitude appalling, yet I imagine it is pervasive. Guidelines and policies are ignored in the name of breastfeeding. Stop the bottle-shaming people!!!
One place where the bottle-shaming attitude does not seem to exist is in the NICU. I was there with my third child and all his nurses were just thrilled that he ate two ounces from a bottle. Of course they encouraged and facilitated nursing, but they want to make sure the baby is healthy. Why can’t this attitude reach over to labor and deliver floors?!
Thanks for all your efforts that you have put in this. very interesting Blog… Thank you for posting this….
Normal-Rent-On-Computer In Delhi
I am so sorry to hear your story. I have 5 kids. My first wouldn’t latch. I wanted to nurse so badly. I tried with my 2nd, but she needed a nipple shield, lost a little weight, fed all the time, and I didn’t have enough support. Third one came along. I was determined to breastfeed. She struggled with jaundice. I pumped and gave baby that as well. When baby stopped nursing I knew something wasn’t right. She fed on the bottle fine, but couldn’t breastfeed. She was too fatigue. She was born with two chd. I knew my pediatrian would blow it off and say continue to formula feed. I took her to her cardiologist and she was in heart failure with coarctation of the aorta. Breastfeeding saved my daugter’s life.i wouldn’t have known something wasn’t right without her failure on the breast. I dried up when she was in surgery but she was intolerant to formula and I had to get donor milk for her first year. It was amazing and I’m so happy it made her happy and it was such a blessing from other moms. Baby number 4 was a little slow to gain, but I took herbs to increase supply and did switch feeding. The pain at the breast was so bad. Some feedings I would cry. She was really colicky. I had ppd. But I kept pressing on. Some moms told me he was tongue tied. My doctor said no she’s not. I came back the next appointment with research. This is what the symptoms of tongue tie are, this matches up. I convinced the doctor to clip it. Unfortunately it reattached. I had supply issues at 6 months. I went on domperidone and that saved our breastfeeding relationship. I nursed her for 2.5 years. Last baby I knew we had tongue tie right away. I knew that chompy feeling wasn’t right. I got hooked up with a tongue tie savvy IBCLC and she taught me what effective nursing vs non-nutritive sucking looks like. I feel like if we can educate moms even before they have a baby on what effective nursing looks like, that is more beneficial than telling moms they might be staving their baby’s on their moms milk and formula is just as good. I think education on breastfeeding would be more beneficial then scaring moms that sometimes breast isn’t best. Breast is normal. Sometimes there are medical reasons why a baby can’t transfer, or a mom who can’t produce enough, but getting to the root of the problem is key, instead of putting a band-aid on the problem.
Thank you so much Elisabeth for sharing your story! We are very glad your feeding stories ended in success. We want mothers to be educated on successful breastfeeding as well and we post instructional videos on how to latch effectively, how to pump to increase supply and how to manually express to check for colostrum. However, education on how to breastfeed is not enough. Thousands of babies get hospitalized for brain-threatening complications of underfeeding that cannot be reversed every year and no family deserves to have a child disabled from starvation because they are taught incomplete and half-truths about the realities of breastfeeding. The reality is, there are consequences to not feeding your child enough and pushing a child beyond their physical limit in order to achieve exclusive breastfeeding. Mothers are taught about safe sleep and other child safety issues. They also need to be taught about safe infant feeding. Until babies stop being hospitalized for these complications, we will continue to educate mothers on these complications and how to avoid them.
Cool idea. Thanks. I love your blog! So many great ideas and a breath of fresh air. I used to work in safe sleep and am thus somewhat neurotic when I see pictures of sleeping kids. I noticed that your daughter has long ties on her bonnet. Those can be unsafe for sleeping as kids can get tangled. Just wanted to point this out so your family can stay safe.